As the population of the United States has grown and changed over the past few decades, especially in urban areas, cultural competency in psychiatric practice has become increasingly important. In mental health care, in which clear communication and a sense that the client is respected and understood are particularly important for developing and maintaining a therapeutic alliance, differences in language and culture can impair the effectiveness of treatment. In addition, persons from different ethnic backgrounds have been shown to have different patterns of treatment use, both for inpatient services and for outpatient services (
1). Thus attention to cultural differences has become vital in the provision of appropriate care to persons with mental illness.
In general, persons from ethnic minority groups have been found to have fewer contacts with mental health services than whites (
2). Specific service use patterns have also been noted for persons from certain ethnic groups. For example, blacks use more emergency and inpatient mental health services than outpatient services, whereas whites use more outpatient services; blacks also have a higher rate of involuntary commitment (
3,
4). Asians and Latinos, on the other hand, use comparatively more outpatient mental health services than whites and are hospitalized less frequently (
2,
5). Treatment outcome has been less well studied, but ethnic differences have been suggested by dropout rates and by scores on the Global Assessment Scale; blacks fare less well on both measures than Latinos, Asians, or whites (
1,
6).
As a result of demographic changes and the changing needs of the patient population, many mental health facilities are striving to develop culturally competent psychiatric treatment programs (
7). Psychotherapy and case management services have led the way in this regard: matching therapists and clients by ethnicity or other characteristics, such as sexual orientation, is now relatively common (
8,
9). Community outpatient psychiatric clinics have also become more attuned to cultural factors. In many urban areas of California, a large proportion of outpatient programs focus on persons with specific ethnic or cultural backgrounds, primarily as a natural consequence of geographic and demographic clustering. Some studies have shown that mental health programs with a focus on specific ethnic groups are effective in increasing treatment retention (the percentage of referred patients who attend more than one outpatient session) and treatment duration (the amount of time a person stays in outpatient treatment) (
1,
10), whereas other studies have not demonstrated effectiveness (
9).
However, for the most part, ethnically or culturally focused treatment has not been available to inpatients. Although many large hospitals now have specific language services, only a few inpatient units are intentionally focused to address the needs of a particular cultural group. One example is the specialty focus units at San Francisco General Hospital, the only public acute care hospital in San Francisco County.
Developed initially for the purpose of teaching cultural competency in psychiatric practice to trainees in psychiatry, psychology, and social work, the inpatient units at San Francisco General Hospital have several specialty teams. Each team focuses on a particular ethnic group, such as Asians, blacks, or Latinos, or another group with specialized needs, such as women, gay and lesbian patients, or persons with HIV infection or AIDS (
11). The teams attempt to diagnose and treat psychiatric inpatients in a culturally competent manner.
Several of the staff on the ethnic specialty teams share the cultural background of the patients they serve. Many are bilingual or multilingual. Members of the various specialty focus teams are fluent in Spanish, Cantonese, Mandarin, Tagalog, Vietnamese, and ten other Asian languages and Chinese dialects.
Patients who do not speak English are assigned preferentially to an appropriate focus unit. Because of the high volume of patients who are treated in the county hospital, other patients are assigned to focus units on the basis of the availability of beds at the time of admission. Thus these units are necessarily heterogeneous in ethnic composition. However, in general, most patients on the Asian focus unit are of Chinese or Filipino descent, and most patients on the Latino unit are of Mexican or Central American descent.
Virtually nothing is known about the relationship between ethnic specialization and the treatment outcome or diagnosis of inpatients. Thus the specialty focus units at San Francisco General Hospital provided a unique opportunity to study these relationships. The relationship between matching and diagnoses was examined in a separate study, also published in this issue (
12). In this study we examined the relationship between matching patients to ethnically focused units and treatment outcome. We hypothesized that matching inpatients to ethnically focused psychiatric units would improve treatment outcome for patients from ethnic minority groups.
