The token economy
The token economy system was implemented on the neo-adult unit because the level of negative events there was consistently higher than on other units. Initial attempts to implement the token economy in 1996 were resisted by state advocacy groups due to concerns that the program would be punitive and would fail to provide individualized treatment. To help allay these concerns, the program was required to be voluntary. However, since the program became operational in March 1997, more than 98 percent of the patients admitted to the unit have enrolled in the program. No additional resources or staff were provided for the implementation and maintenance of the token economy.
Staff were trained using both classroom and hands-on training. A substantial percentage of the staff—approximately 25 percent—had previous experience in a token economy system while working with chronic populations or patients with mental retardation. Initially, a majority of the staff were exposed to the specific rules, procedures, and interventions of the program in a day-long classroom session. Staff who were not able to attend the large session were trained in shorter, more intensive sessions that fit unit scheduling.
Classroom training consisted of a review of a manual prepared by the author, question-and-answer sessions, and role playing. After the classroom training, a one-week trial period was conducted on the unit. During this time senior staff, the unit psychologist, and experienced staff provided hands-on instruction for other staff members in the procedures and verbal interventions. During the on-unit training, patients collected tokens but were not required to spend them for privileges. This procedure allowed patients and staff to become comfortable with the procedures. Further mistakes would cause minimal disruption, and patients could build a bank of tokens to spend.
When a patient was admitted to the unit, staff members provided the patient with a token sheet on which tokens in the form of ink-stamps were collected. At that time, staff members explained the rules and procedures. Staff also provided prompts to patients about the rules and the need to collect and use tokens. Lists of the activities that would earn tokens and items for which tokens could be spent were posted on the unit.
The token economy that has been developed on the unit combines unitwide and individual behavior plans. The basic mode of the program is reinforcement of desired behavior. The use of response costs—the loss of tokens for inappropriate behavior—is limited. Patients earn points for engaging in therapeutic activities, groups, assessments, and individually targeted behaviors. Patients also may earn points for keeping their room clean and rising early in the morning. Patients exchange tokens for extra smoke breaks, off-unit grounds passes, television time, movies, trips to snack machines and the canteen, and similar activities.
