Advance care plans document a person's treatment choices or identify a proxy for health care decisions should the individual become too critically ill to make decisions. Proponents of advance care planning believe that such directives promote patient autonomy, dignity, and comfort in the use of life-sustaining medical treatments. The Patient Self-Determination Act (PSDA) of 1991 requires that health care facilities receiving Medicare or Medicaid reimbursement, including nursing homes, inform patients of their right to engage in treatment decisions (
1). The prevalence of advance directives among nursing home residents, such as do-not-resuscitate (DNR) orders, increased notably after the passage of the act (
1–
3). However, documentation of advance care plans is found to vary considerably across subgroups of nursing home residents, suggesting possible disparities associated with socioeconomic status or race (
2–
5).
It is estimated that between 10% and 25% of U.S. nursing home residents have a serious mental illness, including schizophrenia, bipolar disorder, and other psychosis (
6–
8). Federal law mandates that persons with serious mental illness should not be admitted to nursing homes unless they show extensive general health care needs that justify institutionalized nursing services above and beyond their mental illness (
6,
9). Therefore, in addition to needing appropriate psychiatric care, nursing home residents with serious mental illness tend to need the same general medical and end-of-life services as other residents (
10).
Nevertheless, the appropriateness or quality of the nursing and end-of-life care received by residents with serious mental illness has not been a focus of study. Specifically, appropriate documentation of medical advance care plans has not been studied for nursing home residents with serious mental illness, who for several reasons might be more vulnerable than other nursing home residents in making informed choices about treatment. First, nursing home staff generally lack training to care for persons with serious mental illness (
11) and may be uncomfortable with treating them because of concerns about possible dangerous and disruptive behaviors (
7) and because staff may harbor stigma toward this population of residents (
12). Second, health care providers may assume that persons with serious mental illness inevitably lose decisional capacity to participate in advance care planning (
13,
14); this is a common misconception that has proved stigmatizing (
15–
18). Finally, persons with serious mental illness who are under legal guardianship are likely to be prohibited from self-determining their medical and psychiatric treatments (
19,
20). Taken together, these factors may place nursing home residents with serious mental illness at a disadvantage in advance care planning.
This study analyzed data from a nationally representative sample of nursing home residents to determine the association between presence of serious mental illness and documentation of several components of medical advance directives. We hypothesized that nursing home residents with serious mental illness are less likely than other residents to have written advance directives.
