Antidepressant medications and psychotherapy can substantially reduce or completely eliminate the symptoms of depression (
1), and a number of studies have demonstrated that organized programs of care for depression can deliver those treatments in primary care with resulting improvements in outcomes, both for quality of care and for depression (
2,
3,
4,
5,
6,
7,
8). Decisions about investing additional resources in depression treatment depend in part on the balance of improved outcomes and cost of such treatments (
9). Cost-effectiveness studies of such programs (
5,
8,
9,
10,
11) have concluded that providing effective treatment for depression improves health but also requires additional expenditures. Information about the value of such programs will be important for patients, health care providers, and policy makers who have to make decisions about investing additional resources in this area.
Willingness-to-pay methods have been used by health economists as one way to assess the value of a particular treatment or to compare the relative value of different treatments (
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26). The willingness-to-pay method is based on welfare economics; one of its advantages is the fact that it allows cost-benefit analyses that compare consumers' willingness to pay with the actual costs of treatment. Information on willingness to pay is well received by health care decision makers and may be a useful alternative to other methods of valuing health care technologies (
27,
28). This method has been shown to be feasible in studies of patients with depression and schizophrenia (
29), but few studies have used the methodology in mental health research (
14).
Methods
We used data from a population-based research program that tested two closely related models of depression treatment in primary care (
4,
30). The study was conducted from June 1996 to February 1998 in four primary care clinics of Group Health Cooperative of Puget Sound (GHC), a staff-model health maintenance organization (HMO) in western Washington. In these clinics, 73 board-certified family physicians cared for a population of 88,000 enrollees. GHC members have an age and income distribution that is generally representative of the population of the area.
Potentially eligible patients were identified with data from automated registration, pharmacy records, and visit records. Patients between the ages of 18 and 80 years who had received a new antidepressant prescription and a diagnosis of depression from a primary care physician in one of the four participating clinics were eligible for an assessment to determine their eligibility for the study. Six to eight weeks after the index prescription, patients received an invitation letter, followed by a phone call that sought verbal informed consent for a screening interview to determine eligibility for a study of two depression treatment programs, the persistent depression program or the relapse prevention program.
For the persistent depression program, patients who were found by the Structured Clinical Interview for DSM-III-R (SCID) (
32) to have four or more symptoms of major depression (N=228) were randomly assigned to one of two treatment groups: a collaborative care intervention, in which a psychiatrist worked with the primary care provider to improve antidepressant treatment for depression, or care as usual—the control group (
4). In the relapse prevention program, patients who had recovered from depression but were at high risk for relapse (N=387) were identified and also randomly assigned to one of two treatment groups: a relapse-prevention intervention with a depression specialist or care as usual—the control group (
30). In this article, "intervention" is the term used for special interventions rather than care as usual.
Exclusion criteria included a score of 2 or more on the CAGE alcohol screening questionnaire, the conditions of pregnancy or breast-feeding, a plan to disenroll from GHC, active treatment by a psychiatrist, limited command of English, and recent use of lithium or antipsychotic medications. The study protocol was approved by the institutional review boards of the University of Washington and GHC, and all participants signed a written consent form.
Patients assigned to care as usual received treatment for depression from their regular primary care physician. This treatment generally involved prescription of an antidepressant by their primary care provider, two to four follow-up visits over six months, and in some cases referral to a GHC mental health specialist. All participants could self-refer to GHC mental health providers.
Measures
Participants were assessed at baseline before randomization and at six-month follow-up by a trained interviewer blinded to the patients' randomization status. Five baseline measures were selected, and a subset of these was included in the follow-up assessments. The baseline measures were demographic information, including age, gender, ethnicity, employment, and household income; a 20-item depression scale derived from the Symptom Checklist-90 (SCL-90) (
33), a scale that has been used in a number of studies of primary care and has been found to have high reliability and validity (
4,
30,
34); the current and past depression modules of the SCID (
32,
34); seven items from the NEO Personality Inventory neuroticism scale (
35) that have been found to predict persistence of depressive symptoms in a primary care population (
36); and a chronic disease score, a measure of chronic medical illness derived from the patient's use of prescription medications over a six-month period (
37).
We assessed patients' willingness to pay for depression treatment in primary care by asking the following question: "Assume for a moment that you had no health insurance but that there was a treatment that would completely eliminate the symptoms of depression. How much money would you be willing to pay each month for a six-month treatment?" Respondents were given continuous response choices from $0 to $400 as well as more than $400 per month.
