Rates of cigarette smoking are high among people with schizophrenia (45.3%–88.0%) (
1–
6), bipolar disorder (58.1%–90.0%) (
4–
8), and major depressive disorder (36.6%–73.0%) (
4–
8) compared with the rate of smoking in the general population (about 20%) (
9) or among those with no history of mental illness (about 12%) (
8). Although rates of smoking have decreased over the past 20 years in the general population (
10,
11), they have remained high among people with severe mental illnesses (schizophrenia and severe mood disorders). These individuals are more likely to start smoking and less likely to quit than those without mental illness (
1,
5,
7,
12).
Smoking tobacco (even in small amounts) contributes to the development of multiple diseases, including heart and lung diseases, stomach and pancreatic cancers, strokes, and diabetes (
13,
14). Smoking is therefore considered the leading preventable cause of death in the United States (
11). Given the high rates of smoking, higher rates of these diseases are expected and have been found among people with severe mental illnesses (
15). Recent reports have also shown a 25-year gap in the life expectancy of this group compared with the general population (
16–
19), which is largely attributable to cardiovascular disease.
Quitting smoking reduces the risk of death from tobacco-related disease: even a 60-year-old lifelong smoker gains three years of life expectancy by quitting, and those who quit before age 35 have the same life expectancy as nonsmokers (
14). Quit attempts are common among people with severe mental illnesses (
20,
21) but are typically unsuccessful if not accompanied by cessation treatment (
4).
People with severe mental illnesses tolerate and respond well to smoking cessation medications approved by the U.S. Food and Drug Administration (
22–
27). As in the general population (
28–
30), in the population with severe mental illness the strongest effects were achieved with a combination of medications and behavioral counseling. Combined treatment led to abstinence for approximately half of the study participants in the general population and for somewhat lower percentages among persons with severe mental illnesses. For example, 36% of patients with schizophrenia had continuous abstinence after 12 weeks of treatment with nicotine replacement, bupropion, and group cognitive-behavioral therapy (
25), and 43% had two weeks of continuous abstinence after 12 weeks of varenicline treatment with group cognitive-behavioral therapy (
27). On the basis of this research, combined medication and behavioral smoking cessation interventions have been recommended for people with severe mental illnesses stabilized on psychotropic medication (
31–
33). However, people with severe mental illnesses frequently do not use evidenced-based cessation treatments because of lack of interest (
34,
35) or lack of access (
36).
How can clinicians engage patients in evidence-based smoking cessation treatment? Motivational interviewing (
37,
38) and education (
38) have been shown to increase motivation to seek treatment for smoking cessation among people with severe mental illness. However, training and using clinicians to conduct such interventions involves time and money. The field needs cost-effective, easily implemented methods to motivate this population to participate in evidence-based smoking cessation treatments.
Decision support systems have the potential to meet this need (
39). They can educate, motivate, and engage users into treatment by providing simple scientific information about a medical problem (such as quitting smoking), information about treatment options, an individually tailored presentation of the risks and benefits of treatments, and personal testimonies that describe what the treatment is like and that inspire hope and motivation. Moreover, decision support systems often include exercises that allow participants to explore the advantages and disadvantages of making a decision, such as quitting smoking, and to use other motivational exercises that increase intention to change. Numerous controlled trials support their efficacy (
40). One large study, conducted in the general population of the Netherlands, demonstrated that the use of a decision support system for smoking cessation enhanced knowledge about cessation methods, improved attitudes toward use of cessation tools, and increased confidence about quitting, and it was associated with more quit attempts and abstinence at a six-month follow-up (
41).
Electronic decision support systems delivered via the Internet on home, clinic, or library computers could provide an inexpensive, systematic method to educate and motivate smokers with severe mental illnesses. This group is interested in using computers to get health information (
42), but decision support systems currently available on the Internet may be too visually complex and mechanically challenging for them (
43) because of cognitive limitations (
44) or minimal computer experience (
42). Our research group recently developed a simple electronic decision support system for smoking cessation designed for use by smokers with severe mental illnesses (
45). The purpose of this study was to test the effectiveness of the first version of this motivational tool.