Methods
Data sources
Data were extracted from the management information system database of the San Francisco County Department of Community Mental Health Services, a database that tracks demographic and clinical information, and data on referrals and service providers for each patient admitted to one of the psychiatric units. The data were collected through standardized forms that are completed by the treating clinicians at admission and at discharge. Approval for the study was obtained from the committee for human research for the University of California, San Francisco, and from the Division of Mental Health, Substance Abuse, and Forensic Services in the Department of Public Health for San Francisco County. The data were placed into a SAS 6.12 format for data management purposes and were subsequently imported into Stata 6.0 for statistical analysis.
Study subjects
We examined data for all psychiatric inpatient admissions between 1989 and 1996 to three specialty focus units—an Asian focus unit, a Latino focus unit, and a black focus unit. Patients were included if they were between the ages of 20 and 80 years and were Asian, Latino, black, or white. Patients from other ethnic groups (6 percent of admissions), including persons of Native American, Middle Eastern, Russian, and mixed or unknown descent, were not included. The final study sample consisted of 5,983 psychiatric patients, representing 10,645 admissions. Asians—persons of Chinese, Japanese, Filipino, Vietnamese, Laotian, Cambodian, Korean, Pacific Islander, and other Southeast Asian descent—represented 14 percent of all inpatient admissions. Latinos—persons of Mexican, Spanish, Latin American, Puerto Rican, and Cuban descent—represented 11 percent of all inpatient admissions (1,120 admissions). Blacks represented 26 percent (2,827 admissions), and whites represented 48 percent (5,064 admissions). For all analyses presented in this article, the unit of analysis is admission. For the proportional hazards model, statistical corrections were made to control for the fact that individual patients had multiple admissions.
Patients who were admitted to an ethnically appropriate psychiatric unit—for example, an Asian patient who was admitted to the Asian unit—were considered to be "matched." Patients who were admitted to a unit that focused on an ethnic background other than their own—for example, a black patient who was admitted to the Latino unit—were considered to be "unmatched." White patients, who were admitted to all ethnically focused units as well as to a unit that did not have a specialty focus, were treated as a separate group and were used as the basis for comparison. Overall, 3,600 admissions (34 percent) were ethnically matched, 1,981 (18 percent) were unmatched, and 5,064 (48 percent) were admissions for white patients. A total of 1,258 Asian admissions (77 percent), 1,578 black admissions (56 percent), and 764 Latino admissions (68 percent) were matched.
Most patients (8,917, or 83 percent) spoke English as their primary language. Other primary languages were divided into three main categories: Spanish (584 patients, or 5 percent), Asian languages (829 patients, or 8 percent), and other or unknown languages (315 patients, or 4 percent). Fifty-two percent of all Asian admissions and 48 percent of all Latino admissions were for non-English speakers. In contrast, 3 percent of all black admissions and 3 percent of all white admissions were for non-English speakers. Between 14 percent and 20 percent of all admissions for non-English speakers were unmatched.
Outcome variables
We examined three outcome variables: referral destination, risk of rehospitalization within one year after discharge, and length of stay. Referral destination included referral to a state inpatient psychiatric hospital, residential placement, outpatient treatment, and discharge without follow-up treatment. Thirty-seven percent of patients had multiple admissions during the seven-year study period. The referral destination after each admission was included in the analysis.
Statistics
Cox proportional-hazards methods were used to assess risk of hospitalization and length of stay. Multinomial regression was used to assess differences in referral destination. Differences between ethnic groups were examined with chi square analyses. The robust variance method (
13) was used to correct for multiple admissions per patient in the proportional-hazards regression. The method of Liang and Zeger (
14) was used to correct for the dependencies potentially created by multiple admissions per patient in the multinomial regression. Analysis of variance was used to examine differences in mean length of stay.
Results
Referral destination
Patients were referred to a variety of follow-up programs on discharge from the inpatient units, including restrictive inpatient settings such as the state hospital or long-term locked facilities, less restrictive supervised facilities such as residential treatment facilities, and traditional outpatient follow-up or day treatment centers. Although attempts were made to provide referrals on discharge, some patients refused follow-up treatment. Referral destination was divided into three mutually exclusive categories: locked facilities, residential treatment or outpatient settings, or home self-care (which included patients who refused further treatment). Individual patients who were referred to more than one type of treatment were categorized according to the most restrictive or intensive type of treatment to which they were referred.