Access to these reinforcers is limited by a system in which patients progress through several levels based on safety needs. Individuals on close constant observation or 15-minute safety checks are not allowed to purchase extra smoke breaks (five per day are provided for free). Only individuals who reach the highest level are allowed grounds passes.
The only behaviors that require a response cost are violations of major safety rules, such as patients' smoking in their bedrooms, and behaviors that would cause the police to become involved if they occurred outside the hospital, such as hitting someone, threatening someone, and destroying property. These violations result in the loss of all unspent tokens and restriction to the unit for 72 hours. During the 72 hours, patients can continue to earn all available tokens but can only spend tokens on extra smoke breaks.
Individual plans target specific patient needs, such as increasing eating, improving hygiene, reducing cursing, and decreasing self-mutilating behavior. A patient either earns extra tokens for performing a desired behavior or pays tokens for performing an undesired behavior.
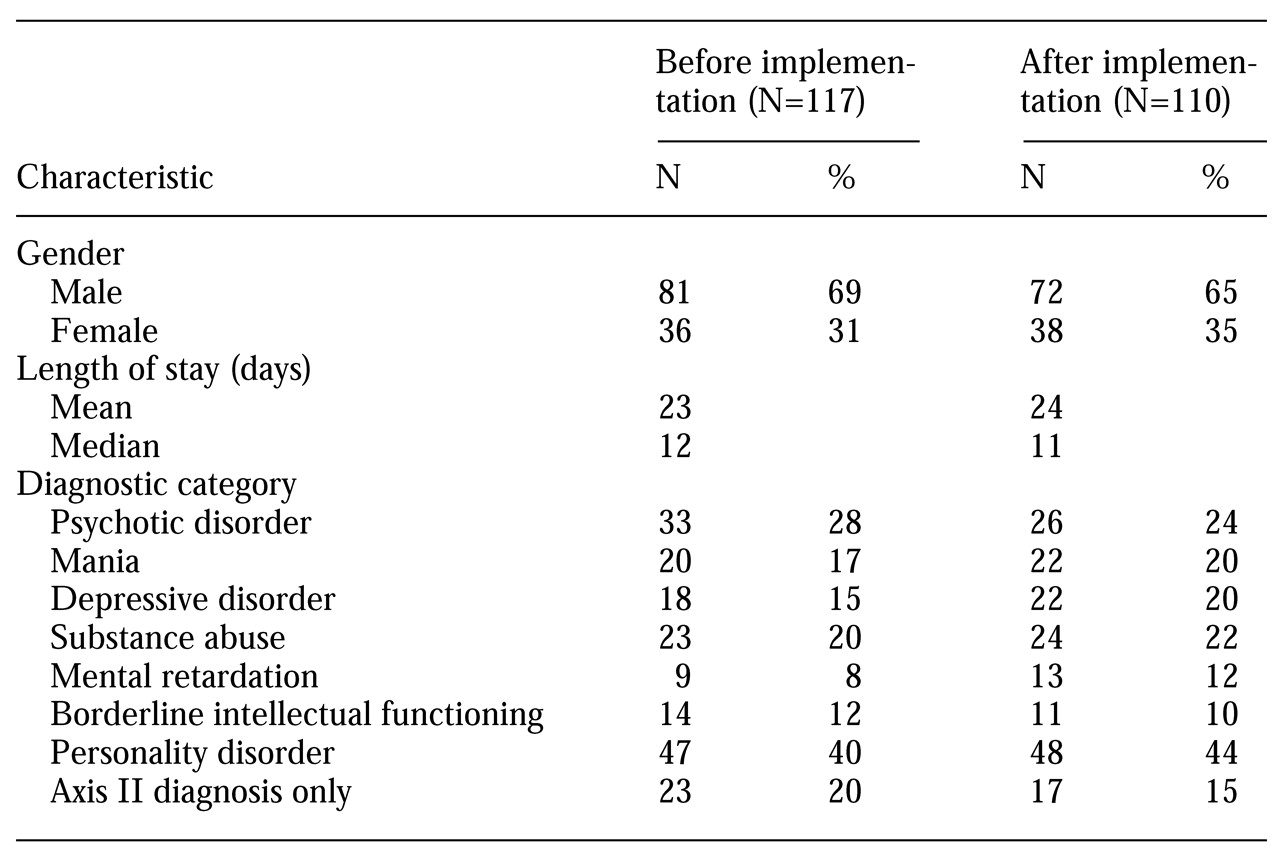
Design and procedure
Two four-month periods were assessed in the study—the first period, from October 1996 through January 1997, without the token economy, and the second period, from April 1997 through July 1997, with the token economy. Before implementation of the token economy, staff members participated in group training sessions in which the policies and procedures were discussed and role playing of the proper administration of tokens was performed.
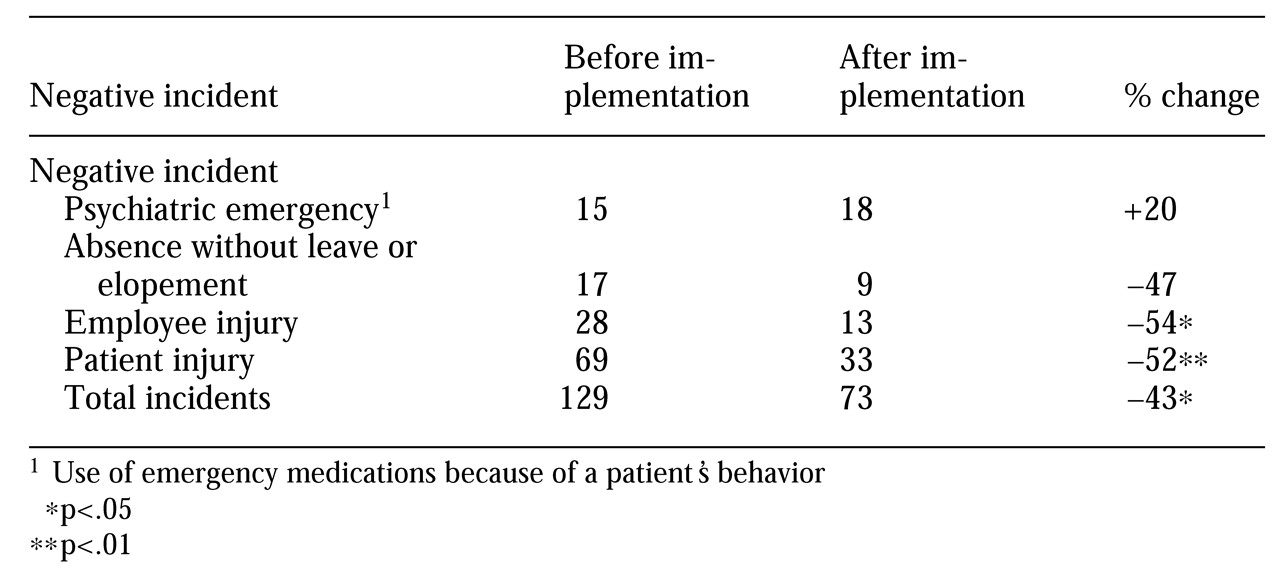
The number of negative incidents during both periods was compared. The collection of information about negative incidents is required for all units as part of the bylaws and procedures of the facility. Negative incidents were defined as staff and patient injuries that were not accidents; the definition also included absences without leave and elopements and psychiatric emergencies. Psychiatric emergencies were incidents in which emergency medications were used because of a patient's behavior. Staff and patient injuries were defined as injuries that required any form of medical attention, the lowest threshold of attention being the need for a visual examination of the injured area.