Borderline personality disorder is a severe mental disorder associated with a high burden of disease (
1) and high economic burden (
2).
DSM-IV-TR defines borderline personality disorder (in axis II, cluster B) as a pervasive pattern of instability of interpersonal relationships, self-image, and mood, as well as marked impulsivity, beginning by early adulthood and present in a variety of contexts. Common co-occurring conditions are substance abuse and dependence, depression, and other mood and personality disorders (
3). The prevalence is approximately 2% in the general population, 15%–20% among psychiatric patients, and probably even more among patients with substance use disorders (
4).
Natural recovery is estimated at about 4% per year (
5), whereas receipt of treatment is associated with recovery that is up to seven to eight times faster (
6). The Dutch multidisciplinary practice guideline for patients with personality disorders (
7) recommends psychotherapy as a first-step treatment in all cases of borderline personality disorder. The efficacy of psychotherapeutic treatment in personality disorders is not primarily determined by the specific theoretical orientation. One of the most important determinants of the efficacy is a clear and coherent therapy framework, which should be applied consistently. Dialectical behavior therapy, schema-focused therapy, mentalization-based treatment, and transference-focused psychotherapy are examples of empirically supported psychodynamic and cognitive-behavioral psychotherapeutic treatments that are structured and manualized (
7). The use of semistructured interview schedules is recommended in the diagnostic phase.
In other countries practice guidelines with similar recommendations have been published (
8,
9). However, there is suggestive evidence that a gap exists between what is recommended in practice guidelines (optimal care) and what actually occurs in specialized mental health practice (actual care) concerning key recommendations for diagnosis and treatment (
10).
This study had two main objectives. The first was determining the gap that exists between actual care and optimal care for patients with borderline personality disorder, and the second was identifying facilitators and barriers that affect the implementation of guideline recommendations in specialized mental health organizations.
Methods
A cross-sectional study was conducted to determine the diagnostic and treatment gap prospectively by analyzing patients' medical records. Focus interviews were held to identify facilitators and barriers to implement key guideline recommendations. Thirty-eight specialized mental health organizations in the Netherlands were invited to participate in the study. The first ten organizations that responded could participate.
For the first research objective, researchers requested medical records for a sample of the 50 most recent patients at each organization whose records indicated that they had a diagnosis of borderline personality disorder. The researchers' goal was to determine the proportion of patients who immediately received a DSM-IV diagnosis of borderline personality disorder (that is, not at a later stage of treatment after having first received another diagnosis) and the proportion of patients immediately receiving this diagnosis who also received psychotherapy as a first-step treatment. Diagnosis Treatment Combination (DTC) data were used. One DTC covers a period of one year maximum, and medical records of each patient comprise one or more DTCs. DTC data were introduced in the Netherlands in 2005 and contain information on diagnosis and treatment at the level of the individual patient. Mental health organizations are required by the government to use DTC registration to determine and invoice the total costs of treatments.
Patients were included in the sample if they had a primary diagnosis of borderline personality disorder and were at least 18 years of age. DTC data for the patient in previous years were provided (DTC history), including patient functioning as measured by the Global Assessment of Functioning (GAF) (
3). GAF scores range from 0 to 100, with higher scores indicating better functioning. Data files were not aggregated but analyzed on an organization level by using SPSS, version 15.0.
For the second objective, two series of focus group interviews were conducted in 2010. We aimed to recruit at least two professionals (psychiatrists, psychologists, and nurses) and two managers from each participating mental health organization. The first series of focus interviews took place with participants from all ten organizations, with managers and professionals participating in separate groups. Interchange between representatives of the organizations was encouraged in the groups. Barriers and facilitators in regard to implementation of key recommendations of the practice guideline were explored from a number of perspectives: the guideline itself, the professional, the patient, the medical-scientific boards, the mental health organization, and the macro system (laws, regulations, and financing) (
11). Identified factors were ranked by importance and by the extent to which they could be modified.
In a second series of focus group interviews, each organization was visited separately, and professionals and managers participated in a single focus group. Feedback on the gap findings was presented, and participants were asked to elaborate on findings of the first focus interview. All focus interviews were audio-recorded, and a summary of findings was made (
12).
