Coercive interventions and efforts to reduce or eliminate them are the oldest issue in psychiatric institutions. The beginning of modern psychiatry has been dated to the liberation of the insane from their chains by Pinel in 1793 in the Salpétrière asylum in Paris (
1). Most psychiatric hospitals have not succeeded in abolishing coercive interventions such as seclusion and restraint (
2–
4). In particular, the treatment of patients with violent or self-harming behavior is frequently accompanied by an ethical conflict between patients' autonomy and physical and mental integrity on the one hand and the requirement to prevent harm on the other. A sound scientific evaluation is urgently required because of the high impact of coercive measures on patients' autonomy, their subsequent traumatization, and the effect of these measures on patients' attitudes toward psychiatric services (
5).
The first review of this topic, in 1994, stated that seclusion and mechanical restraint “can have deleterious physical and (more often) psychological effects on patients” (
2). After a series of newspaper articles in 1998, several bills were introduced in the U.S. Congress to monitor or restrict the use of seclusion and restraint in psychiatry (
6). It was required that coercive interventions constitute a “last resort” to be used only when other less restrictive approaches have failed (
6). Authors of European guidelines (
7,
8) and recommendations (
9,
10) have come to similar conclusions. Lately, various organizations have aimed to restrict the use of seclusion and restraint. The “least restrictive alternative” is recommended (
10–
15).
However, there is some controversy over which measure is least restrictive—seclusion or mechanical restraint. Conclusive evidence is not available. In several countries only a single coercive intervention is used or even legally allowed, whereas in other countries the same intervention is regarded as inhumane or unsafe (
16,
17). Controlled studies that evaluate the value of seclusion and restraint of people with serious mental illness have repeatedly been demanded (
5,
18). Ethical and methodological difficulties of randomized controlled trials of coercive interventions that hindered research efforts for a long time and have only recently been addressed (
19).
The purpose of this study was to compare the psychological impact of seclusion and mechanical restraint by using a randomized controlled design.
Methods
Setting
The study was conducted between March 2004 and March 2006 at the Center for Psychiatry Suedwuerttemberg, Ulm University, a psychiatric hospital in southern Germany serving a catchment area of 480, 000 people. In Germany both interventions—seclusion and mechanical restraint—are legally permitted, although most hospitals prefer only one of the two interventions. At the study site both interventions have been used for many years without obvious preference. The legal premises do not differ significantly from those in other countries (
17). The interventions used in this trial required no special permission.
Design
Seclusion and mechanical restraint were compared by means of a comprehensive cohort study (
20,
21). The design consisted of two randomized and two nonrandomized cohort arms, which allowed us to compare the two randomized groups and to achieve a high internal validity. Moreover, the randomized arm of one intervention could be compared with the nonrandomized arm of the same intervention, which allowed us to check the external validity of the obtained results (
19).
Randomization procedure
Because coercive measures are used primarily in emergency situations, the “envelope-method” was chosen. Randomization was stratified, and each stratum referred to one ward. The strata were balanced into blocks of ten. The envelopes on each ward were serially numbered. If a coercive measure seemed inevitably necessary, the next envelope was opened and the respective measure was carried out.
Ethical considerations
The study was approved by the ethical review board of Ulm University. After a complete description of the study, written informed consent was obtained from the patients. Patients generally were not capable of informed consent at the time of the intervention because of their mental state. Because coercive measures are coercive by definition, patients could not be expected to consent to these interventions at the time of the intervention. The informed consent was not related to randomization procedure or to the intervention itself (which was coercive in its nature) but to participation in the subsequent study, which involved questionnaires and interviews (
19). As in studies in emergency medicine, baseline data were collected before consent was obtained (
22). Precollected data of those who refused to consent were later deleted. The ethical problems of informed consent, capacity, and randomization are described in detail elsewhere (
19).
Inclusion criteria
To be eligible patients had to be 18 years or older and have a DSM-IV diagnosis of schizophrenia, affective disorder, or personality disorder. Patients were excluded if they refused to consent, if they had already been enrolled in the study during a previous admission, or if they had requested seclusion or mechanical restraint on a voluntary basis. Other exclusion criteria were language barrier, severe and persistent psychopathological symptoms, and inability to recall details of the index intervention. Patients were excluded from randomization for ethical reasons if the responsible psychiatrist or the patient definitely preferred one intervention for any reason. Patients excluded for the above reasons were included in the cohort arms of the trial.
