With the aging of the population and the shift toward community care, growing numbers of older parents are caring for a son or daughter with disabilities (
1,
2). In New York State alone, almost 11,000 adults with serious mental illness live with their aging parents (
3). Family-based care is also the dominant residential arrangement for persons with mental retardation; more than one-quarter of those who reside with family members live in households headed by aging parents (
4).
For both adults with mental illness and those with mental retardation, the need for services will increase after the deaths of their parents, but if siblings are willing to take on at least partial responsibility, the cost to the public will be reduced and the continuity of family-based support will be ensured. Little is known, however, about the propensity of adult siblings to assume caregiving roles (
5).
The purpose of the study reported here was to identify factors associated with the involvement of midlife siblings with a brother or sister who has a disability, including their current provision of instrumental and emotional support as well as their expectations about future caregiving. These siblings are not currently caregivers, but they can anticipate a time when their parents will no longer function in this role, and when they might be expected to assume more active caregiving responsibility.
We chose to compare families of adults with mental illness with families of adults with mental retardation because they are faced with similar yet distinct sets of stressors. The stressors are similar because they involve the long-term need for family support for a loved one who might never lead a fully normal life.
Differences in stressors include the timing of the diagnosis and the course of the disability. Whereas the diagnosis of mental retardation generally occurs at birth or in early childhood, mental illness is commonly diagnosed during late adolescence or early adulthood. Hence, most siblings of adults with mental retardation grew up with a sibling whose disability was a prominent feature of family life, whereas most siblings of persons with mental illness needed to adjust to the diagnosis in adulthood. Further, whereas the functional abilities and behavioral problems of adults with mental retardation are generally stable over time, mental illness is marked by episodic relapses. Thus, compared with sibings of adults with mental retardation, siblings of adults with mental illness have greater uncertainty about their brother's or sister's current and future care needs.
The relationship between adult siblings and their brother or sister with disabilities may be conceptualized as the product of various factors that either push siblings toward greater involvement or pull them away. One set of "push factors" arises from differences in childhood socialization experiences. Chodorow (
6) has argued that women are socialized from early childhood to care for others. Siblings of persons with mental retardation are socialized to anticipate a caregiving role as part of future family responsibility (
7,
8,
9). In contrast, siblings of adults with mental illness generally spend their formative years more or less unaware of the looming mental illness and hence are not socialized to expect a future caregiving role.
Another set of factors that push the sibling toward the caregiving role are feelings of closeness with the family. Life course research suggests a continuity in family relationships over time, and thus the quality of family-of-origin relationships forms a template for sibling relationships in adulthood (
10). In families with an adult child with disabilities, the nondisabled siblings may be more involved to support the parents, particularly when the siblings have a close relationship to the family and are concerned about the toll that caregiving takes on the parents. Thus sibling involvement may be sustained by family values that emphasize closeness across the generations and over time.
However, multiple midlife roles—marriage, parenthood, and career—are "pull factors" that can strain sibling involvement (
11). Horwitz and his colleagues (
12) found that siblings who have multiple role commitments are less involved with their brother or sister with mental illness. However, whereas the role demands associated with midlife may limit the sibling's current involvement, such roles may be less likely to affect the sibling's willingness or ability to provide care in the future, when the high demands of midlife, particularly child rearing, will be diminished.
An additional pull factor that might limit sibling involvement is the severity of the brother's or sister's behavior problems (
13). Adults with mental illness often have elevated levels of behavior problems, which may disrupt family relationships. Adults with mental retardation, although also subject to such difficulties, manifest behavior problems at a lower rate. In both groups, the presence of behavior problems may limit the degree to which siblings are willing to assume a supportive role in the life of their brother or sister with disabilities.
Based on past research and on our conceptualization of push and pull factors affecting sibling involvement, we made the following hypotheses.
• Siblings of adults with mental illness will provide less instrumental and emotional support at the present time and will have more limited expectations of future caregiving responsibility than siblings of adults with mental retardation.