Results
Ten specialized mental health organizations from rural and urban areas participated in this study. Together they covered a catchment area of approximately 5,900,000 inhabitants (one-third of the population of the Netherlands).
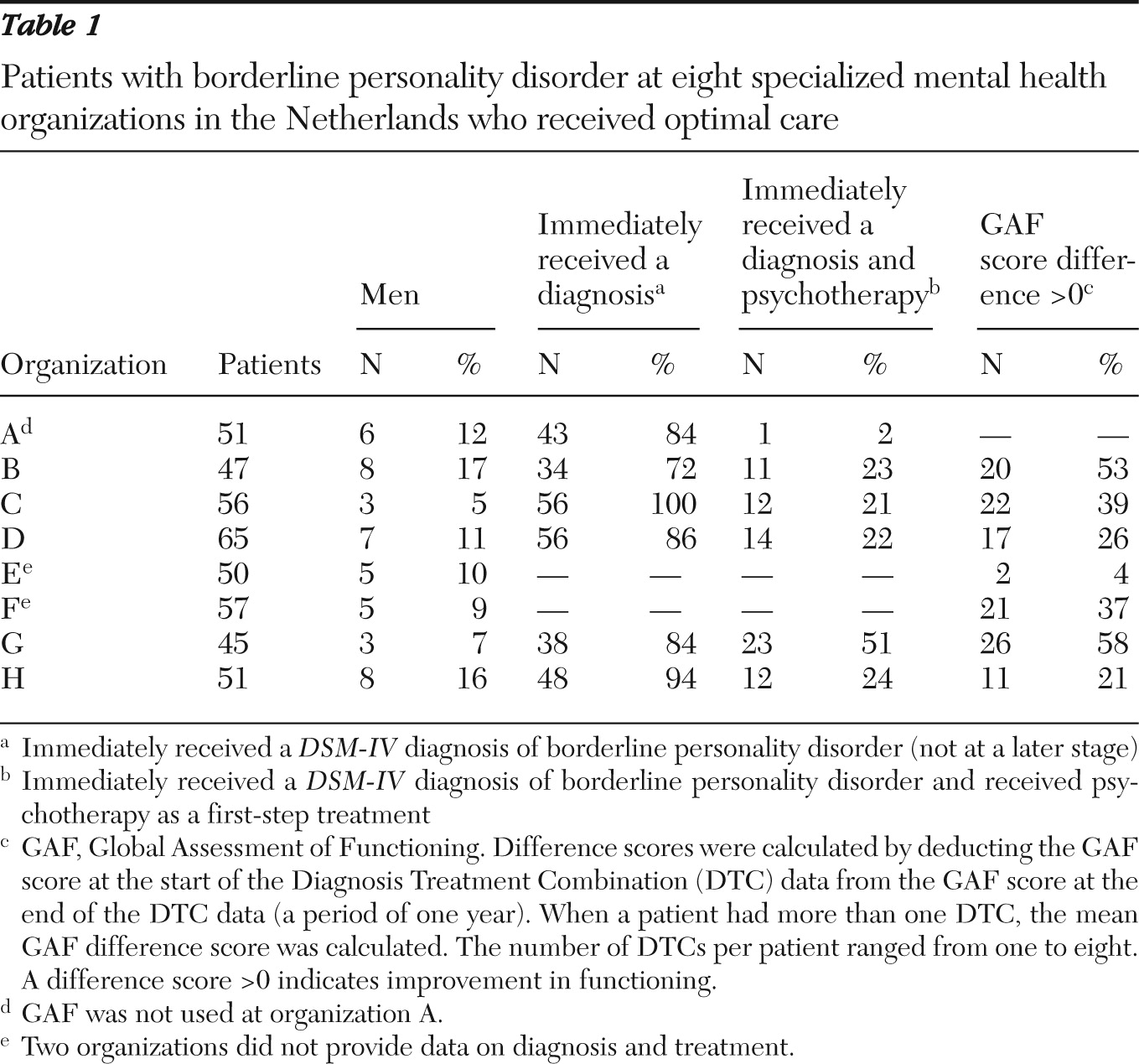
To address the gap between optimal and actual care, eight organizations (80%) provided data for 422 patients with borderline personality disorder; two organizations were unable to provide the requested data file. Results are presented in
Table 1. Most patients were female (range 83%–94%). Six DTC data files (60%) were adequate to provide an answer to our questions on diagnosis and treatment (N=315 patients). Between 72% and 100% of the patients with borderline personality disorder at each organization received the diagnosis as their first diagnosis (median 85%). Between 2% and 51% of the patients with an initial diagnosis of borderline personality disorder received psychotherapy as a first-step treatment (median 23%). The GAF difference scores show that a minority of patients showed progress in functioning—4%–58% of patients (median 37%) had a GAF difference score greater than 0.