Referral destination was assessed in two ways. We conducted an initial multinomial regression analysis by entering ethnicity, matching status, diagnosis, sex, language, and total number of admissions in the previous year into the model as predictor variables. The multinomial regression indicated a significant relationship between matching status and referral destination for patients who either were admitted to locked facilities (z=-2.26, p=.024) or refused further treatment (z=-3.96, p<.001) compared with patients who were referred to residential or outpatient settings. This association was independent of primary language, which was also significantly associated with referral destination (for locked facilities, z=2.50, p=.013; for no further treatment, z=5.45, p<.001).
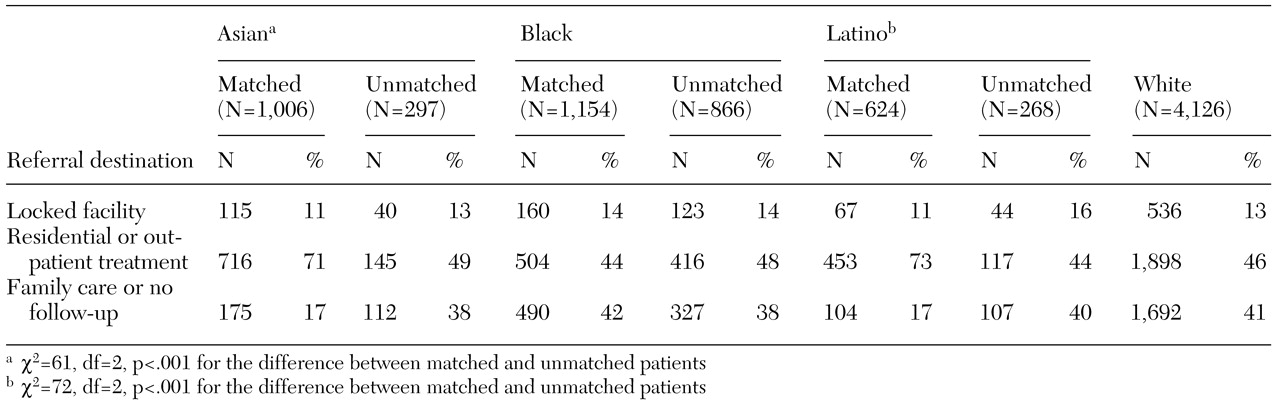
The association between matching status and referral destination was further assessed with chi square analyses that were stratified by ethnicity. The results are summarized in
Table 1. The results of these analyses suggested that for Asian and Latino patients, but not for black patients, matching was associated with a significantly greater likelihood of being referred to residential or outpatient treatment and a significantly lower likelihood of being referred to a locked facility or refusing follow-up. In general, 38 to 40 percent of unmatched patients refused follow-up treatment, compared with 17 percent of matched Asian and Latino patients and 42 percent of matched black patients. Referral patterns for white patients were similar to those for unmatched ethnic minorities.