Methods
Overview
This study used a quasi-experimental design to test an electronic decision support system for smoking cessation. In 2009, a convenience sample of 41 smokers with severe mental illnesses was assessed at baseline and two months later for smoking characteristics and behavioral indicators of motivation for smoking cessation. At baseline, all participants received a pamphlet on smoking cessation and a referral to a smoking cessation counselor, who helped participants consider treatment options. The intervention group used the electronic decision support system shortly after the baseline interview, whereas the control group was able to use the system after the follow-up interview. The study was approved by the Dartmouth Committee for the Protection of Human Subjects, and participants gave written informed consent.
Participants
Through flyers and posters and via clinicians' communication with their patients, we recruited English-speaking adult smokers with severe mental illnesses who were receiving supported housing and comprehensive psychiatric services at two settings within a large, urban, psychosocial rehabilitation center. Potential participants were told that the purposes of the study were to learn about smoking among people who have a mental illness and to try out a computer program about smoking. They were also told that they did not have to change their smoking habits in order to be in the study. Of 48 individuals who initially expressed interest, 43 (90%) agreed to participate. Reasons for not participating included inability to read at a fifth-grade level (N=2, 4%), severe psychiatric symptoms (N=1, 2%), and lack of interest or unstated reason (N=4, 8%). The final study group therefore included 41 participants.
Intervention
The electronic decision support system is a simple, interactive, Web-based program that is tailored for use by people with cognitive deficits and little computer experience. Following national guidelines for usability (
46), we incorporated the following features into the program. An optional tutorial on how to use a computer mouse is available at the beginning for those who have not used a computer. The program provides a small amount of information on each page. The large-font text is written at a fifth-grade reading level and formatted simply on a blank background. Users move from page to page by clicking on large, clearly labeled buttons. Information is presented in a linear sequence of pages with a maximum of one additional layer of information that can be accessed under some pages. The linear design of this version required all users to move through the bulk of information and exercises in the motivational sections, whereas in the treatment section users can choose whether to view detailed treatment information after viewing basic information about treatment. All users in the intervention group chose to view treatment information.
The program was designed to stimulate motivation to quit smoking with use of evidence-based treatment. Health behavior change theory informed the content development (
47–
50). By changing knowledge and attitudes, the program attempted to increase the user's motivation to quit smoking and to use cessation treatment to do so. Specifically, the program focused on the perceived risks of smoking and the perceived benefits of cessation treatment. A video-recorded narrator, who identifies himself as a former smoker with mental illness, guides users through the program and encourages them to quit smoking. He speaks to users at the beginning of the program and in between each section to introduce users to the purpose and tasks of each section.
Initially, the program assesses a user's smoking by asking how much the user smokes and how much he or she spends on tobacco. The user blows into a carbon monoxide meter, which provides a measure of the severity of nicotine dependence. The program then provides the user feedback on these assessments. The program also gives information about the health risks of smoking by presenting an illustration of a body upon which users can click to get more information. Users answer questions about their personal views of the pros and cons of smoking and create a summary in the form of a decision balance. These types of interactive exercises were designed to personalize the impact of smoking, improve attitudes about quitting, and increase self-efficacy for seeking smoking cessation treatment.
A two-minute video presents a vignette of one patient's attempt to quit by using a nicotine patch. The vignette is designed to develop social norms for smoking cessation treatment and increase self-efficacy for quitting with cessation treatments. The program provides information about evidence-based smoking cessation treatments that can be viewed if the user clicks on a “view” button. The cessation treatment information was designed to prepare users for a discussion with a clinician about choosing a treatment. At the end of the program, users can print out a personal report that summarizes their level of smoking, pros and cons of smoking, and treatment interests. This report also repeats the referral to the smoking cessation specialist (received by all participants after the baseline interview), who was available to discuss treatment options. All users printed their report. A sign-up sheet for meeting with the smoking cessation specialist was also pointed out to all participants after using the decision support system, and this was the point at which users could choose to make an appointment with the specialist.