Interviewers received three hours of training before the first interview, plus individual practice sessions with a supervisor—a master's-level clinician with extensive training in structured interviews. Each interviewer was tested against either the supervisor or the project director during a practice interview, as well as during a study interview; reliability exceeded 80 percent for each interview question.
Analyses
We used t tests and chi square tests to compare baseline differences between study participants from the persistent depression program and those from the relapse prevention program. We used multiple regression analyses to estimate the association of demographic and clinical factors with willingness to pay. We first tested a number of predictor variables, including age, gender, ethnicity, employment status, household income, chronic disease score, score on the NEO Personality Inventory neuroticism scale, baseline depression severity as measured by the SCL-90, depression program (persistent depression or relapse prevention), and intervention status (intervention or care as usual). For the final models, we omitted variables that were not found to be significantly associated with willingness to pay. Age, gender, chronic disease score, household income, and depression program (persistent depression or relapse prevention) were included in the models, regardless of statistical significance, because of their potential confounding effects on willingness to pay.
We used analyses of covariance to determine whether there was a treatment effect at the six-month follow-up on willingness to pay. In this model, we controlled for age, gender, chronic disease score, depression program (persistent depression or relapse prevention), intervention status, household income, baseline willingness to pay, and baseline depression score. Means adjusted for the covariates were examined. We also examined the interaction of intervention status and depression severity on willingness to pay at six-month follow-up.
Results
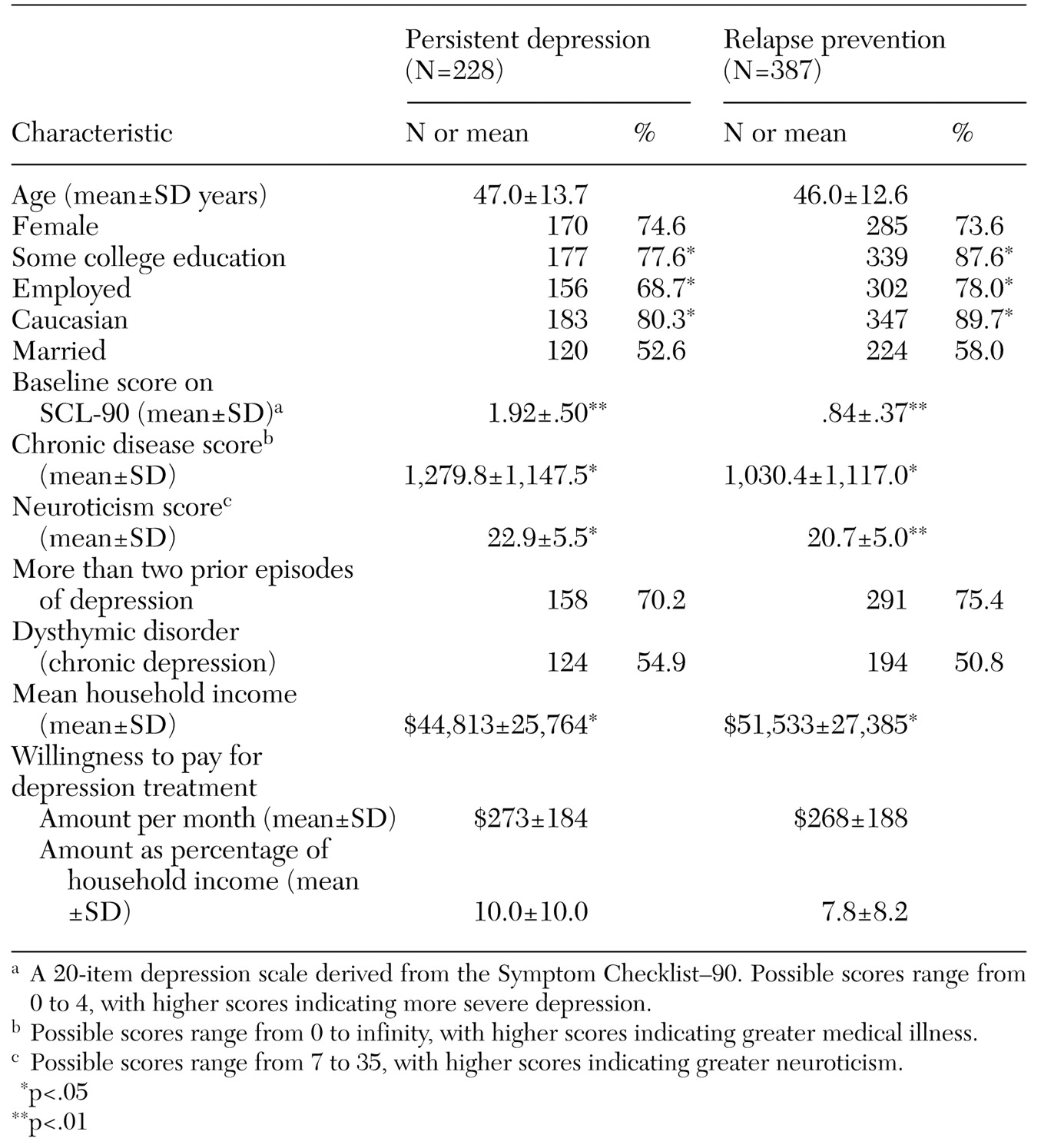
Participants in the persistent depression program showed significant differences from those in the relapse prevention program. As shown in
Table 1, those with persistent depression had a lower level of education and a lower household income and were less likely to be employed or to be Caucasian. They also had higher levels of depression, comorbid medical illness, and neuroticism.
