Smoking-related illnesses are the most common type of preventable diseases in the United States today (
1). Although the public health focus on smoking cessation has resulted in a reduction of the prevalence of cigarette smoking to about 20% in the United States (
2), 50% to 85% of people with severe mental illnesses, such as schizophrenia and severe mood disorders, still smoke (
3,
4). Research has also shown that individuals with severe mental illness die at a younger age—up to 25 years younger—than persons in the general population (
5), mostly from cardiovascular diseases that are caused or worsened by smoking. As in the general population, people with severe mental illness who smoke die younger than those who do not (
6).
People with severe mental illness both with and without substance use disorders want to and frequently attempt to quit smoking (
11,
12). Evidence-based treatments, such as a combination of group or individual treatment plus medication (nicotine replacement therapy or bupropion or both), help these people succeed in quitting (
13). Research shows that people with schizophrenia are twice as likely to quit smoking when they receive psychosocial treatment with medication, such as bupropion (
14). Among people with substance use disorders, the findings are similar but limited to nicotine replacement therapy (
15).
The Institute of Medicine highlighted the fact that smoking occurs disproportionately among people with mental illness and recommended that they be included in smoking research (
16). However, relatively little research has evaluated characteristics of smokers with severe mental illness who have quit or attempted to quit smoking. One study reported that persons with severe mental illness who identify as African American or Latino and those with more education were more likely to try to quit (
17). Another study found that smokers with severe mental illness, like former smokers in the general population (
18), reported that the main reason for trying to quit in the past was a concern about their health (
19). A retrospective study of veterans who participated in a multicomponent smoking cessation program for people with mental illness with or without a substance use disorder reported that participants were less likely to quit if they had a diagnosis of schizophrenia or an alcohol use disorder than if they had a diagnosis of another mental or substance use disorder (
20).
Predictors of cessation among clients with schizophrenia are older age at smoking initiation and an increased attention span (
21), along with the use of bupropion as a cessation aid (
22). On the opposite side of the coin, correlates of smoking severity among clients with schizophrenia were increased depressive symptoms, increased illness severity, and decreased global assessment of functioning and quality of life (
23). Also, the same study did not find significant differences in prevalence of smoking between diagnostic groups.
This study examined data from an 11-year, prospective, observational study of people with co-occurring severe mental illness and substance use disorders to assess rates and predictors of smoking cessation over time. We hypothesized that the following characteristics would be associated with quit attempts or smoking cessation: more years of education, higher income, fewer psychiatric symptoms, a psychiatric diagnosis other than schizophrenia or schizoaffective disorder, chronic health problems, abstinence from alcohol or drugs, fewer cigarettes smoked, contact with friends who are abstinent from alcohol and drugs, and involvement in more social activities.
Methods
The New Hampshire Dual Diagnosis Study was a prospective longitudinal study of clients with severe mental illness and co-occurring substance use disorders (alcohol or other drugs) (
24). Trained interviewers assessed clients at baseline and yearly for 16 years. Informed consent was obtained before study involvement and each year over the course of the study. Questions regarding smoking were added to the interviews in the fifth year and continued through the end of the study.
Participants
Researchers recruited 223 participants through clinician referral from seven New Hampshire community mental health centers between 1989 and 1992. Recruitment inclusion criteria included an axis I diagnosis of schizophrenia, schizoaffective disorder, or bipolar disorder; active alcohol or drug abuse or dependence in the past six months; 18 to 60 years old; absence of general medical conditions; and willingness to participate in case management.
From year 5 to year 16 researchers interviewed between 174 and 117 participants regarding smoking (the numbers decreased because of attrition). Researchers included all interviewed participants at each time point in order to use full information in the analyses. Year 5 is considered the baseline for the smoking analyses reported here. The study was approved and monitored by the Dartmouth Committee for the Protection of Human Subjects. More information about the parent study design, recruitment, screening, and main outcomes has been reported elsewhere (
24,
25).