Interventions
The study focused on the index intervention—that is, the first coercive measure used during the admission. Seclusion was defined as involuntary confinement of a person in a room from which the person is physically prevented from leaving (
23). During seclusion patients were observed every ten to 15 minutes through a window in the door.
In this study mechanical restraint was defined as five-point restraints in a bed (both arms, both legs, and a hip belt) (
18). According to internal hospital guidelines, patients had to be constantly monitored face-to-face during mechanical restraint. If this was not possible, patients had to be monitored at least for 15 minutes of each hour of restraint and by sight check every ten to 15 minutes for the remainder of each hour. Chemical restraint was not examined as a separate intervention, because it is frequently administered along with seclusion or mechanical restraint and was considered a confounding variable.
For each index intervention, a semistructured interview was conducted with the patient to establish mutual trust. The patient was asked to describe the coercive intervention, and the CES was administered. The interview was conducted four weeks after the intervention (median of 27 days for both intervention groups). If patients had difficulties concentrating, the interviewers helped them focus on the index intervention. Interviews were conducted by three individuals. One interviewer (JB) worked as a consultant on one of the admission wards and interviewed most of the patients. The two other interviewers were social workers on rehabilitation wards. These two interviewers were not involved in applying coercive measures; however, JB was involved in the treatment as supervisor.
Outcomes and instruments
It is critical to define a reasonable primary outcome variable for a randomized controlled trial of coercive measures. Safety aspects, reduction of psychopathological symptoms, or duration of the coercive measure were not considered appropriate outcome variables, because adverse events are rare, the interventions are not primarily therapeutic in nature, and their duration is affected by other factors, such as medication.
From the user's perspective, coercive measures are not primarily a problem of safety or efficacy but a problem of human rights (
10,
24). Thus we used the score on the Coercion Experience Scale (CES) (
25) as a primary outcome variable. This instrument was developed for the study (
25). The CES assesses restrictions of human rights from the patient's' point of view; it also assesses several stressors experienced during coercive measures by means of a self-rating questionnaire. The patients were asked to rate these stressors on a 5-point Likert scale (not at all, a little, moderate, severe, and extreme). The CES consists of 29 items (for example, “I felt my dignity taken away,” “I couldn't move freely,” “I had to obey the orders of others,” “I was afraid I would be killed,” “I feared the measure would last forever,” “I was not able to sleep well,” “I suffered pain”), which could be categorized into six factors (humiliation, adverse physical effects, separation, negative environment, fear, and coercion). Values of the single items were summed to derive the subscale scores and the total score. The higher the total CES score or the subscale scores, the higher the amount of burden.
Because the number of items in each subscale varied, we improved the comparability of the subscales by transforming the total score and subscale score into a standardized ratio. This ratio was a quotient of the score divided by the number of items. For example, if the CES total score, in which 29 items are included, was 62, then the standardized ratio was 62/29, or 2.14. If the subscale score for adverse physical events (includes four items) was 15, then the standardized ratio was 15/4, or 3.75.
The six factors explained 55 % of the total variance. Cronbach's alpha ranged from .67 to .93, which can be interpreted as a high internal consistency. Convergent and discriminant validity were both highly significant (r=.79, p<.001 and r=−.38, respectively, p<.001) (
25).
Several secondary outcome measures were defined, and they are described below.
Global strain of the coercive measure.
After rating the CES items, patients were asked to estimate the global strain on a visual-analogue scale (from 0 to 100): “How stressing did you experience the measure in total, independent of the aspects mentioned above [in the CES]?”
Medication.
To ensure comparability of the individual medication on different wards, two researchers (JB and TS) independently rated medication as none given, low, standard, or high. Differences between the two raters were discussed until agreement was reached.
PANSS aggression score.
Scores on four items from the Positive and Negative Syndrome Scale (PANSS)—excitement, hostility, uncooperative behavior, and poor impulse control—were summed for an aggression score, ranging from 4 (no aggression) to 28 (extremely severe aggression) (
26).