The question about willingness to pay was generally well received by study participants. Only a small number of participants refused to answer the question or answered "do not know." Three percent of the answers to this question were missing at baseline and 10 percent at the six-month follow-up. At baseline, the mean±SD amount that all participants were willing to pay was $270±187 per month for a six-month depression treatment, and the median amount was $200 per month. At baseline, 13 participants (2.2 percent) reported their willingness to pay as zero, and 190 (31.8 percent) reported their willingness to pay as $400 or more. The mean willingness to pay was $273 per month in the persistent depression program and $268 in the relapse prevention program, as shown in
Table 1—representing 8.6 percent of the overall sample's mean household income. These amounts represented 7.8 percent of the mean income of the relapse prevention group and 10 percent for the persistent depression group. Baseline difference in willingness to pay between patients in the two depression programs was not statistically significant.
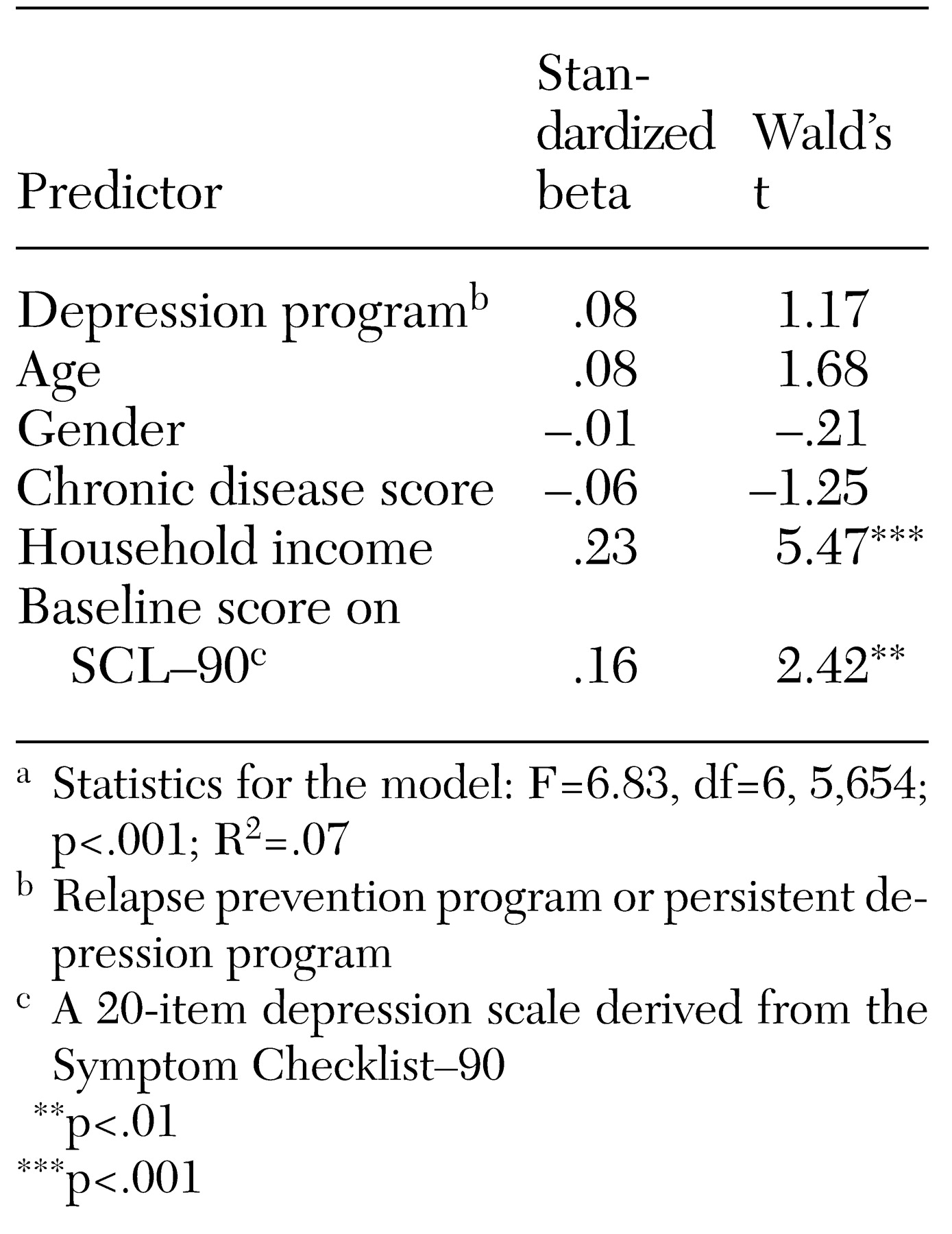
Participants with higher incomes and those with more severe depression symptoms at baseline were willing to pay significantly more, as shown in
Table 2. To illustrate the magnitude of these effects, we estimated the willingness to pay of participants at the 25th and 75th percentiles of household income and depression severity at baseline, using average values for all variables in our regression model. The estimated willingness to pay was $246 per month for those at the 25th percentile of depression severity, compared with $292 for those at the 75th percentile. The estimated willingness to pay was $230 per month for those at the 25th percentile of household income, compared with $292 for those at the 75th percentile. The estimates ranged from $222 per month for those with low incomes and low depression scores to $332 for those with high incomes and high depression scores.
For all participants, the mean monthly willingness to pay decreased from $270±186 at baseline to $214± 174 at six months. Neither the type of treatment—intervention or care as usual—nor the interaction between participants' severity of depression and the type of treatment they received was a significant predictor of willingness to pay at six months.
Discussion
At baseline, the participants in our study were willing to pay a mean of $270 per month for depression care; this amount is almost three times greater than that reported for antihypertensive therapy in the same HMO (
15) and is roughly comparable to the amount reported for treatment of asthma, estimated to be between $200 and $350 per month (
38), and for treatment of psoriasis, estimated to be $150 to $270 per month (