• Sisters of adults with disabilities will provide more support than brothers and will be more likely to expect that they will have caregiving responsibilities in the future.
• The extent of current sibling instrumental and emotional support for the brother or sister with disabilities and the expectation of future caregiving responsibility will be a function of the sibling's feelings of closeness to his or her family of origin.
• Siblings who are more strongly established in midlife roles will provide less support currently to their brother or sister with disabilities, but these factors will not predict expectations of future caregiving responsibility.
• Siblings of adults with more behavior problems will provide less current support and be less likely to expect future caregiving responsibilities than siblings of adults with fewer behavior problems.
Methods
Sample
This analysis is based on two related longitudinal studies of aging parents who have an adult child with a disability (
14,
15). In both studies, families met two criteria when the study began: the mother was age 55 or older, and the son or daughter with disabilities was living at home. However, as noted below, some adults moved away from the parental home during the study period. Data were collected from multiple family members including siblings, who are the primary respondents for this analysis. Data from siblings of adults with mental retardation were collected during the sixth wave (1996) of an eight-wave study, and data from siblings of adults with mental illness were collected at the second wave (1994-1995).
All of the participating families of adults with mental illness (N=73) lived in Wisconsin. About half of the families of adults with mental retardation lived in Wisconsin (N=190), and the other half lived in Massachusetts (N=165). This analysis of siblings of adults with mental retardation is restricted to those living in Wisconsin to control for state differences in community services that may have affected the involvement of siblings.
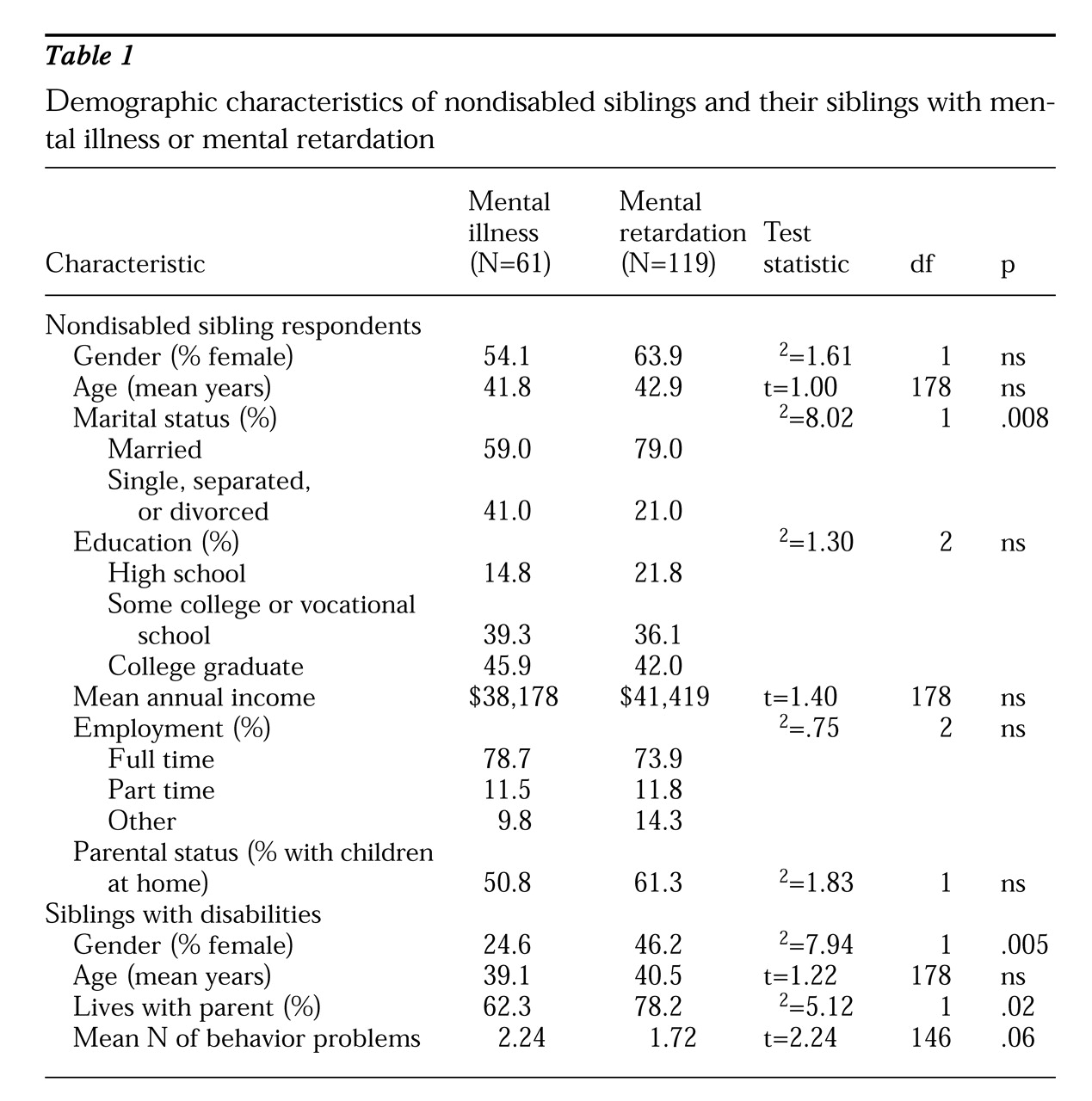
Siblings who participated in the study were identified by their mothers, who were asked to indicate which of their other adult children was most involved with the adult with disabilities. The sample for the analysis reported here consisted of 61 siblings of adults with serious mental illness and 119 siblings of adults with mental retardation. As
Table 1 shows, the two groups of siblings shared many characteristics, including gender, age, education, income, employment status, and parental status. However, significantly more of the siblings of adults with mental retardation were married.