Measures
Baseline demographic characteristics and diagnosis.
At baseline, interviews with the Uniform Client Data Inventory (
26) assessed demographic characteristics, which included age, gender, marital status (ever married and never married), and level of education (high school or more and less than high school). The Structured Clinical Interview (SCID) for DSM-III-R (
27) assessed psychiatric and substance use diagnoses. In these analyses, researchers dichotomized the diagnosis of severe mental illness into either schizophrenia spectrum disorders (including schizoaffective disorder) or bipolar disorder.
Smoking variables.
Interviews assessed current smoking status (current smoker, quit, or never smoked), length of smoking and quit time, number of cigarettes smoked, and money spent on cigarettes in an average week. We assessed three smoking variables regarding quit attempts as outcomes: any quit attempt, number of quit attempts in the past year, and duration of smoking abstinence in the past year. Interviews assessed medications prescribed for smoking cessation by participant self-report of nicotine replacement therapy or bupropion.
Other yearly measures.
Interviews assessed current symptom severity with the expanded Brief Psychiatric Rating Scale (BPRS) (
28); we excluded the subscale of disorganization from these analyses because of the limited distribution. Possible BPRS total scores range from 24 to 73, with higher scores indicating more psychiatric symptoms. The possible ranges for the BPRS subscales of anergia, thought disturbance, activation, and affect are from 1 to 7, with a 1 indicating no symptoms and a 7 indicating severe symptoms. We measured proportion of days of independent living by participant self-report supplemented by hospital and outpatient records (
29).
Interviews measured chronic medical problems that interfered with life by self-report of various illnesses. Researchers used consensus ratings on the Alcohol Use Scale (AUS) and Drug Use Scale (DUS) to measure the severity of drug and alcohol use on the basis of information from a structured timeline follow-back interview (
30), clinician ratings, and urine drug screens (
31). The AUS and DUS are 5-point scales that are based on
DSM-IV-R criteria for severity of disorder: 1, abstinence; 2, use without impairment; 3, abuse; 4, dependence; and 5, severe dependence. Interviews assessed caffeine use by participant report of daily consumption of caffeinated beverages, and this variable was transformed by square root to adjust for skewness.
Researchers assessed activities in daily life with questions from the Quality of Life Interview (QOLI) (
32) related to engaging in playing cards, sports, or a hobby or reading a book, magazine, or newspaper. We used a subscale of the QOLI to measure social relationships. Interviews measured social contact with non-substance-abusing friends with two questions, “Do you have any close friends who do not use alcohol or other drugs at all?” and “About how often do you do things with any of the friends who do not use alcohol or other drugs?”
Interviews assessed employment over the past year by asking for the number of hours participants worked in a competitive job. Because of the high proportion of zeros, data analysts recoded this variable as either any work or no work over the past year.
Statistical analysis
Descriptive statistics, chi square tests, and analyses of variance were used to examine demographic differences between the three groups (current smokers, former smokers, and never smoked) at baseline. In addition, descriptive statistics assessed characteristics of interest at each year. We then conducted a systematic multivariate analysis to explain whether quitting smoking over time was related to variables in four domains (demographic, clinical, financial, and social) for the three smoking cessation outcomes described above: any quit attempt, number of past-year attempts, and duration of past-year smoking abstinence. We selected potential predictors for quit outcomes based on previous research on smoking cessation in the general population and among people with severe mental illness and substance use disorders (
17,
19,
33–
35).
Preliminary analyses explored relationships between multiple predictors and these outcomes. We fit a series of models that included all relevant time-constant covariates and time-varying covariates for each model. We examined concurrent and lagged associations between each covariate and outcome. Because we did not find any differences between the concurrent models and the lagged models, we report only the concurrent models here. Model fit determined the selection of the random component for each outcome: we chose either a random-intercept model or a random-intercept-slope model, depending on model fit.