Risk of rehospitalization
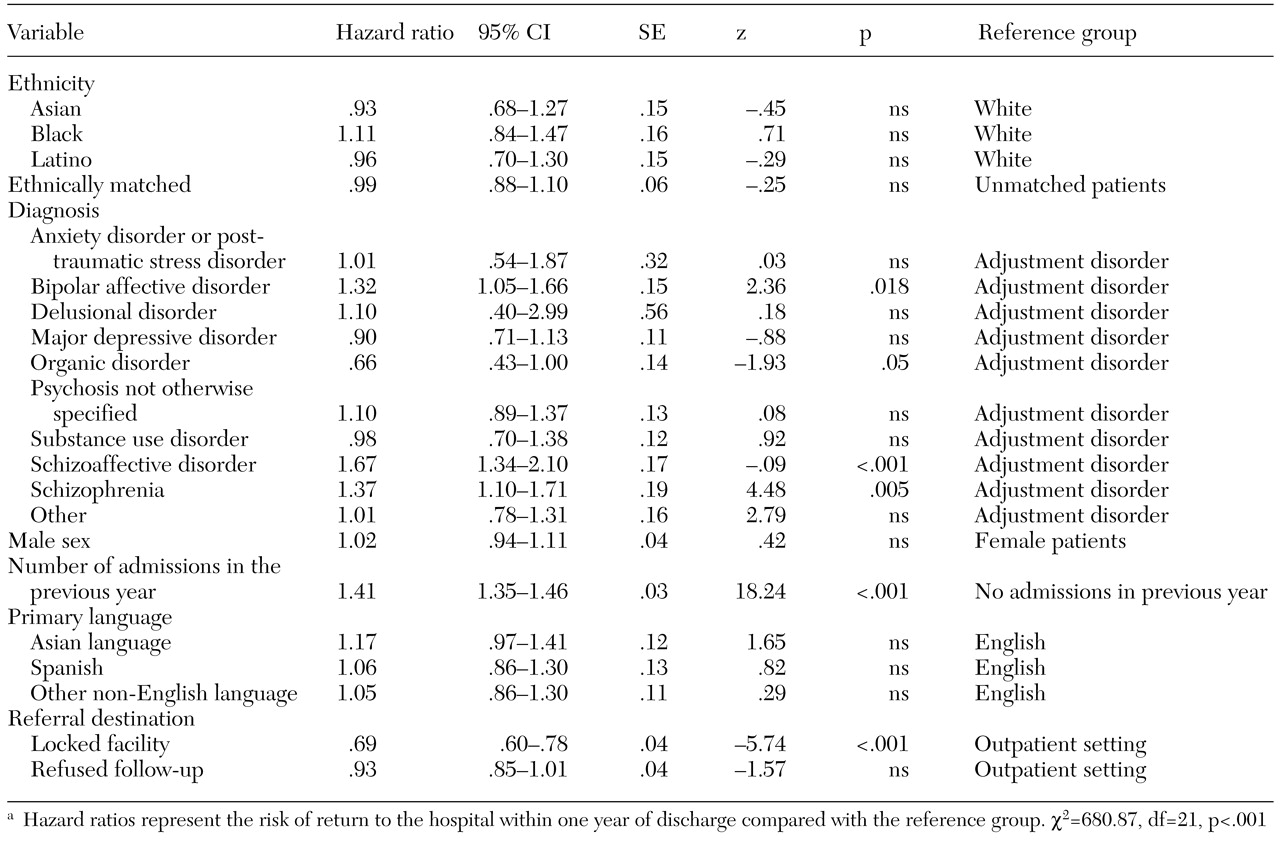
Rehospitalization within a year of discharge was assessed with a Cox proportional-hazards model. The results are summarized in
Table 2. Ethnicity, sex, matching status, diagnosis, language, number of admissions in the previous year, and referral destination were all included in the model, which was significant. Matching status, ethnicity, and primary language were not significantly associated with rehospitalization rate, although diagnosis of a severe disorder was. For patients with diagnoses of bipolar affective disorder, schizoaffective disorder, or schizophrenia, the risk of returning to the hospital within a year was 32 to 67 percent greater than for patients with a diagnosis of an adjustment disorder, which was the comparison diagnosis.
Similarly, the number of admissions in the previous year, another indicator of the severity of illness, was strongly associated with the risk of readmission: for every hospitalization in the previous year, the risk of readmission in the subsequent year was 41 percent higher. Rates of rehospitalization within 30 days and within 90 days were also examined, because rehospitalization within a short period is thought to be due to a different mechanism—for example, a partially treated episode of illness—than rehospitalization later on. The results of these analyses were similar to the results of the proportional-hazards model for return to the hospital within a year (data not shown).
Specifically, matching status, ethnicity, and primary language were not significantly related to the risk of readmission. Sixty percent of matched patients, 61 percent of unmatched patients, and 62 percent of white patients were readmitted to the hospital within one year.