Methods
Data source
The data came from the public-use resident file of the 2004 National Nursing Home Survey (NNHS) that was conducted by the U.S. Centers for Disease Control and Prevention (
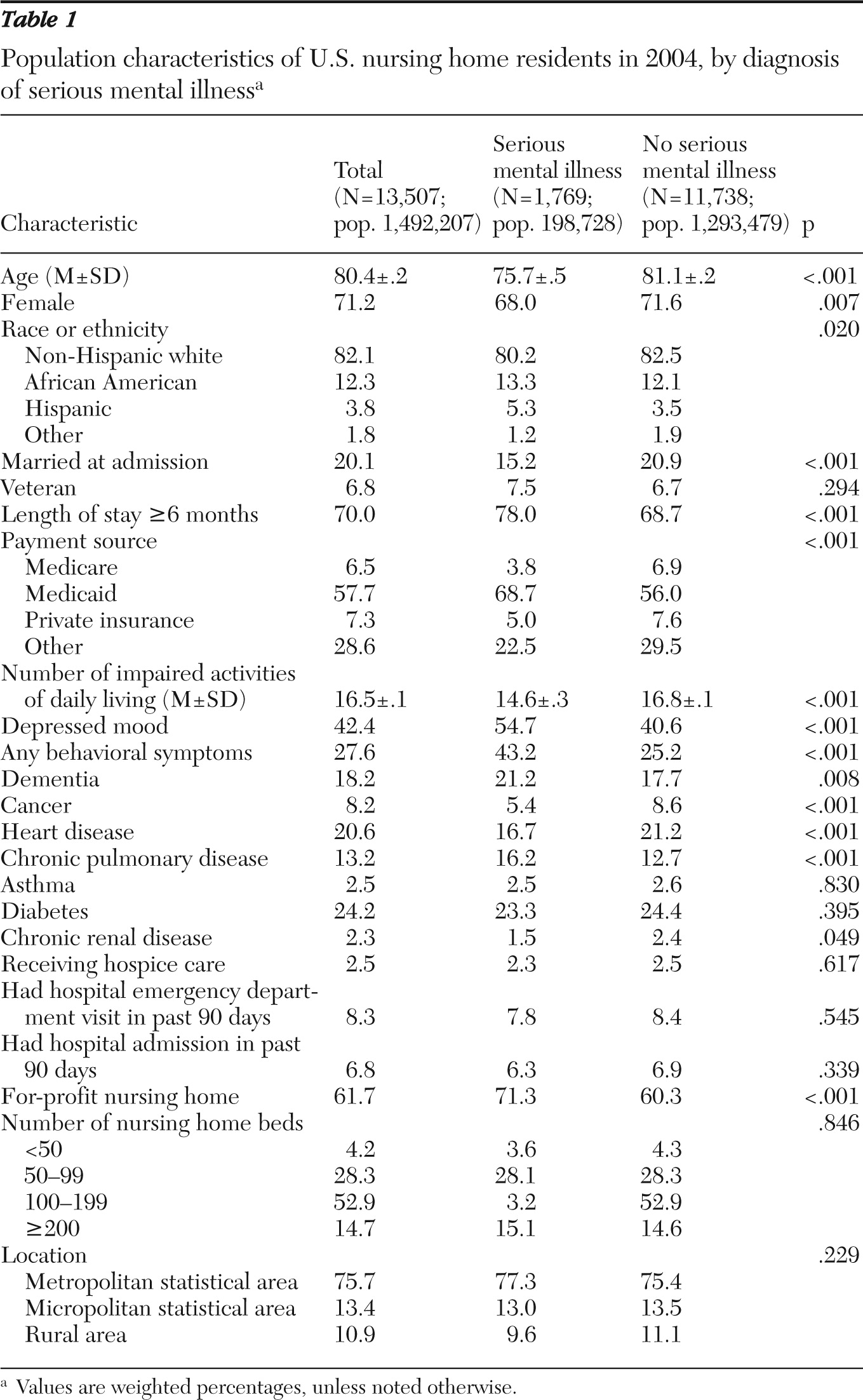
21). The 2004 NNHS contains a nationally representative sample of U.S. nursing homes, including their residents and services, and provides patient-level information on demographic and functional characteristics, length of stay, primary diagnosis and up to 15 secondary diagnoses coded by the
International Classification of Diseases, 9th Revision, Clinical Modification (
ICD-9-CM) system, services received, and payment sources. Facility information includes geographic location, profit status, and number of beds. The resident data were obtained through personal interviews with facility administrators and designated staff members, who used medical charts and assessment records to answer questions about residents. Nursing home residents were not directly interviewed. This study was approved by the institutional review board of the University of Iowa.
The survey involved a stratified two-stage probability design (
22). The first stage was selection of nursing homes stratified by metropolitan area status, bed size category, and other facility characteristics. Nursing homes were finally selected by systematic sampling, with the probability proportional to bed size. The second stage, sampling of current residents, was carried out by on-site interviewers. A sample of up to 12 current residents per facility was selected for final interview. The response rate was 81% for the first-stage sampling (that is, 19% of sampled nursing homes did not participate for reasons such as being out of business during the survey period) and 96% for the second-stage sampling (that is, data for 4% of sampled residents were not collected for reasons such as lack of consent), resulting in an overall response rate of 78%. The final sample included 13,507 residents in 1,174 nursing homes.
Advance care plans
The outcome variables of interest were whether sampled residents had any of the following advance care documents: living wills, DNR orders, do-not-hospitalize (DNH) orders, and orders restricting feeding, medication, or other treatments. Following guidance of McAuley and Travis (
3), we further categorized these orders into two types: basic advance directives (living wills and DNR orders), which usually are developed on the basis of general knowledge about end-of-life care but have little impact on the resident's current treatment, and progressive advance directives (DNH orders and treatment restrictions), which are considered progressive because they are beyond the general decision-making framework for end-of-life care and typically are derived from personalized futility assessment and have relatively immediate impacts on the resident's current care (
3). Finally, an overall summary variable was created for each resident to indicate the presence of any of the two types of advance directives (1, yes; 0, no).