Adverse events.
Patients' medical records were reviewed, and staff members were interviewed about whether negative incidents occurred during coercive measures. Adverse events were assessed as present or absent; if present, the type of adverse event was documented.
Other secondary outcome measures.
In the interview part of the questionnaire, patients were asked about their feelings during the intervention (for example, helplessness or anxiety). Because close monitoring of all patients after a coercive intervention was required, the duration of their sleep was documented in the records. In addition, the resident who was responsible for implementing the coercive intervention was required to record the reason for the intervention. CGI values were also obtained from patients' records.
Statistical analysis
To compare seclusion and mechanical restraint, a priori ordered hypotheses were established. This means that if the first hypothesis is significant, the second can be proven and the level of significance is still p≤.05. First, we hypothesized that there would be a significant difference in the CES total score between the seclusion and mechanical restraint groups for the entire sample—that is, when the randomly assigned patients and patients in the cohort arms were considered as a group. Second, we hypothesized that there would be a significant difference in the CES total score between the two groups randomly assigned to either seclusion or mechanical restraint. Thus the second hypothesis focused only on the randomized groups.
Both hypotheses were tested with Mann-Whitney U tests. The level of significance was set at .05.
STATISTICA for Windows (Software-System for data analyses), version 8.0. (
www.statsoft.com), was used for all analyses.
Results
Characteristics of patients
From March 2004 to March 2006, a total of 233 patients admitted to the three psychiatric units were informed of the study and asked to provide consent. A total of 108 patients consented (46%); 125 patients were excluded on the basis of the criteria described above. Reasons for exclusion were refusal to participate (N=32), diagnosis (N=22), enrollment in the study during a previous admission (N=22), discharge before the interview could occur (N=13), voluntarily requested coercive measure (N=12), language barrier (N=11), ongoing severe symptoms (N=9), and lack of ability to recall details of the coercive measure (N=4). One patient in the randomized mechanical restraint group and three patients in the nonrandomized seclusion group dropped out by withdrawing informed consent during the interview. One patient in the nonrandomized mechanical restraint group, who had to be interviewed as an outpatient because of early discharge, was too drunk to be interviewed. One patient in the nonrandomized seclusion group dropped out because of ongoing severe symptoms. She stated that her answers were forced by auditory hallucinations. Analyses were conducted with data from 102 patients. [The enrollment, randomization, and analysis are described in a CONSORT flow diagram, which is available as an online appendix to this article at
ps.psychiatryonline.org.]
Because the dropout rate of 5% (six patients) was considered very low, no intention-to-treat analysis was carried out.
The trial had to be stopped in March 2006 because the regulatory body (Ministry of Social Welfare) advised that patients in mechanical restraint must be continuously monitored, referring to a recommendation of the European Committee of Prevention of Torture. Continuous monitoring would have changed the study conditions, because the hospital guidelines permitted exceptions to constant and face-to-face monitoring during mechanical restraint. Therefore, we finished the trial with only half the number of patients that would be required for the analyses to have sufficient statistical power. Thus the analyses must be considered as exploratory.