The two groups of adults with disabilities were similar in age, but a significantly higher percentage of the adults with mental retardation were female. Adults with mental retardation were more likely to be living with their parents when the data for this study were collected. Also, adults with mental illness had a higher frequency of behavior problems. All had a diagnosis of a serious mental illness, most commonly schizophrenia (72 percent). Most of the adults with mental retardation had mild or moderate retardation (28.4 percent and 42.2 percent, respectively).
Data collection and measures
Data were collected using a self-administered mailed questionnaire. Data were collected on the following characteristics of the sibling: gender (coded 1 for female and 0 for male), education (coded from 1 to 6, for categories ranging from eighth grade or less to college degree), family income in dollars, and age. Characteristics of the adult with the disability included gender (coded 1 for female and 0 for male), residence (coded 1 for in the parental home and 0 for elsewhere), and presence of behavior problems. The measure of behavior problems, developed by Bruininks and associates (
16), was a count of up to eight maladaptive behaviors, such as being harmful to self and withdrawn, reported by the mother, who had the most contact with the adult with disabilities.
Data on the sibling's midlife roles included employment status (coded 1 for employed full time and 0 for otherwise), marital status (coded 1 for married and 0 for otherwise), and whether the sibling had children under the age of 18 at home (coded 1 for yes and 0 for no). Data on closeness to the family of origin included residential proximity to the brother or sister with the disability (coded 0 for more than one hour, 1 for less than one hour, and 2 for less than 15 minutes), and current level of emotional closeness of the nondisabled sibling to the mother and closeness of the siblings during adolescence (both coded from 0 to 3, for categories ranging from not at all close to very close).
The dependent variables were three indicators of the sibling's involvement with the brother or sister with disabilities. Two were indicators of current provision of instrumental and emotional support, and one was an indicator of the expectation of caregiving responsibility in the future.
The amount of instrumental support provided currently was assessed for four types of caregiving activities—direct caregiving, transportation, financial assistance, and running errands. The sibling indicated how much help he or she currently provided for each caregiving task on a scale from 0, none, to 2, a lot. Items were summed for a total score. Alpha reliability for the samples of siblings of adults with mental illness and mental retardation were .73 and .76, respectively.