In the final models, we used generalized linear mixed-effects models in SAS GLIMMIX (
36). We chose an integral approximation method (-LAPLACE) for parameter estimation in order to provide real maximum-likelihood estimation rather than pseudo-likelihood estimation.
Results
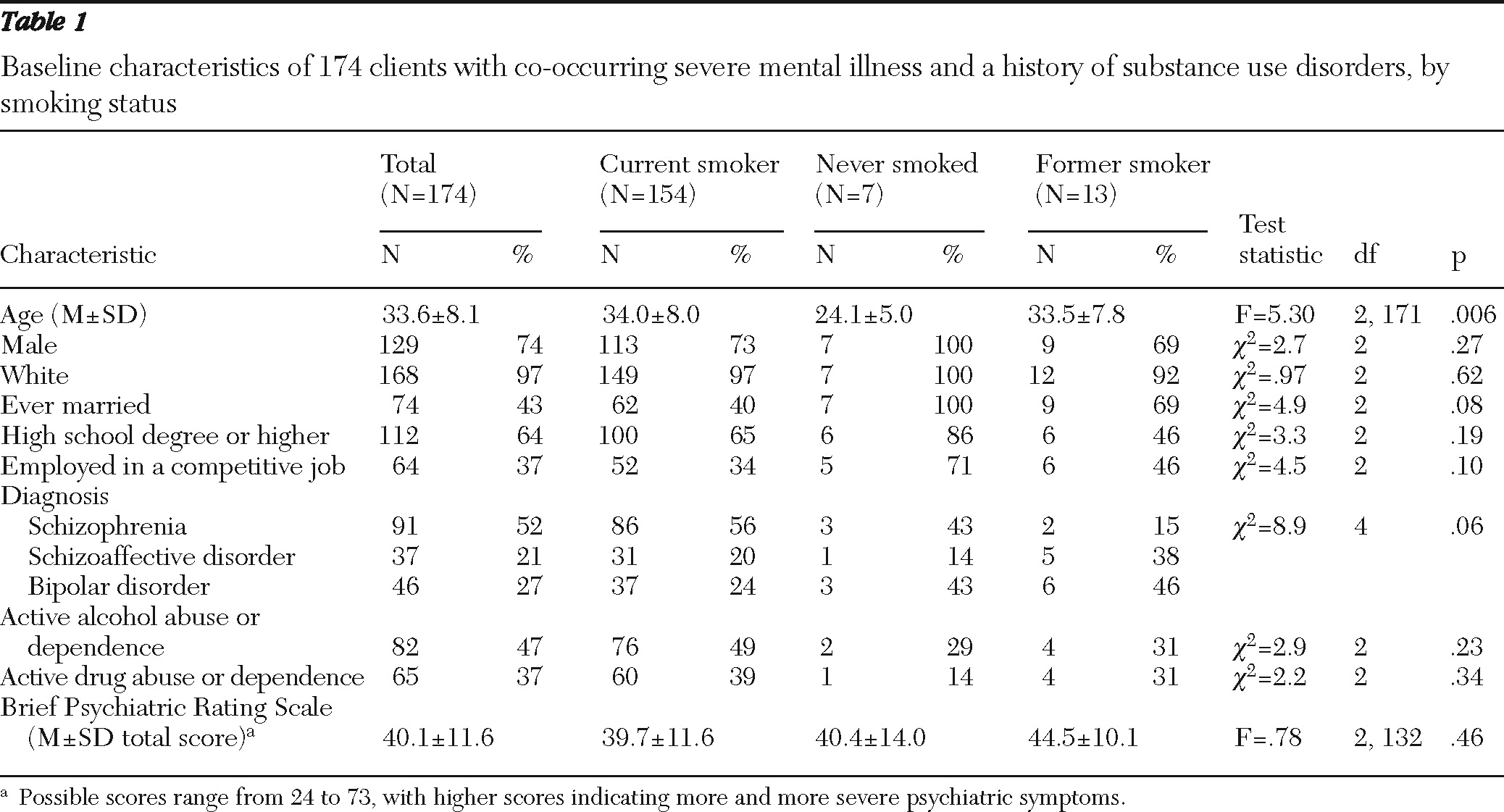
At baseline, the first year of smoking data collection, 174 participants were engaged in the study: 74% were male, 97% were white, 64% had at least a high school degree or GED, and the mean age was 34 years (
Table 1).