Length of stay
The mean length of stay was longer for patients from an ethnic minority group than it was for whites and was longer for matched patients than for unmatched patients. For all admissions studied, the mean±SD length of stay was 18±22 days. The mean±SD length of stay was 20±24 days for matched patients, 18±22 days for unmatched patients, 17±22 days for white patients, 22±22 days for Asians, 18±24 days for blacks, and 18±20 for Latinos. When ethnicity and matching status were both incorporated into the model, the overall model was significant (F=15.98, df=4, 10,644, p<.001), as was ethnicity (F=18.02, df=2, 10,640, p<.001), although matching status was not. Only matched Asians had longer mean stays than their unmatched counterparts (23±23 days compared with 19±21 days).
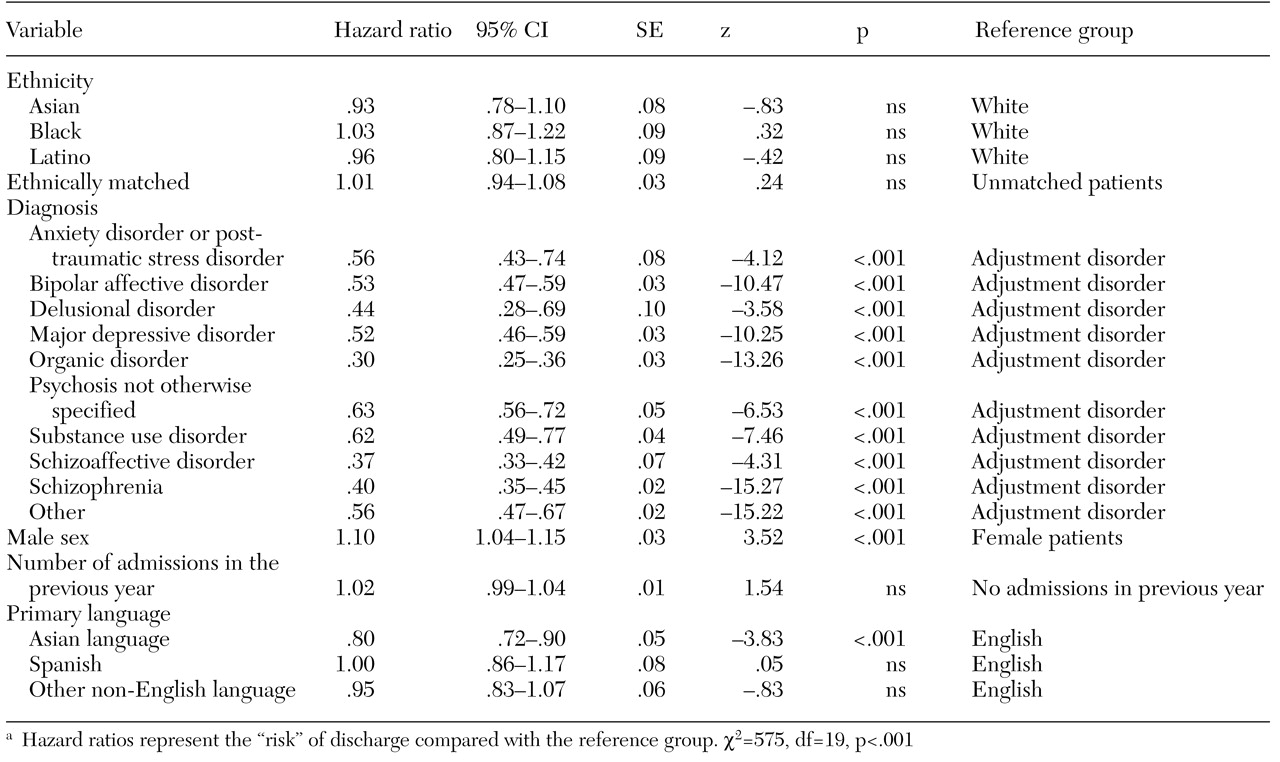
No significant association was found between matching status and length of stay, shown in
Table 3 as "risk" of discharge. Factors that were significantly associated with length of stay included diagnosis, male sex, and speaking only an Asian language. Men were 10 percent more likely than women to be discharged at any given length of stay, and English speakers were 80 percent more likely to be discharged than patients who spoke only an Asian language—that is, they had shorter stays.