Serious mental illness and covariates
The key independent variable for analysis was diagnosis of serious mental illness (schizophrenia, bipolar disorder, or other psychosis) identified through the resident's primary diagnosis and all secondary diagnoses with
ICD-9-CM diagnostic codes 295, 296.0, 296.1, 296.4–296.9, 297, and 298. We also defined a set of resident- and facility-specific covariates that, according to previous studies (
2–
5), may be associated with advance care documents. Resident covariates were age in years (<65, 65–84, and ɥ85), female gender (yes or no), race (nonwhite versus white), marital status at admission (married or not), being a veteran (yes or no), length of stay (six months or more versus less than six months), payment source (Medicare, Medicaid, private, or other), and number of impairments in activities of daily living. The activities of daily living included bed mobility, transfer, dressing, eating, toileting, personal hygiene, and bathing; each component was coded in five categories from 0 (independent) to 4 (totally dependent), resulting in a total range of the aggregate activities-of-daily-living score of 0–28 (
22).
Resident covariates also included a set of indicator variables (coded 0 or 1) defining whether the resident had depressed mood, behavioral symptoms, and current diagnoses with dementia (ICD-9-CM codes 46.1, 290.0–290.4, 291.2, 292.82, 294.1, 331.0, 331.1, 331.7, 331.82, and 331.9), cancer (codes 140–239), heart disease (codes 389.