39). In our study, the mean amount that participants were willing to pay for depression treatment corresponded to 9 percent of the sample's mean household income. This proportion is somewhat lower than that found for a treatment that would eliminate symptoms of arthritis—17 percent of household income (
21). Patients may have greater willingness to pay for treatments of conditions with high symptom burden—such as depression, arthritis, or asthma—than for relatively asymptomatic conditions such as hypertension (
15) or for preventive services such as colorectal cancer screening (
40).
The amount that our participants were willing to pay was substantially greater than the actual costs of depression treatment provided to the intervention patients in this study, about $120 per month over six months (
5). It is also greater than the cost of depression care for adults who are treated for depression in the HMO used in the study (
41), greater than cost estimates from previous quality improvement studies for depression in our HMO (
11), and higher than the typical cost of antidepressant medications. We used a method developed by Lave and colleagues (
42) and Simon and associates (
43) to estimate the amount our participants were willing to pay for a depression-free day; the amount was approximately $18. This result is based on calculating that a decrease from our participants' mean SCL-90 depression score at baseline—1.26—to complete remission of depression symptoms—an SCL-90 score of about .5, which corresponds to a score of less than 7 on the Hamilton Depression Rating Scale—would result in a gain of about 91 depression-free days over six months. This estimate is well within the range of cost-effectiveness estimates of $10 to $20 per depression-free day that has been established in quality improvement trials for depression in primary care (
43).
A finding consistent with previous research and with our first hypothesis was that willingness to pay was strongly associated with household income. We adjusted for differences in household income in our multivariate analyses, and we want to make it clear that we are not advocating for willingness to pay as a method of allocating resources among individuals. Because psychiatric disorders such as depression may be more severe among those with lower incomes and because there is a strong association between income and willingness to pay, we caution against using consumers' willingness to pay as the only consideration when making decisions about resource allocation.
As we also hypothesized, willingness to pay was significantly associated with the severity of depressive symptoms. Over the six-month study period, willingness to pay decreased along with participants' depression severity (
4). The strong association between willingness to pay and the severity of depressive symptoms at baseline and over time suggests that willingness to pay may be a reasonably good proxy for health status preferences, or the value patients place on their health status.