A total of 128 participants (73%) had schizophrenia or schizoaffective disorder, and 46 (27%) had bipolar disorder. The entire sample had a history of a drug or alcohol use disorder, but 76 (49%) had an active alcohol use disorder, and 60 (39%) had an active drug use disorder. On average, participants reported none to very mild symptoms on the BPRS subscales measuring anergia (1.5±.7), thought disturbance (1.9±1.3), and activation (1.3±.65). Scores on the affect subscale were slightly higher, from very mild to mild (2.3±1.1).
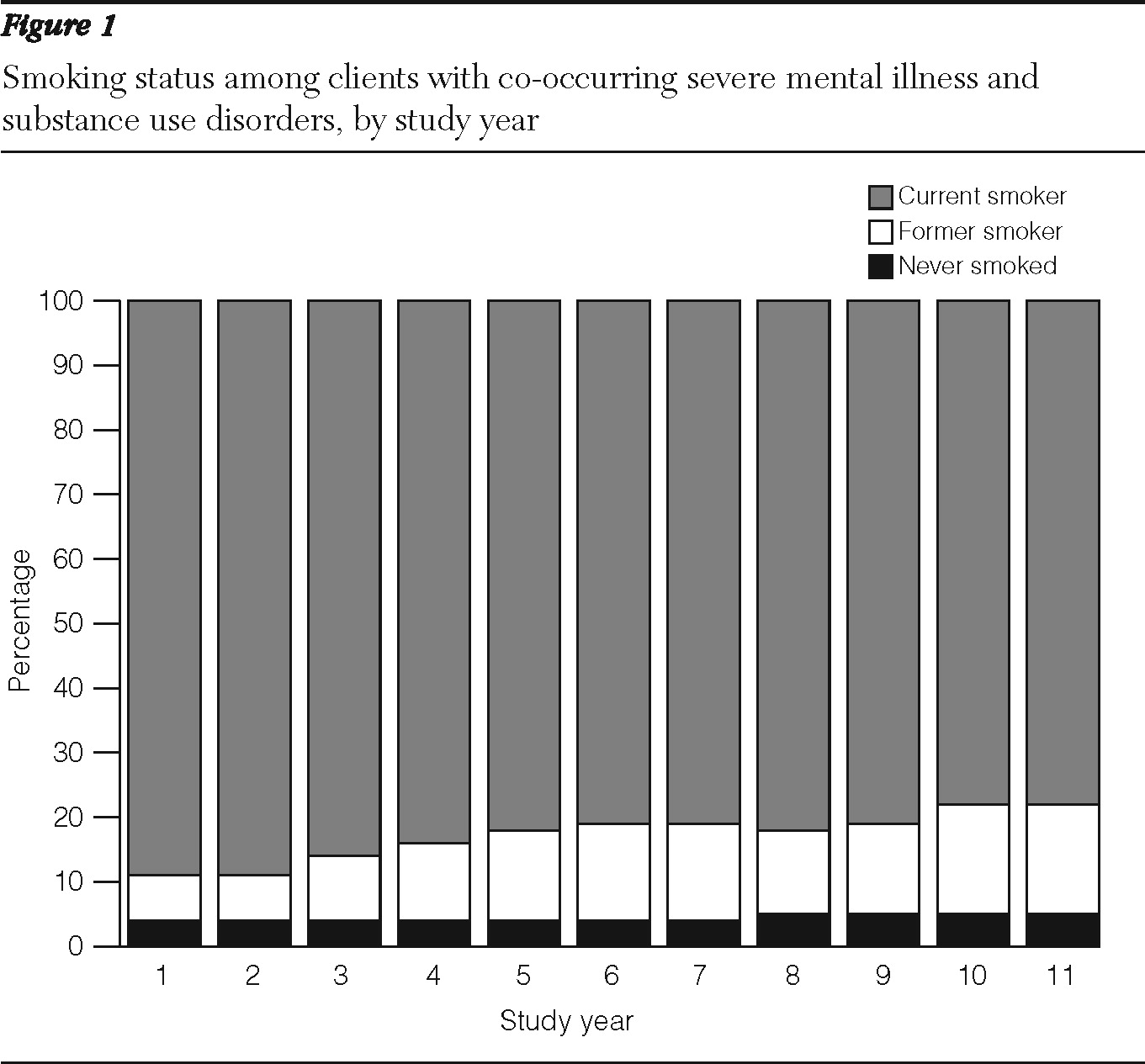
At baseline of the smoking data collection, 154 of the 174 (89%) participants were current smokers, seven (4%) had never smoked, and 13 (7%) were former smokers (
Figure 1). The current smokers averaged about 1.5 packs per day (mean±SD=31.6±14.9 cigarettes) and had smoked for more than 20 years (21.8±9.1 years). Former smokers averaged about 14 years of smoking (13.9±9.4 years) and had quit smoking about six years before the study interview (5.7±9.6 years).
As shown in
Table 1, smoking subgroups differed by age. Specifically, clients who had never smoked were younger than current smokers and those who had quit smoking.