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 416, 425, 428, and 440), chronic pulmonary disease (codes 491, 492, 494, 496, 506.4, and 518.2), asthma (code 493), diabetes (code 250), and chronic renal disease (codes 581 and 585); whether the resident was receiving hospice care; and whether the patient had visited a hospital emergency department or had a hospital admission in the past 90 days. Facility covariates included profit status (for profit versus nonprofit), number of beds (<50, 50–99, 100–199, and ɥ200), and geographic location (metropolitan, micropolitan, and rural area).
Analyses
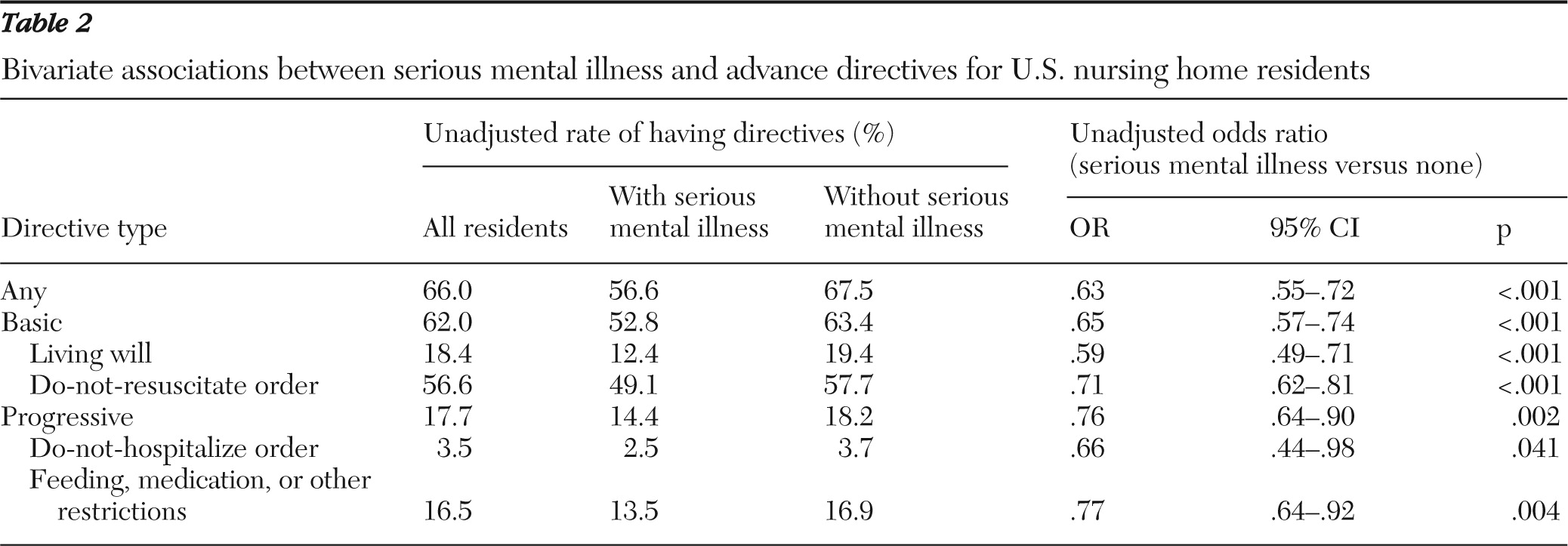
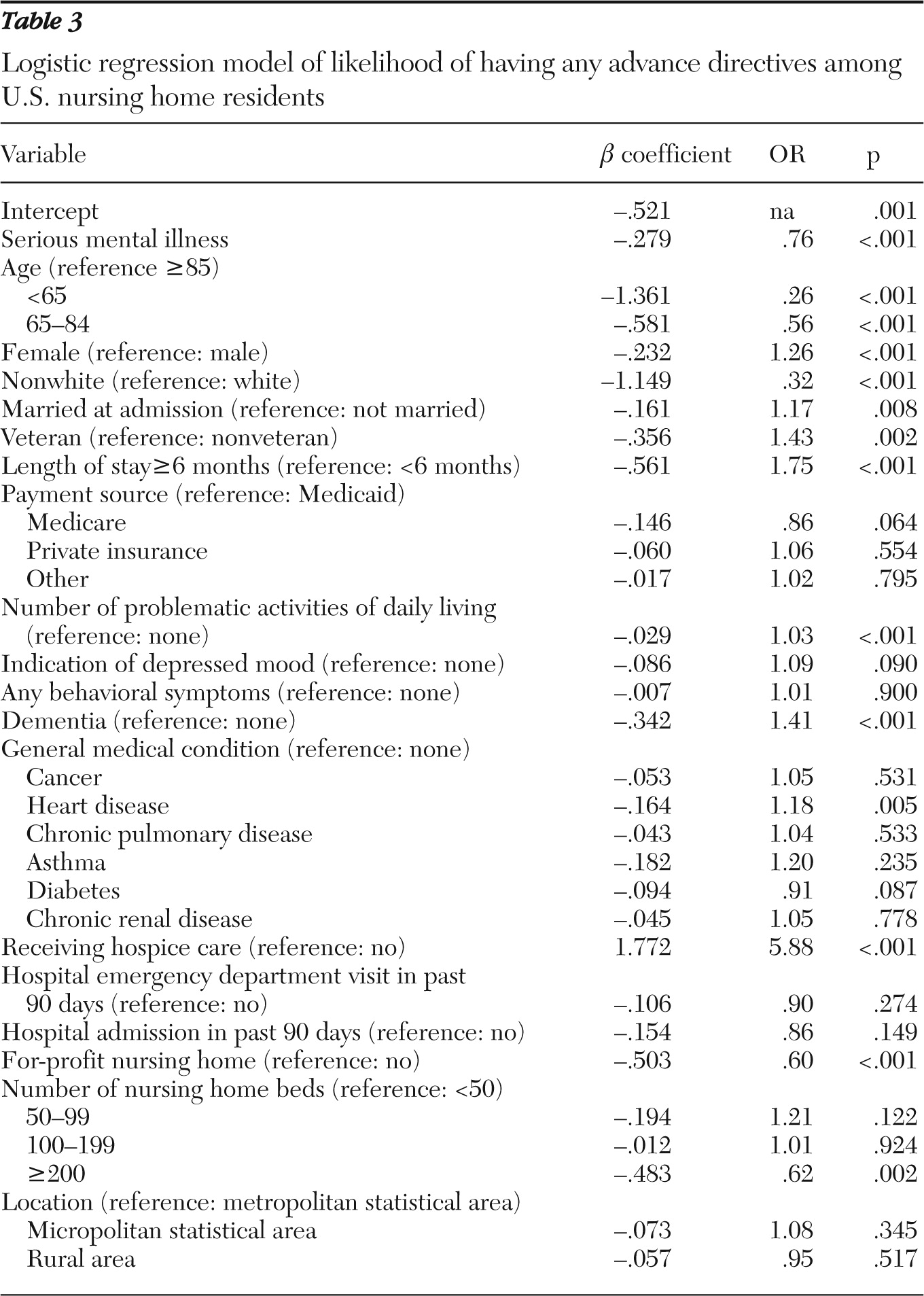
We performed bivariate and multivariate analyses, both of which accounted for the complex sampling methodology, including stratification, clustering, and weighting. Therefore, our analyses pertained to the population of U.S. nursing home residents. In bivariate analyses, we compared individual and facility characteristics between the two groups, using t tests for continuous variables and chi square tests for categorical variables. For each type of advance directives, we also used 2×2 contingency tables to calculate unadjusted odds ratios (ORs) of patients with serious mental illness.