Twenty-four professionals and 11 managers from the ten organizations were actively involved in the focus interviews. The following barriers, in order of importance, were identified. First, applying recommendations from the practice guideline was hampered mostly by insufficient capacity of trained psychotherapists. As a result, only a few patients could be offered psychotherapy. Moreover, patients received psychotherapy at a lower intensity than was recommended by the guideline. The gap occurred mostly in outpatient care. The source for this structural barrier is within the macro system—that is, it is the result of limited health care financing. Second, organizational barriers caused inefficiency. Many organizations had difficulties in systematically implementing the guideline recommendations. Third, barriers at the level of the patient and psychotherapist contributed to inefficiency in the provision of care. Patients receiving psychotherapy failed to keep many of their appointments. In addition, both patients and professionals were hesitant to end psychotherapy, which meant that patients stayed in psychotherapy too long. Fourth, on a professional level, semistructured interview schedules were not used systematically. Fifth, the guideline does not give recommendations for cases in which patients must be stabilized and motivated before entering psychotherapy treatment. As a consequence, most organizations did not provide guidance for treating these patients.
Discussion
Our assumption that patients with borderline personality disorder have a long history of axis I diagnoses before receiving the correct diagnosis was not confirmed by our data. This cross-sectional study showed that most patients with borderline personality disorder were given that diagnosis immediately after entering specialized mental health care (median 85%). However, only a minority received psychotherapy as a first-step treatment (median 23%). Insufficient capacity of trained psychotherapists, primarily an insufficient number of psychotherapists, was the main explanation for this gap. Of the patients who did receive psychotherapy, some received suboptimal treatment (for example, psychotherapy at a lower frequency, such as once every two weeks instead of every week). The 23% of patients who received optimal treatment should therefore be interpreted as a maximum. Many patients who did not receive any form of psychotherapy were provided with an adapted psychotherapeutic treatment from a social psychiatric nurse, according to the professionals in the focus groups. Psychiatric nurses are not psychotherapists, and therefore the treatment was not registered as a psychotherapeutic intervention.
The study had some limitations. First, DTC data do not contain all the data for our quantitative research question. For example, the unrecognized patients, that is, patients with borderline personality disorder who had not yet been given a diagnosis of borderline personality disorder were not included in the files. The proportion of patients who were immediately diagnosed should therefore also be interpreted as a maximum. Second, the reliability of the DTC registration system for use in scientific research and policy making in general can be questioned (
13). In part this may be due to start-up problems (DTC registration is still relatively new and data may not always be complete), but it is also related to the purpose of the DTC registration (mental health organizations require DTC registration to invoice the treatment costs of patients). Third and finally, relevant information was lacking in this study. The type of psychotherapy (theoretical framework) was not explored, nor did we have information on fidelity.
Conclusions
Although effective psychotherapy treatments exist, our gap study showed that less than a quarter of patients with borderline personality disorder received this first-step treatment. Implementation of the guideline was hampered mainly by capacity problems and organizational factors. Capacity problems are difficult to address, but organizational factors can be addressed. To improve efficiency, the development of care pathways should be considered. Care pathways improve quality of care and efficiency.
Acknowledgments and disclosures
The study was funded by grant 80-82315-97-10003 from the Netherlands Organization for Health Research and Development (ZonMW).
The authors report no competing interests.