We did not observe significant effects of treatment type (intervention or care as usual) on willingness to pay at six months, and we believe that two factors may have affected, in opposite directions, the willingness to pay of participants in the intervention group. Participants in the intervention group experienced a significantly greater reduction in depression symptoms than did patients in care as usual (
4,
30), which may have reduced their willingness to pay for depression treatment. On the other hand, those in the intervention group were provided with systematic education about the value of depression care and a more organized model of depression care than were participants in care as usual. Intervention-group participants reported greater satisfaction with depression care at six months (
4), and their treatment experience may have increased their perceived value of depression treatment and thus their reported willingness to pay for depression treatment at six months.
In regression models predicting willingness to pay at the six-month follow-up, we did not find a significant interaction between treatment type and depression severity—a finding suggesting that the type of treatment did not alter the relationship between depression severity and willingness to pay and that the two factors described above may operate independently.
Our study of willingness to pay for depression care was exploratory and has a number of limitations: First, the sample consisted of patients who had received new prescriptions for antidepressants in primary care and who agreed to participate in a trial of quality improvement for depression. Second, this sample may not be representative of other depressed primary care patients. In our analyses, we combined patients from two different programs, persistent depression and relapse prevention, who had been randomly assigned to intervention or to care as usual. We believe that this combined sample represents the spectrum of patients in treatment for depression in the four nonacademic primary care clinics; in our regression analyses we adjusted for depression status and for the two types of treatment. Our combined sample included 228 patients with persistent depression and 387 patients with only residual symptoms of depression, with the second group being those in the relapse prevention program. In this study, "baseline" measures were taken after patients had received from six to eight weeks of treatment. The willingness to pay $270 per month at baseline thus reflects the fact that many patients had already experienced a substantial reduction in depressive symptoms. Among the 83 patients in the group with persistent depression who met research diagnostic criteria for major depression (
31) after six to eight weeks of treatment in primary care, the mean willingness to pay was slightly higher—$278±$188 per month.
Our study did not use the willingness-to-pay method to assess participants' valuation of the type of depression care they received, either the intervention or care as usual. Rather, we asked a hypothetical question about willingness to pay for a depression treatment that would completely eliminate all symptoms of depression. However, existing treatments for depression generally result in full remission among only about 50 percent of treated patients (
1), and our question about willingness to pay did not allow us to estimate willingness to pay for partial treatment results. Other studies have demonstrated that willingness to pay for treatment is associated with the expected reduction in symptoms (
24,
45). Judging from this finding, our estimates of willingness to pay are probably higher than the actual willingness to pay for the depression treatments we evaluated in this study.
Because of the hypothetical and limited nature of our question about willingness to pay, we do not know whether participants' self-reported willingness to pay is an accurate estimate of their true willingness. Other studies have found that contingent valuation methods to assess willingness to pay may overestimate subjects' real willingness (
44). Because willingness to pay was not a primary study outcome, we had to limit the length and complexity of our question to a simple payment-card question. We asked participants "How much would you be willing to pay each month?" but did not specifically inquire about the maximum amount that they would be willing to pay, as recommended by some experts. To give a valid assessment of their willingness to pay, respondents would need perfect information about depression; the quality, effectiveness, risks, and side effects of treatment; and treatment alternatives. More comprehensive assessments of willingness to pay (
24,
31,
46) might result in different and possibly more valid responses than did our simple question.
Despite these limitations, we feel that the assessment of willingness to pay to estimate the value of treatment for common mental disorders appears promising, and we believe that further research in this area is warranted. The willingness-to-pay method may allow consumers to express preferences for treatments that could be important to researchers, clinicians, and health policy makers. Patients may be better able to understand relatively concrete questions about money than questions reflecting utility measurement techniques, such as time trade-off or standard gamble. The vast majority of our patients completed the willingness-to-pay question—97 percent at baseline and 90 percent at six months. This response compares favorably with that in another recent trial of quality improvement for depression treatment in primary care, which had a relatively high rate of nonresponse (about 25 percent) to brief time-trade-off and standard-gamble questions used to assess health status preferences (
47,
48,
49).
Our findings suggest that depressed primary care patients place a high value on treatments that would relieve them of the symptoms of depression. Treatments that can accomplish this goal for a majority of patients are available (
1,
50), but many depressed primary care patients do not receive such treatments (
51,
52), and efforts to improve access to effective depression care may be of substantial value. Barriers to effective depression treatment in primary care include limited insurance coverage for such treatments—for example, limited reimbursement for antidepressants, psychotherapy, and depression care management under Medicare. Discrepancies between consumers' and insurers' willingness to pay for effective mental health treatments could result in a growing demand for true parity for mental health treatments.