As shown in
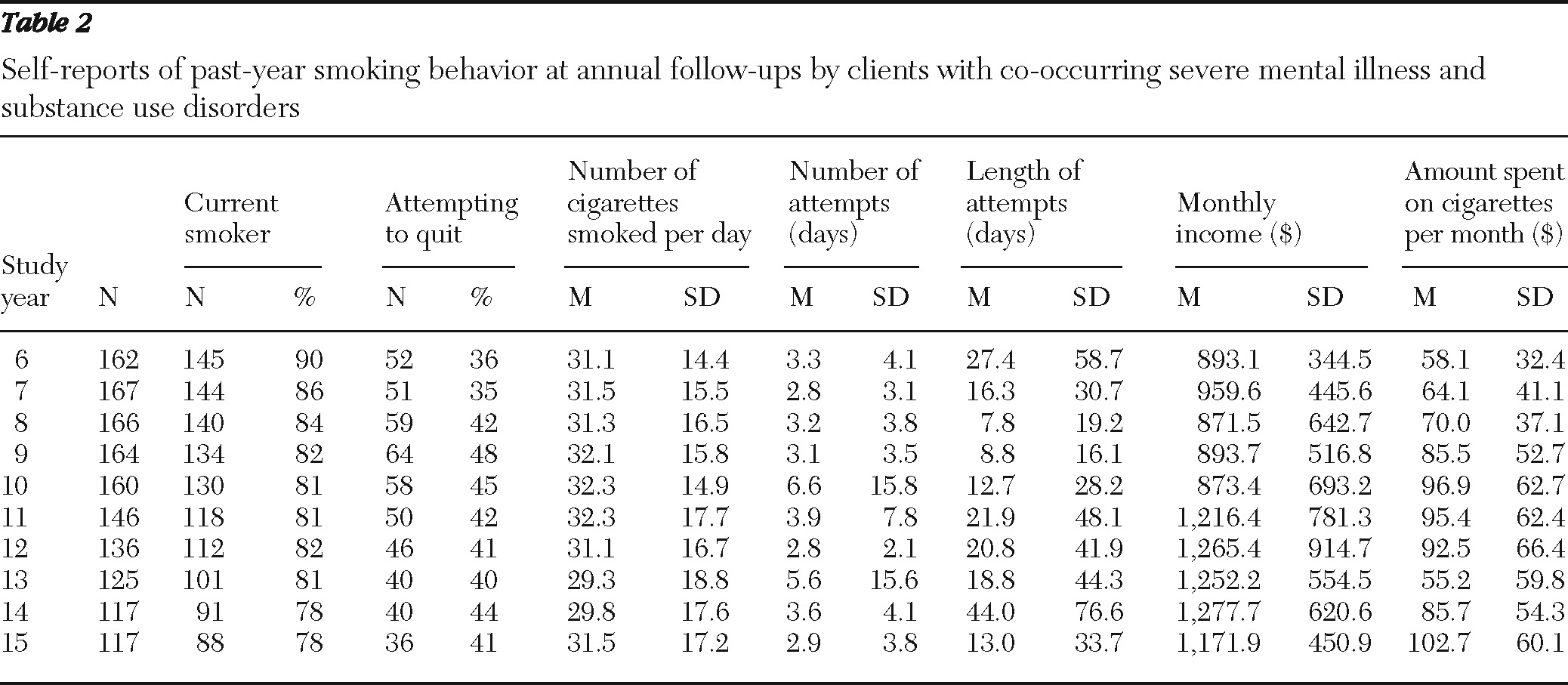
Table 2, follow-up participation rates varied from year to year but decreased over time. The proportion of participants who smoked at each time point decreased steadily but remained high. By the final follow-up interview (year 15 of the larger study), 78% continued to smoke. The average number of cigarettes smoked per day among current smokers at each time point stayed relatively stable over the 11 years of the follow-up, with a range from 29.3 to 32.3 cigarettes. The average proportion of monthly income smokers spent on cigarettes ranged from 7% to 10%.
Each year over one-third of the group reported at least one quit attempt (
Table 2). During the 11-year study period, 75% of the participants who smoked at baseline (115 of 154) attempted to quit at least once. Of those who attempted to quit, 40 (35%) attempted one to five times, 48 (42%) attempted six to 17 times, and 27 (23%) attempted 18 to 80 times. None of the participants, however, reported using nicotine replacement therapy or bupropion.