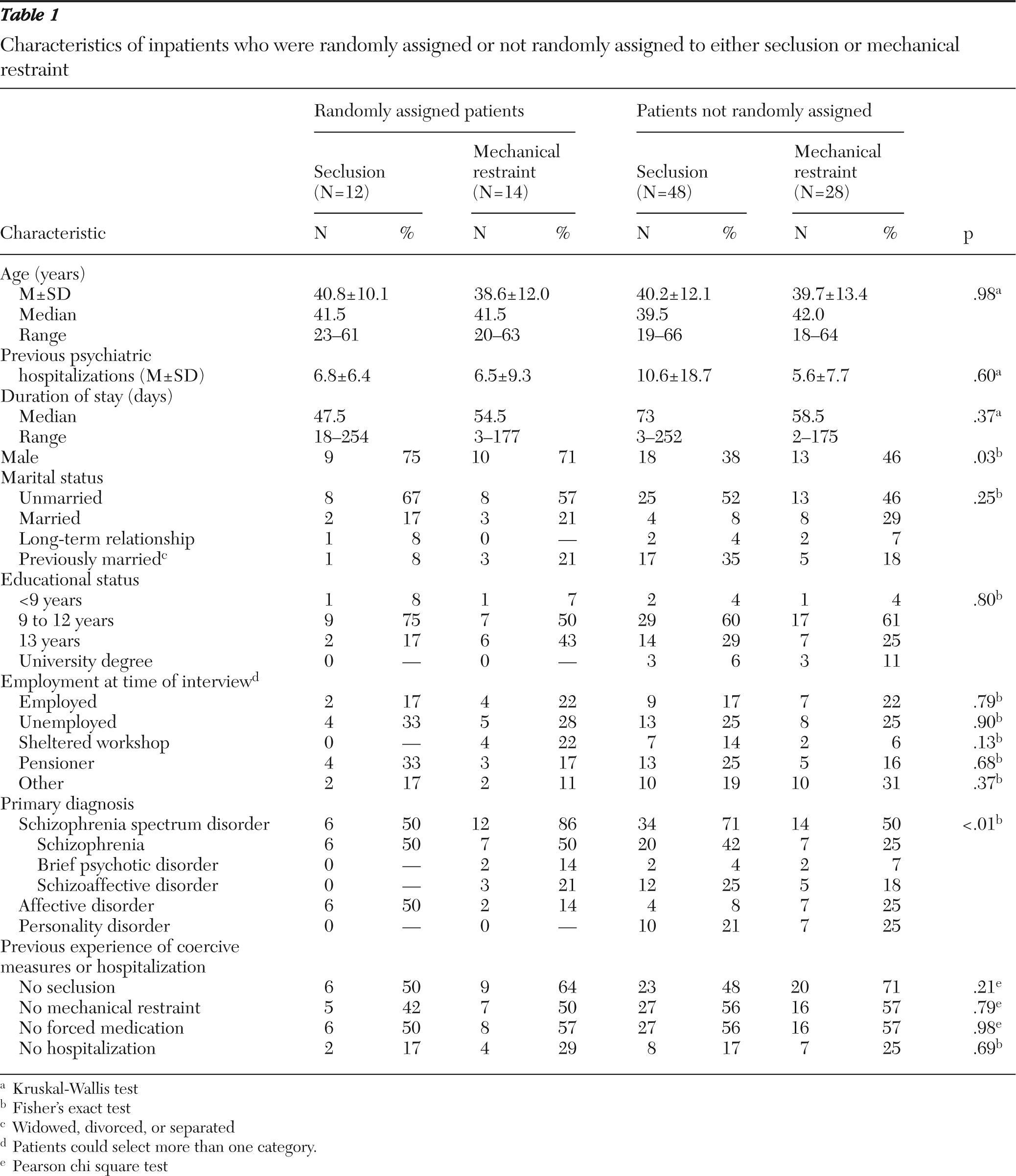
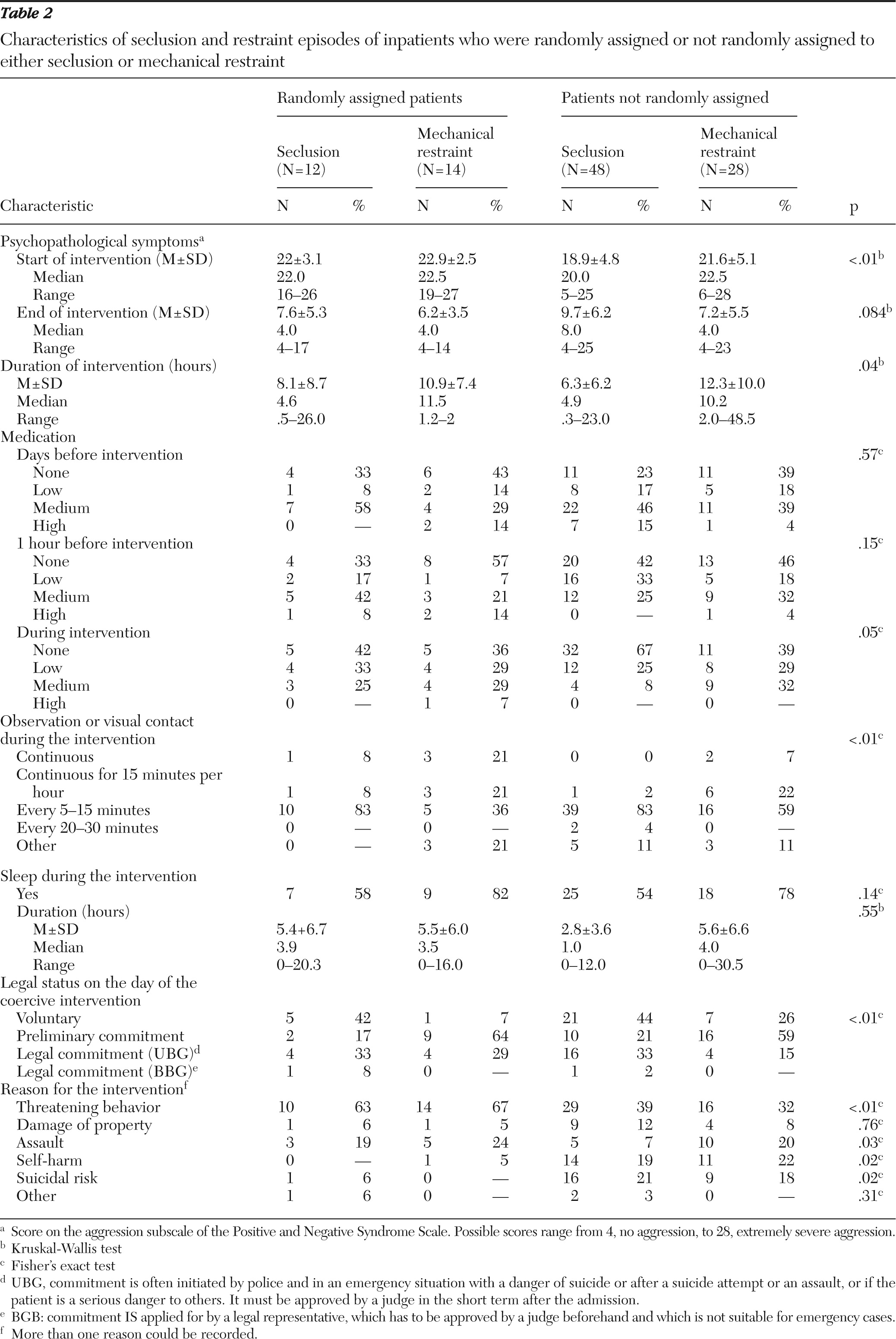
Demographic and clinical characteristics are presented in
Tables 1 and
2. No baseline differences were found between the two randomized intervention groups, indicating that randomization led to equivalent groups. The significant differences in the tables are for the nonrandomized groups.
Subjective experience of coercive measures
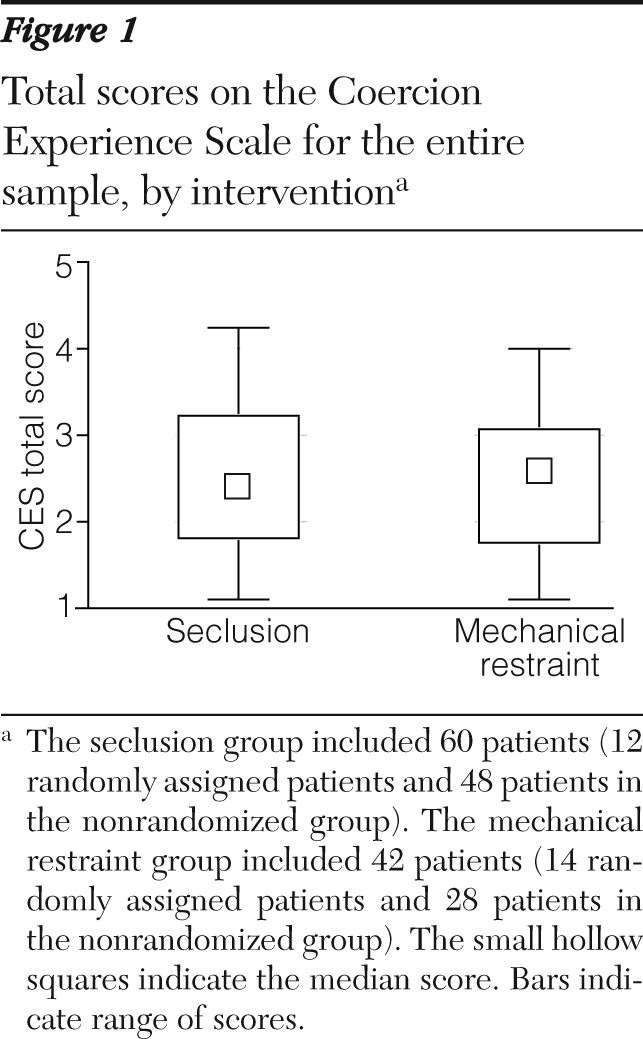