The amount of emotional support provided by the sibling was measured using two items that assessed the extent of provision of companionship and general emotional support on a scale from 0, none, to 2, a lot. Alpha reliability for the samples of siblings of adults with mental illness and mental retardation were .73 and .76, respectively.
Different questions were asked of siblings of adults with mental illness and siblings of adults with mental retardation about the expectation of future caregiving responsibility. Siblings of adults with mental illness were asked whether any member of the family was expected to take primary responsibility for providing help to the adult with disabilities after the parents are no longer the primary caregivers. The nondisabled sibling could identify him or herself (coded 1) or someone else or no one (coded 0).
Siblings of adults with mental retardation were asked to indicate who would take primary responsibility for each of three caregiving tasks after the parents were no longer the primary caregivers: providing or arranging for housing, financial oversight, and guardianship. Siblings were designated as having future caregiving responsibility (coded 1) if they planned to assume primary responsibility for these three tasks.
Results
Diagnostic-group differences
We hypothesized that siblings of adults with mental illness would be less involved than siblings of adults with mental retardation with the brother or sister with disabilities. Analysis of covariance was used to test this hypothesis. The covariates were the four characteristics on which the two samples differed significantly—the nondisabled sibling's marital status and the gender, residential status, and number of behavior problems of the adult with disabilities. Due to the small size of the sample of siblings of adults with mental illness, we report trends up to p<.10.
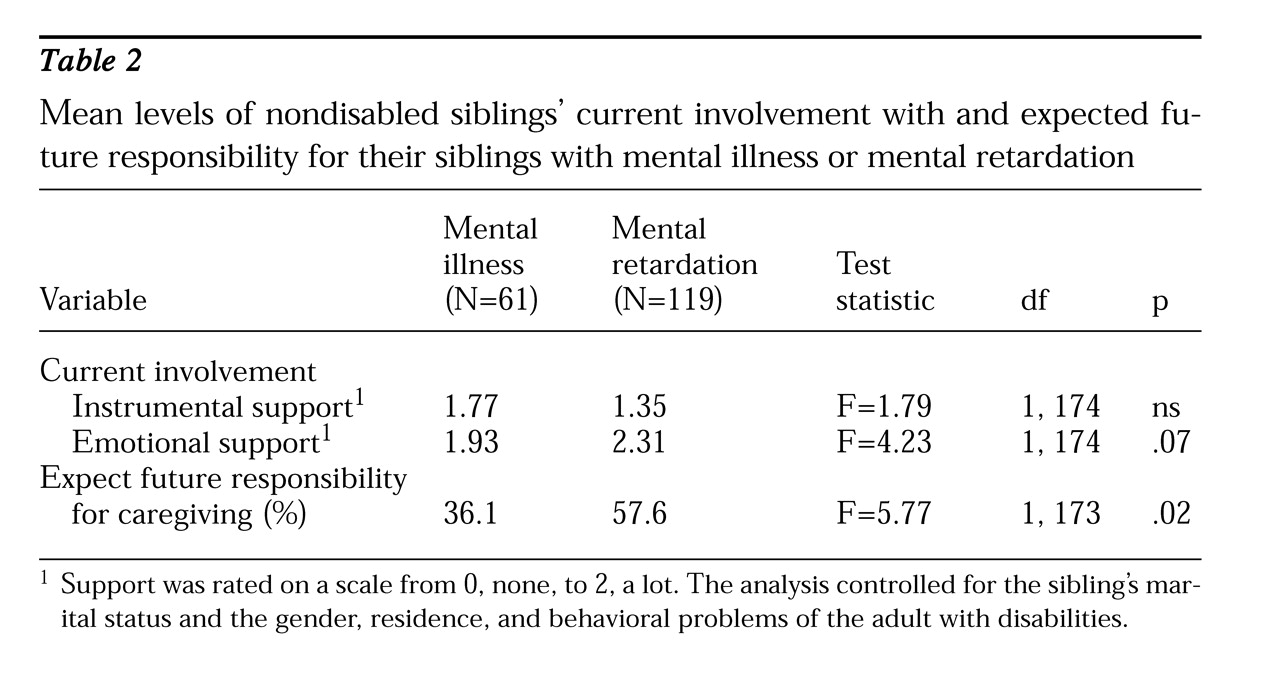
As shown in
Table 2, the two groups of siblings did not differ in the amount of instrumental support they provided to their brother or sister with disabilities. However, compared with siblings of adults with mental illness, siblings of adults with mental retardation provided significantly more emotional support and were more likely to expect to have primary caregiving responsibility in the future.