The average duration of abstinence attained after a quit attempt varied between one and six weeks. During the 11 years of the study, the proportion of former smokers at each assessment doubled from 7% to 17% (
Figure 1). Most of the participants who quit relapsed: 44 participants reported abstinence from smoking at least once at the yearly interviews, but no more than 20 participants were former smokers at any given assessment.
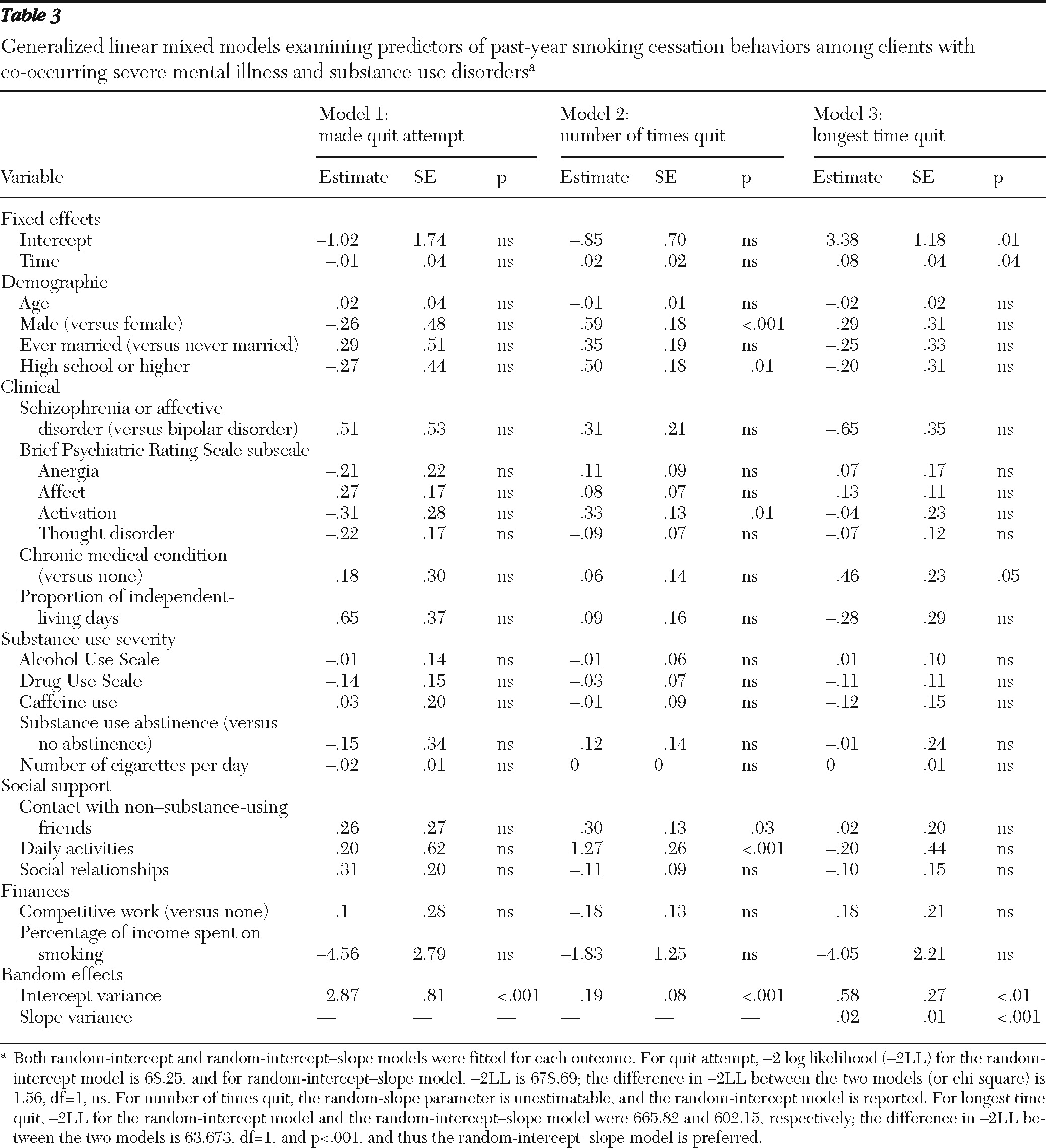
Table 3 shows the results of three generalized linear mixed-effects models. The first model found no covariates associated with the likelihood of a quit attempt in a given year. The second model found that two demographic variables, being male and having a high school education or higher, were associated with more attempts to quit smoking. In the second model three time-varying covariates were also associated with more attempts to quit: higher BPRS-activation scores, more social contact with non-substance-using friends, and more daily activities. In the third model, having a chronic general medical condition predicted longer periods of smoking abstinence.
Discussion
Most participants in this study tried to quit but continued to smoke throughout the 11-year follow-up period. At baseline, the few nonsmokers were younger than the smokers and former smokers. Many of the smokers engaged in numerous quit attempts, but few were able to sustain abstinence and none of the participants reported using either nicotine replacement therapy or bupropion to aid in quitting. Having a chronic general medical condition predicted longer periods of abstinence.
Our data indicate that clients with co-occurring serious mental illness and substance use disorders often attempted to quit smoking without professional treatments and with limited success. Studies indicate that a combination of smoking cessation groups and medications (bupropion, nicotine replacement, or varenicline) increases the likelihood of achieving abstinence among clients with severe mental illness (
37,
38). Yet none of the clients reported using nicotine replacement therapies or bupropion, and smoking cessation support groups were unfunded and unavailable in New Hampshire mental health centers throughout the course of the study.