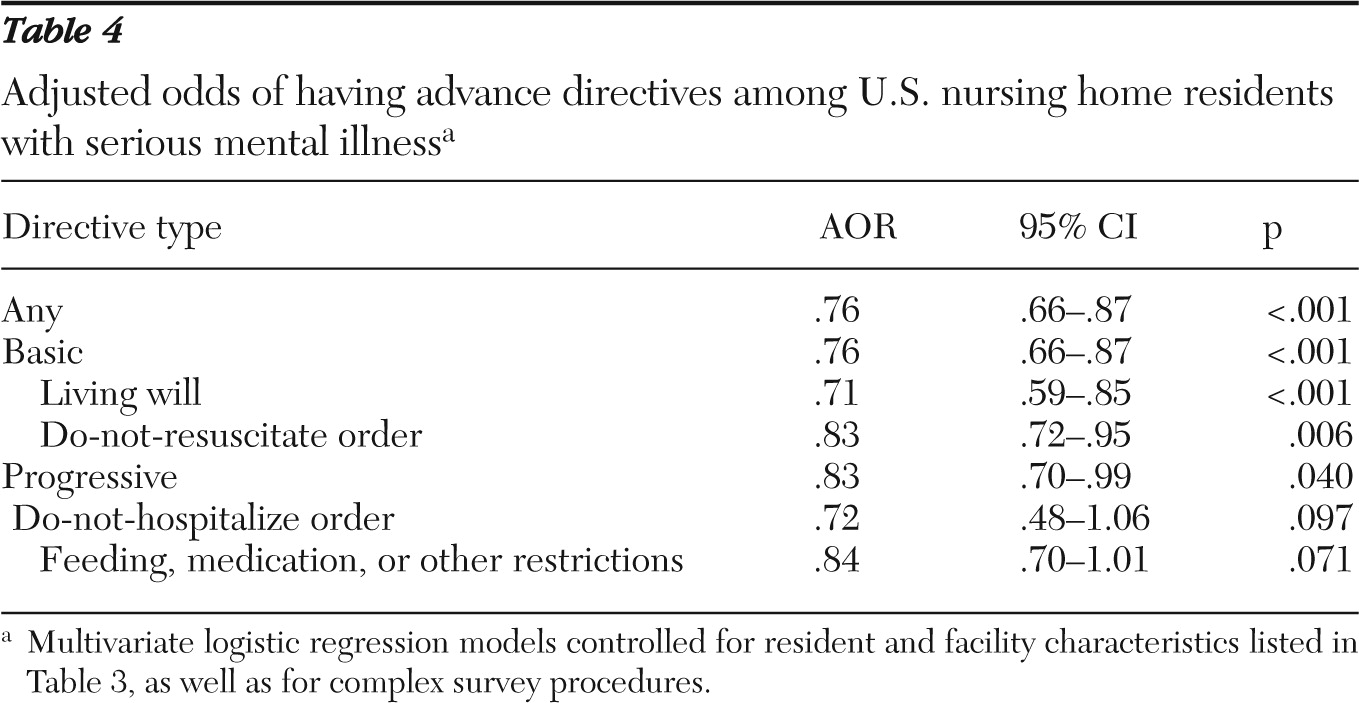
In multivariate analyses, we estimated separate logistic regression models for having any and each type of advance directive. Each model had presence of serious mental illness as the primary independent variable and controlled for the resident and facility covariates described above. All analyses were performed with the survey estimation routines available in Stata, version 8.
Discussion
Using a large and nationally representative survey of nursing home residents, this study revealed that residents with serious mental illness were less likely than other residents to have written medical advance directives, including living wills, DNR or DNH orders, and treatment restrictions concerning feeding, medication, and other treatment. After controlling for resident and facility covariates that may affect advance care plans, we estimated that serious mental illness was associated with 15%–30% reduced odds of having written advance directives.
The PSDA of 1991 requires that federally funded health care institutions inform competent patients of their rights to make health care decisions, including accepting or refusing treatment and completing advance directives. To our knowledge, however, although end-of-life care planning and preferences have been studied in the nursing home setting (
1–
5), no research is available to illustrate this issue for nursing home residents with serious mental illness. Given the relatively high prevalence of serious mental illness in nursing homes (<10%) (
6–
8) and the high level of physical disability and medical comorbidities associated with it (
10), nursing home residents with serious mental illness are likely to represent a group of high priority for implementing advance directives. This study presented a first comparative analysis of common types of advance directives for a group of previously neglected persons and suggests that this group, compared with other nursing home residents, had lower rates of establishment of all examined directives.