The first hypothesis was that the mean total CES scores would differ significantly between the seclusion group and the mechanical restraint group across the entire sample (when patients in the randomized and nonrandomized arms were considered together). As shown in
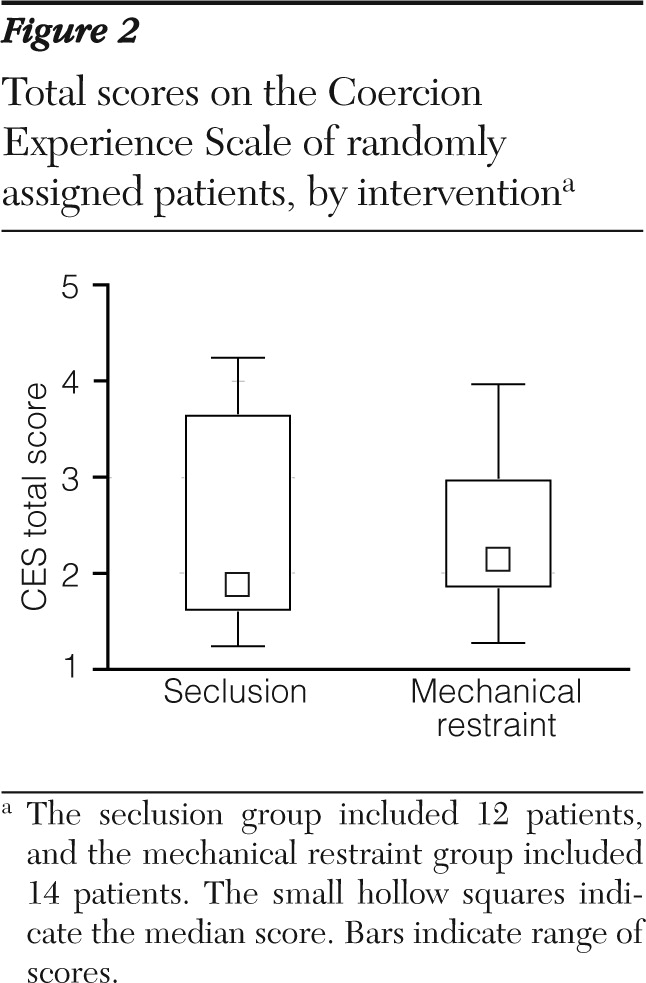
Figure 1 there was no significant difference between the two groups in the level of experienced coercion as measured by the CES. The second hypothesis focused only on the difference in mean total CES scores between the patients were randomly assigned to each intervention group. However, as shown in