Current involvement and future caregiving
The remaining four hypotheses addressed the predictors of current involvement and future caregiving responsibility for the brother or sister with disabilities. These hypotheses were tested using ordinary least squares and logistic regression. Mean substitution was used to handle missing data on the independent variables. Preliminary analyses were conducted to reduce the number of independent variables because of the small size of the sample of siblings of adults with mental illness.
Employment status, income, marital status, and age of the sibling were dropped after preliminary analyses because they neither added to the variance explained nor altered the pattern of findings. Because the processes explaining sibling involvement may depend on whether the adult with disabilities lives with or apart from the parents, we tested for interaction effects between the residential status of the adult with disabilities and each independent variable in the model. Only significant interactions are reported.
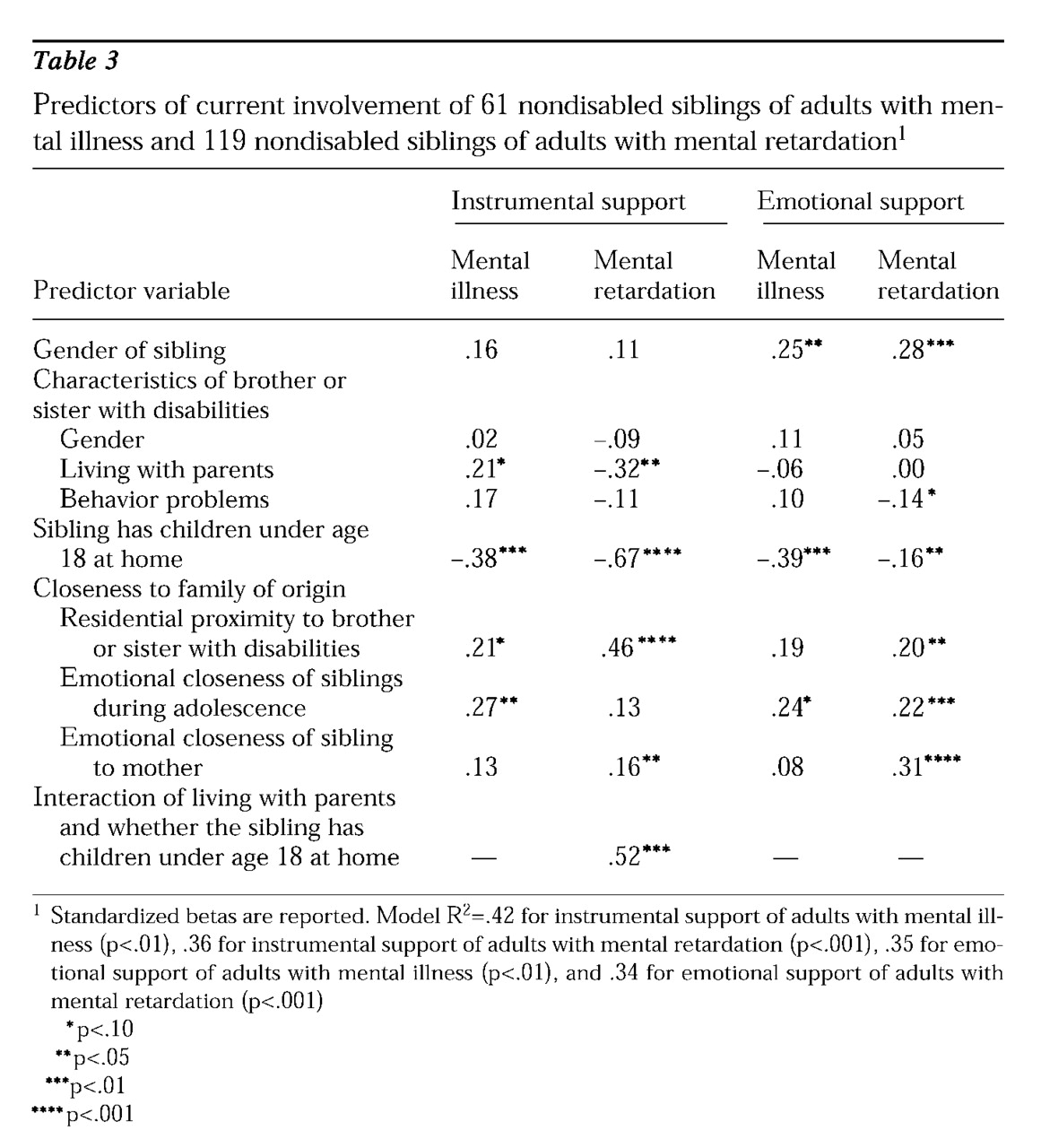
Current provision of instrumental support.