It is important to acknowledge that although persons with serious mental illness may pose unique challenges to nursing home staff with regard to issues of competency and medical decision making, the PSDA does not exclude persons with mental illness from health care self-determination. The act holds a legal presumption that all persons are competent to make decisions unless judicial evidence exists to invalidate their directives (
23).
Although there is no gold standard for defining the capacity or competency for completing a directive, an evidence-based instrument for assessing decisional capacity has been developed and is widely used with patients with mental and neuropsychiatric disorders. The instrument, developed by Grisso and Appelbaum (
16), incorporates widely accepted legal, ethical, and clinical standards into four models of competency that include understanding disclosed information, appreciation of the implications of the information for one's own situation, reasoning with the information in a decisional process, and expressing a choice. A study by Carpenter and colleagues (
15) reported that although community-dwelling patients with schizophrenia performed more poorly in these capacities than persons without mental illness, their reduced capacities can be brought back to normal by an educational intervention during the informed consent process. Palmer and colleagues (
18) found that compared with a control group without serious mental illness, persons with schizophrenia showed only minor impairment in understanding and no impairment in appreciation or reasoning with information. Other studies (
16,
17) of community-dwelling patients showed similar findings, and, taken together, they provided the evidence base that the legal presumption of competency to complete advance directives is reasonable, even for patients with serious mental illness (
23).
Nursing home residents with serious mental illness are more functionally and cognitively disabled (
6,
9) than persons with serious mental illness who are living in the community, and as a group, those residing in nursing homes may be more likely to be decisionally impaired. However, cognitive impairment and its associated decisional incapacity are common in the general nursing home population (
24), and those residents often suffer from dementia or other illnesses that prevent them from participating in medical decisions. Therefore, although we did not have data comparing the decisional capacity between residents with and without serious mental illness, it does not seem likely that the potential cognitive impairment of those with serious mental illness is a primary explanation for their lower rate of written advance directives.
The choice of not forgoing more aggressive treatment through advance directives is a legitimate one as long as it is made by a fully informed nursing home resident. However, the issue we raised with this study is whether residents with serious mental illness tend to be neglected or less informed than other residents when facing medical decision making or whether serious mental illness interferes with communications between the resident and the physician (or other caregivers) in the process of discussing treatment options and preferences. We are not aware of any evidence that residents with serious mental illness prefer more aggressive medical treatment compared with the preferences of general nursing home residents. Therefore, we suspect that our findings reflect disparities in medical decision making caused by such factors as provider bias rather than actual differences in expressed care preferences.
In general, the functioning of U.S. nursing homes and their care and staff structures are organized around the management of chronic medical conditions and functional disabilities of elders rather than care specifically for persons with psychiatric disabilities (
25). Members of nursing home staff usually do not receive appropriate training that emphasizes mental health issues (
11). As a result, they may be unable to appropriately serve persons with mental illness or communicate with them proactively about available treatment options, particularly when the residents experience active psychosis, display aggressive behavior, or have difficulties in communication. Nursing home staff may also hold negative beliefs that those with serious mental illness are “out of touch” and automatically exclude them from participating in health care self-determinations. Further work, therefore, is needed to explore the potential role of patient-caregiver relationships in explaining the decreased rate of written advance directives among residents with serious mental illness.
Strengths of this study include the large and representative sample of nursing home residents, their high response rate, and the collection of data for advance directives, serious mental illness, and medical comorbidities based on medical chart and other records, such as the Minimum Data Set (
22). This study also had several limitations. First, the data were cross-sectional, and thus our estimates represent associations but not causal effects. Second, although the multivariate analyses controlled for detailed resident and several nursing home covariates, the public-use data do not contain a fuller set of facility variables; as a result, omitted facility covariates may mediate a part of the estimated differences. Finally, this study did not analyze other advance directives, such as surrogate decision maker (such as next of kin, family member, or friend), power of attorney for health care, or legal guardianship because these data were not collected in the survey. Persons with serious mental illness are more likely to be under court-appointed legal guardianship, which would obviate their self-determination of medical treatment (
20). Therefore, their lower rates of advance directives in this study may be partially explained by their increased use of legal guardians. However, health care proxies have the authority to initiate and sign living wills and other advance directives for the patients. Thus it also seems to be true that disparities in advance care planning persist for nursing home residents with serious mental illness despite their potentially higher rate of surrogate decision making.