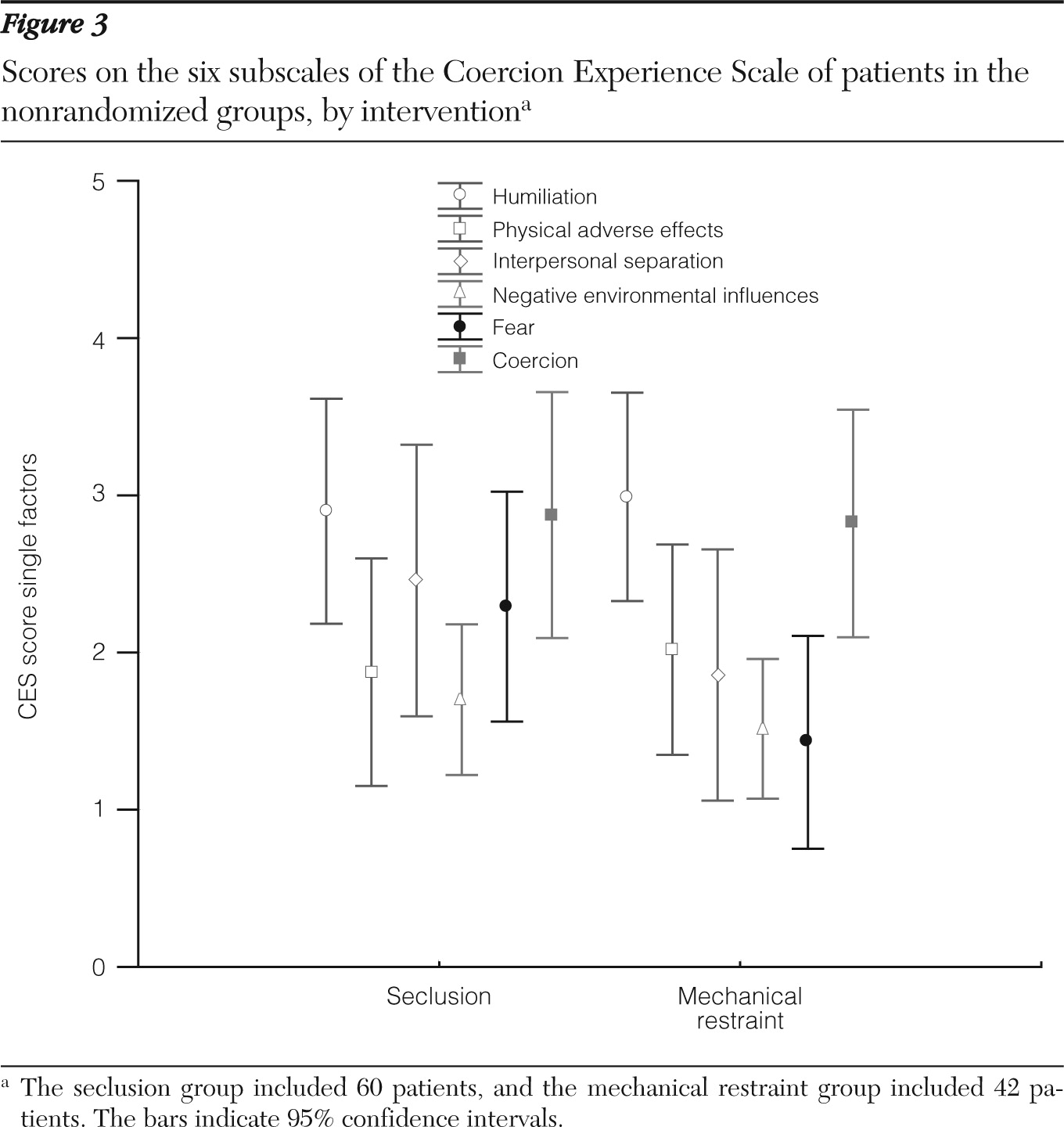
Figure 2, no significant difference was found between the randomized groups in the CES total score. Analysis of subscale scores yielded only one significant difference between the randomized groups; patients in the mechanical restraint group experienced lower levels of fear then patients in the seclusion group (mechanical restraint median score =1.00, range=1–5; seclusion median score=2.25, range=1–5, p=.049 (
Figure 3).
Global strain
Patients assessed the global strain of the intervention on a visual-analogue scale. Median scores were highly similar for all groups.
Medication
Significant differences in the total dosage of medication were found only during the intervention and only between the nonrandomized groups. Patients in the seclusion group received less medication than those in the mechanical restraint group.
Aggressive symptoms
Compared with all other groups, patients in the nonrandomized seclusion group had significantly lower aggression scores when the intervention was initially implemented.