For both groups of siblings, those with minor children living at home were significantly less likely to provide instrumental support, whereas those who lived in close proximity to the adult with disabilities were more likely to be supportive (see
Table 3). For siblings of adults with mental illness, the provision of instrumental support was more likely if the sibling relationship was close during adolescence and if the brother or sister with mental illness continued to live in the parental home. Siblings of adults with mental retardation who had a closer relationship with their mother provided more instrumental support than siblings who had a more distant maternal relationship.
We found a significant interaction effect between the place of residence of the adult with mental retardation and whether the sibling had minor children at home. When the sibling did not have minor children at home, the adult's place of residence did not affect the amount of instrumental support provided. However, when the sibling had children at home, he or she was less likely to provide support if the adult with mental retardation lived away from the parents.
Current provision of emotional support.
In both groups, sisters provided more emotional support than brothers, and siblings with minor children at home provided less emotional support than those without minor children (see
Table 3). Siblings of adults with mental retardation provided less emotional support when the adult had behavior problems that were more severe. Further, for siblings of adults with mental retardation, living in close proximity to the brother or sister with disabilities, feeling emotionally close to him or her during adolescence, and currently having a close relationship to the mother were all significant predictors of emotional support. In contrast, for siblings of adults with mental illness, only a close sibling relationship during adolescence was predictive of whether the sibling currently provides emotional support.
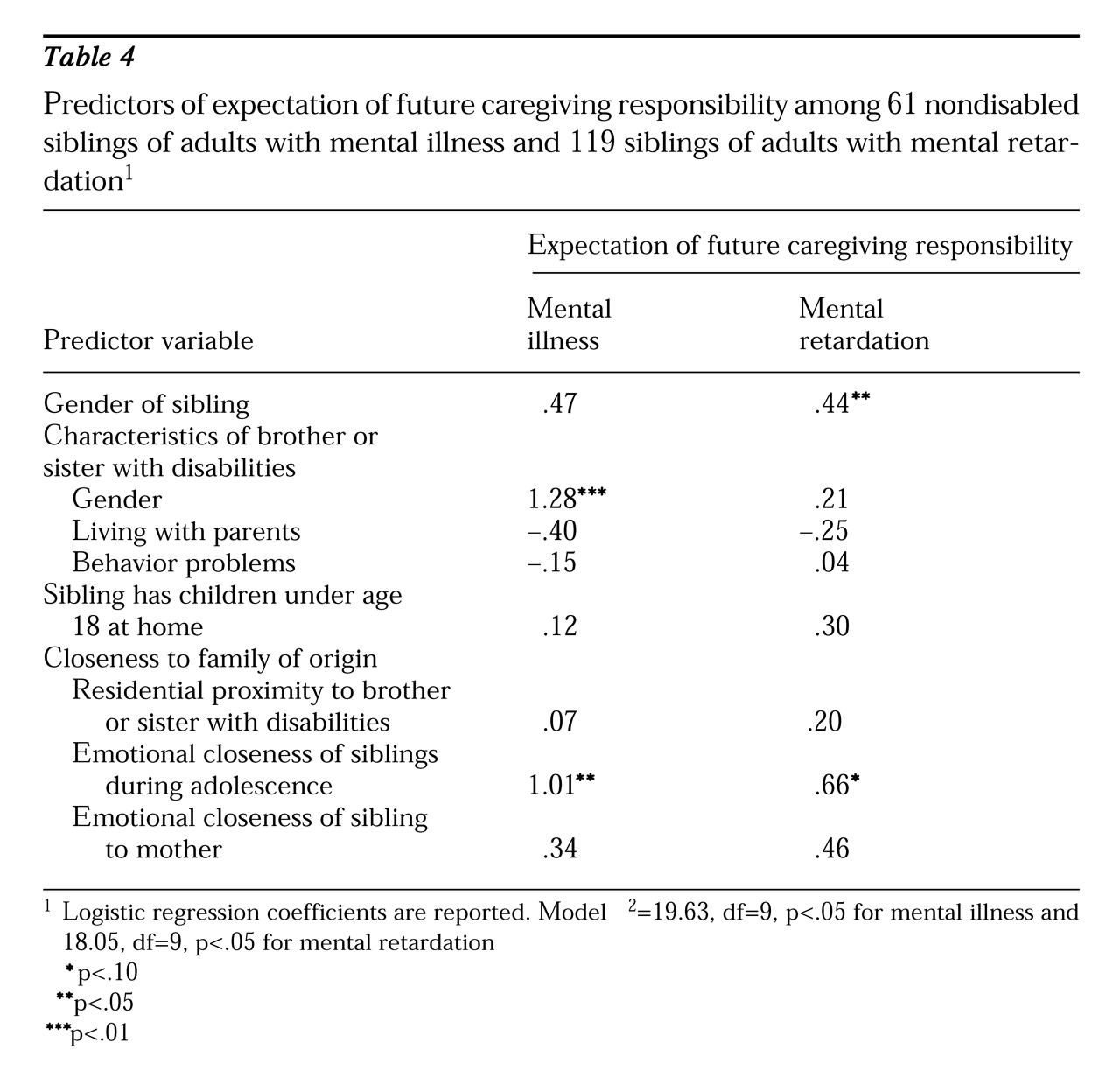
Sibling's expectation of future caregiving responsibility.
As