One study showed that psychiatrists can help clients to quit smoking by asking, advising, assessing, assisting, and arranging treatments (
39). But psychiatrists are less likely to use these “5As” if they themselves are current smokers, feel uncomfortable discussing smoking cessation, or report competing priorities (
40). Treatment providers are also less likely to offer cessation treatment to people with severe mental illness and substance use disorders if they are concerned about substance abuse relapse (
41), even though studies show that concomitant substance abuse treatment and smoking cessation treatment does not increase the risk of relapse but strengthens sobriety efforts (
13). Also, symptoms of mental illness are not worsened by smoking cessation (
42–
44), and recent pharmacotherapy guidelines for persons with schizophrenia prescribe the use of bupropion plus a class or group for smoking cessation (
45).
Few of our hypotheses were confirmed. Abstinence from alcohol and drugs, fewer cigarettes smoked, and fewer overall symptoms did not predict quitting activity or duration of abstinence. For these variables, severe mental illness may moderate the effects on cessation found in the general population.
Several of our findings parallel trends in the general population. Lower rates of smoking among younger clients suggest that they may be initiating smoking at lower rates than in the past. Our clients' yearly rates of quit attempts were similar to the rate of 43.4% found among smokers in the general population (
46). The smoking cessation success rates of our study are similar to rates in the general population when individuals with a high level of dependence attempt to quit without assistance (
47). Smoking rates in New Hampshire declined by about 4% (from 23.3% to 19.4%) between 1998 and 2007 (
48), and smoking in our study group declined by almost 9% over a similar period (from 86.4% to 77.9% between 1996 and 2006).
As in the general population (
49), peer social support, particularly from friends who did not use alcohol or drugs, was related to quit attempts. We did not measure whether these friends were also abstinent from smoking. In the 30-year Framingham Heart Study, the prevalence of smoking decreased over time, but the size of clusters of smokers remained the same (
50), suggesting that groups of people quit in concert. In that study, smoking cessation by a friend decreased the chances of smoking by 34%. Other research in the general population has also demonstrated that the absence of smokers in the home (
46) and home smoking bans (
51) were strongly associated with successful cessation. These findings suggest using peer support and facilitation of pleasant replacement activities in cessation interventions for people with co-occurring severe mental illness and substance use disorders.
Clients with these dual issues had longer periods of abstinence if they also had a chronic general medical condition. A longitudinal study in the general population similarly found that the worsening of physical symptoms predicted smoking cessation (
52). Other research shows that smokers with chronic illnesses, such as heart disease, arthritis, or diabetes, were more likely to want to quit smoking (53) and were more successful at quitting than smokers without these health issues (54). The primary difference between our findings and studies in the general population is that abstinence was not maintained among people with co-occurring severe mental illness and substance use disorders.
Public health and policy efforts to reduce smoking, such as increased taxation, smoking bans in mental health centers, and free telephone quit support lines, have not yet been studied extensively among people with co-occurring severe mental illness and substance use disorders. Meanwhile, other public policies, including the lack of public insurance (Medicaid) reimbursement for behavioral smoking cessation treatments, may be hindering efforts to reduce smoking within this population.
Several limitations of this study warrant mention. The study group was small and included only clients with co-occurring severe mental illness and substance use disorders in New Hampshire who enrolled in a randomized controlled trial of case management. Thus results may not generalize to other groups. A significant proportion of participants were lost to attrition over 16 years. We did not directly assess smoking cessation methods, such as telephone quit lines, support groups outside of mental health centers, and whether participants used any of the available quit-smoking medications (although we asked participants what medications they were currently taking). Nevertheless, our study provides 11 years of prospectively collected data, and these findings represent the only available longitudinal data on smoking and quit attempts among clients with co-occurring severe mental illnesses and substance use disorders.