Discussion and conclusions
This study provided evidence that matching inpatients to ethnically focused psychiatric units, at least for some minority groups, improves one aspect of treatment outcome—referral to follow-up treatment after discharge. Matching was associated with a significantly greater likelihood that Asian and Latino patients would be willing to accept outpatient or residential treatment referrals and a significantly lower likelihood that they would be sent to locked facilities. One explanation for these findings is that the staff on the specialty units were more motivated to engage patients as a result of participating in an innovative clinical program. However, white patients who were assigned to these units did not demonstrate better outcomes. No association was found between matching status and length of stay or time to next hospitalization.
For persons with severe mental illness—the primary population served by San Francisco General Hospital—appropriate referral after hospitalization may be an important determinant of treatment outcome. The vast majority of the facility's inpatients are admitted on an involuntary 72-hour hold. In fact, only 22 percent of the patients studied were discharged with a legal status of "voluntary." This figure in all likelihood underestimates the total number of patients admitted on an involuntary hold, because some patients were admitted involuntarily and subsequently agreed to a voluntary admission. Although the high proportion of voluntarily admitted patients and the relatively short stays on the units might be hypothesized to contribute to the readmission rate, neither of these variables was statistically significant when included in the proportional hazards model. About 40 percent of patients admitted involuntarily leave against medical advice as soon as they are able to do so, usually refusing follow-up mental health treatment. Successful outpatient follow-up has been shown to significantly reduce the rate of readmission to inpatient units by up to 20 percent (
15).
Although we did not find an association between matching status and readmission, we cannot confidently rule out such an association. The specialized language capability of two of the specialty focus units makes it likely that non-English speakers were preferentially readmitted to San Francisco General Hospital when possible, whereas patients who spoke English were more likely to be referred to private hospitals. Because we did not have data on readmissions to other hospitals, this differential admissions procedure could have led to an undercount of returns to the hospital. Thus English-speaking patients would have appeared to have a longer survival in the community, creating a false-negative effect of matching.
Our data provide some support for this conjecture. Although Asian patients accounted for only 14 percent and Latinos for 10 percent of all admissions during the seven-year study period, about 50 percent of admissions for these ethnic groups were for non-English speakers. In addition, patients who spoke only an Asian language tended to have a higher rate of return to the hospital than those who spoke English—about 17 percent higher, but possibly as much as 40 percent higher (
Table 2). Although the specialized services provided by the focus units may have improved outcomes for such patients, it may not have completely offset the patients' higher risk of readmission and may have obscured a positive association between these units and readmission rates.
Diagnosis represents another possible bias in the process of matching patients to ethnically focused units. The results of our study on the relationship between matching and rates of various diagnoses among black, Latino, and Asian patients suggest that black patients who have more severe diagnoses are preferentially assigned to the black focus unit (
12). This finding may explain the observation that the black patients in this study who were matched to ethnically focused units refused follow-up as frequently as those who were not matched—the severity of the illness may have counteracted the beneficial effects of matching in this regard. Although we did not directly control for severity of illness, that variable was encompassed in two predictor variables—number of hospitalizations in the previous year and diagnosis. Both of these measures of severity were strongly associated with rate of return to the hospital. We therefore controlled for their effects in our analysis of the relationship between matching status and return to the hospital. However, this approach may not have completely eliminated the confounding effect of severity of illness.
It is striking that although language was strongly associated with referral rates and with length of stay, the effect of matching was independent of the language effect. Ethnically matched Asians and Latinos, both English and non-English speakers, were more likely than their unmatched counterparts—and more likely than white patients—to accept referral to treatment after discharge. Our findings thus suggest that language services and cultural competency are both important ingredients in the provision of a basic level of appropriate mental health care for ethnically diverse patients and in some cases can significantly improve the quality of care.
Acknowledgments
This research was partly supported by grant K23-RR-15533 from the National Center for Research Resources. The authors thank Bruce Stegner, Ph.D., for his help with the data analysis and Francis Lu, M.D., Robert L. Okin, M.D., and Jo-Ellen Branin-Rodriguez, M.D., for their comments on the manuscript.