Table 4 shows, for both groups, gender was a significant predictor of expecting to have responsibility for future caregiving. Siblings of women with mental illness expected to have caregiving responsibility in the future, but the gender of the nondisabled sibling was not a significant predictor. In contrast, sisters of adults with mental retardation expected caregiving responsibility in the future, but the gender of the adult with mental retardation was not a significant predictor. For both groups, those with a closer sibling relationship in adolescence expected to assume future caregiving responsibility.
Discussion
The two groups of siblings were similar in the amount of instrumental support they currently provided to their brother or sister with disabilities, but siblings of adults with mental retardation provided more emotional support than siblings of adults with mental illness and were more likely to expect to have future caregiving responsibility. The divergence of these two groups of siblings in the expectation of future caregiving responsibility was substantial. Only one-third of the siblings of adults with mental illness expected to assume future caregiving responsibility. Nearly twice as many siblings of adults with mental retardation expected a future caregiving role. Nevertheless, substantial numbers of adults with disabilities now being cared for by their aging parents will need to turn to the public service system to meet their needs. Without a dramatic shift in public resources for community care, the needs of many adults with disabilities will go unmet.
We conceptualized the involvement of siblings as a function of various push and pull factors that affect their likelihood of playing a supportive role. Families with strong emotional bonds fostered nondisabled siblings' continued involvement. All too often, researchers have focused narrowly on the negative aspects of family relationships among persons with disabilities. Our findings highlight the importance of recognizing positive family bonds, which encourage sustained involvement of family members in the care of adults with mental illness and mental retardation.