Adverse events
During seclusion episodes, six adverse events were observed: severe agitation with damage to the seclusion room (N=1), attempted suicide (N=1), fracture (N=1), and self-harm (N=3). During mechanical restraint episodes, one adverse event was observed: retraumatization of a former torture victim. No significant differences were found between the seclusion and mechanical restraint groups in adverse events.
Discussion
To our knowledge, this study is the first randomized trial of coercive measures. The results provide evidence that the psychological impact of seclusion is comparable to that of mechanical restraint and that neither measure can be classified as less restrictive. No significant differences in patients' perceived coercion—CES total score, the primary outcome measure—were found between the seclusion and mechanical restraint groups. This result applied to the comparison of the randomized groups and the comparison of the seclusion group and the mechanical restraint group across the entire sample (that is, when patients in the randomized and nonrandomized arms were considered together). In addition, no significant differences in secondary measures were found between the randomized groups. Furthermore, patients in both intervention groups perceived the global strain of the intervention nearly identically.
No validated instruments have been available to compare different kinds of coercive interventions. Such an instrument must measure subjective experience, must be applicable to all kinds of coercive interventions, and must refer to the ethical construct of restriction of human rights. The CES, which was developed for this study, meets all three criteria (
25).
Because of the study design, the generalizability of the results can be estimated on the basis of the significant differences in primary and secondary outcome variables between the randomized and nonrandomized groups. However, there were three significant differences between the groups on other variables, which may limit generalizability. In the randomized groups, threatening behavior was the reason for implementing the intervention significantly more frequently than in the nonrandomized groups. In addition, the randomized groups included more male patients than the nonrandomized groups, and the randomized groups had no patients with personality disorders. Therefore, external validity can be described as acceptable.
This study had several strengths, which give us confidence in our findings. The design of this trial met all of the requested conditions of the Cochrane Review on coercive measures (
5). Results showed that randomization was successful and that the external validity was verifiable and acceptable. Although the issue of coercive measures is highly challenging ethically, a satisfying and justifiable compromise between service users' rights and scientific requirements was effected. Reliance on patients' assessments required sophisticated skills in interviewing. However, it was necessary to measure the outcome subjectively, and no objective assessment could be used as a substitute. The dropout rate was low, and the missing data could be minimized by interviewing patients rather than asking them to complete a questionnaire. A validated instrument was used to measure the main outcome. It can be used to compare more than one coercive intervention, it takes the subjective experience of service users into account, and it focuses on the subjective strain and the restriction of human rights. This study demonstrated a method that can be used in future research on coercive measures.
Although no significant between-group difference in the primary outcome was found, aspects of the results allow meaningful clinical conclusions. Because feelings of helplessness may indicate traumatization (
27,
28), it may be important to give some control of the situation to the service user. Therefore, the intervention that is regarded as least restrictive by the patient should be used, if it is possible to give the patient a choice.
Scores on the fear factor were significantly lower in the randomized mechanical restraint group than in the randomized seclusion group. This finding underlines the importance of taking any measures to reduce fear. Such measures may include more observation, contact, and monitoring, and higher doses of anxiolytic medication, if necessary.
During seclusion six adverse incidents occurred, whereas only one incident occurred during mechanical restraint. Although this difference was not significant, it seems worth mentioning. The difference may be due to better monitoring during restraint or to immobilization or higher doses of medication.
Several limitations of this trial should be noted. As noted, the external validity can be regarded as respectable on the basis of the differences between the randomized and nonrandomized groups for each intervention. However, the generalizability with respect to other psychiatric hospitals and other regions must be carefully analyzed. Standards for implementing coercive interventions differ widely from hospital to hospital. In hospitals that use only one intervention, patients may judge the expected measure as less restrictive (
29,
30).
Because the trial had to be stopped prematurely, data analyses were explorative and the sample size was rather small. The randomization ratio of 25% was half of the expected ratio. This may have resulted from the study design: for ethical reasons patients could choose to be randomly assigned. In the nonrandomized seclusion group, the aggression score and, correspondingly, the total dose of medication were lower and the duration of the seclusion episode was only half that of the restraint episode; this finding indicates that clinicians chose seclusion for less aggressive patients. However, although there may have been some selection bias in the nonrandomized cohort arms, the finding of no difference in outcome measures between all four groups seems rather robust.