Another push factor was gender, reflecting the differential socialization of women and men (
6). For both groups, sisters provided more emotional support than did brothers, and, compared with brothers, sisters of adults with mental retardation more often expected a future caregiving role. However, the gender of the brother or sister with disabilities was also salient for siblings of adults with mental illness; they were more likely to expect future caregiving responsibility for a sister than for a brother. This finding possibly reflects the greater difficulty of providing care for a man with mental illness because men appear to experience a more debilitating course of illness (
17).
We also found evidence that pull factors limited sibling involvement. One such factor was whether the nondisabled sibling had children at home, which was predictive of providing both less instrumental and emotional support to the brother or sister with disabilities. However, having children at home was not related to the sibling's expectation of future caregiving responsibility. These findings suggest that although responsibility for the sibling's own family may compete with current involvement, having children is not a long-term constraint affecting the willingness of siblings to assume future caregiving responsibility, which generally begins after the children have left home.
Although we had hypothesized that behavior problems would be a pull factor, limiting sibling involvement, they were not a significant predictor of any measure of involvement for siblings of adults with mental illness and were only a weak predictor of emotional support provided by siblings of adults with mental retardation. One explanation for why they were not predictive is that we were limited to a set of questions that were common to both studies, and thus the severity of the behavior problems of the adults with mental illness may have been underestimated. A second possible explanation is that behavior problems may have counteracting effects, functioning both as a push factor, by interfering with the sibling relationship, and a pull factor, by mobilizing siblings to come to the assistance of their parents. These possibilities warrant a more complete investigation in future research.
Our study had several limitations. First, all families volunteered to participate in the research, so subjects might not be representative of the population of siblings of adults with disabilities. Second, the sample of siblings of adults with mental illness was small, consequently limiting the statistical power of the analyses. Thus our findings on this group should be interpreted cautiously. Third, a very specific question was posed to siblings of adults with mental retardation about their expectations of future caregiving, which may have underestimated the number who would have responded affirmatively to a more general question, like the one posed to siblings of adults with mental illness.
Nevertheless, the results of these analyses have two critical implications for service providers who work with families of adults with mental disabilities. First, the findings highlight the importance of involving siblings. Mental health and other service providers often overlook siblings' needs for support and information. Clinicians should expand efforts to reach out to siblings, especially during adolescence, a stage of life during which the sibling may be particularly sensitive to the social stigma of a brother or sister's disability. Supporting and educating siblings about mental illness and mental retardation may help them develop a deeper understanding of their brother or sister's experience, which may foster a closer relationship.
Second, our findings help identify a group of adults with disabilities who are particularly vulnerable to the loss of family support after the death of their parents, namely those who were not close to their siblings during adolescence. In addition, men with mental illness are more vulnerable than women, whereas in the case of mental retardation, the most vulnerable are those without a sister. Mental health providers should help these adults develop a future care plan while the parents are still healthy to smooth the transition to nonparental care.
Conclusions
The extent of current and future involvement by siblings of adults who are disabled by mental illness or mental retardation appears to be a function of the demands and constraints of midlife, as well as the degree of closeness with the family of origin. These pull and push factors, on the one hand, stand in the way of sibling involvement with the brother or sister with disabilities and, on the other hand, promote continued closeness. They serve as the backdrop against which the eventual transition to nonparental caregiving will take place. The extent to which expectations for future caregiving are borne out awaits assessment in longitudinal analyses.
Acknowledgments
Preparation of this paper was supported by the Joseph P. Kennedy, Jr., Foundation, grant R01-AG-08768 from the National Institute on Aging, grants R03-MH-465644 and F31-MH-10649 from the National Institute of Mental Health, grant T32-HD-07489 from the National Institute of Child Health and Human Development, the Waisman Center and the Graduate School of the University of Wisconsin-Madison, and the Florence Heller Graduate School for Advanced Studies in Social Welfare at Brandeis University. The authors thank Rachel Pruchno, Ph.D., for comments on an earlier version of the paper.