Measures
The main outcome of the study was whether participants became motivated to quit smoking. Behaviors indicative of motivation were assessed with the behavioral motivation index, a checklist developed for this study that assessed whether the participant met with a smoking cessation specialist to discuss smoking cessation treatments, met with a physician to discuss smoking cessation treatments, attended a cognitive-behavioral treatment group for smoking cessation, initiated a medication treatment for smoking cessation, and initiated a quit attempt without treatment. Research staff verified self-report of the first four indicators with administrative and medical records.
Medical records also provided psychiatric diagnoses and demographic characteristics of the sample. Structured interviews provided their psychiatric history and information about past computer use. Patients' responses to the five-item Fagerström Test for Nicotine Dependence (
51), questions about quantity and frequency of smoking, and an item from the Stage of Change Scale (
52) provided information about smoking characteristics. Attitudes about smoking were assessed with the Attitudes Towards Smoking Scale, an 18-item scale with three subscales (adverse effects, psychoactive benefits, and pleasure) (
53). Previous test-retest correlations have been high (above .81), and the difference between the advantages and disadvantages subscale scores has been shown to predict smoking cessation (
53).
Procedures
Research staff conducted structured interviews at baseline and two months later. At baseline, research staff gave participants a pamphlet that provided information about how to quit smoking (
54) and a referral to a smoking cessation specialist, an experienced addiction counselor whose name and number were on the pamphlet. Participants were told they could make an appointment with this specialist that day or later during the two-month follow-up period. They also were told that they could talk with the specialist about treatment options for smoking cessation. Prescribers of cessation medication were aware of the study and available to all participants at both sites, but they did not have a list of study participants. A cognitive-behavioral smoking cessation treatment group was available to all participants at both sites.
Staff then invited participants from one residential treatment setting (N=21) to use the electronic decision support system within two weeks; individuals from another residential treatment setting (N=20) were invited to use it after a three-month delay (this group served as the wait-list control group). The second treatment setting offered less intensive treatment programming, although the same usual care for smoking cessation was available. All 21 participants in the intervention group used the decision support system once within two weeks; no further use was allowed. Lack of contact between study participants in the two groups prevented any contagion between the groups for the main outcome. In other words, participants who used the EDSS were unlikely to talk with participants from the control group and persuade them to use smoking cessation treatment.
All participants used the program. The specific characteristics of their use and the usability testing of the program among people with severe mental illnesses before this study established that the system was comprehensible, easy to use, and took 30–90 minutes for users to complete.
All study participants continued to receive usual care, which involved psychosocial and medication treatments for mental illness as well as residential, vocational, and other services. Available care for smoking cessation included meeting with a counselor (smoking cessation specialist) or a psychiatrist to discuss smoking cessation, medication for smoking cessation (including nicotine replacement therapy, bupropion, and varenicline), and a weekly cognitive-behavioral therapy group for smoking cessation. All study participants had equal access to these treatments.
Statistical analysis
We used Statistical Analysis Software to conduct the analyses for this study. Using chi square tests and Student's t tests, we evaluated between-group (control and intervention) differences in baseline characteristics that were expected to affect behavioral motivation (past two-month behavioral motivation, Fagerström Test for Nicotine Dependence score, and a difference score calculated from the Attitudes Towards Smoking Scale). We used the chi square test to compare differences between the intervention and control groups on the dichotomized version (zero versus any behaviors) of the behavioral motivation index at baseline and again at follow-up. We used the summed items of the behavioral motivation index at the two-month follow-up to examine group differences in a regression analysis in which we adjusted for baseline differences. Because the behavioral motivation index indicated extravariability (overdispersion), we used a negative binomial regression, which allows the variance to exceed the mean, to model this outcome while controlling for baseline group differences (
55,
56). The beta coefficient for the difference between the two groups was exponentiated in order to interpret its magnitude as an odds ratio (
56).
Results
Study group
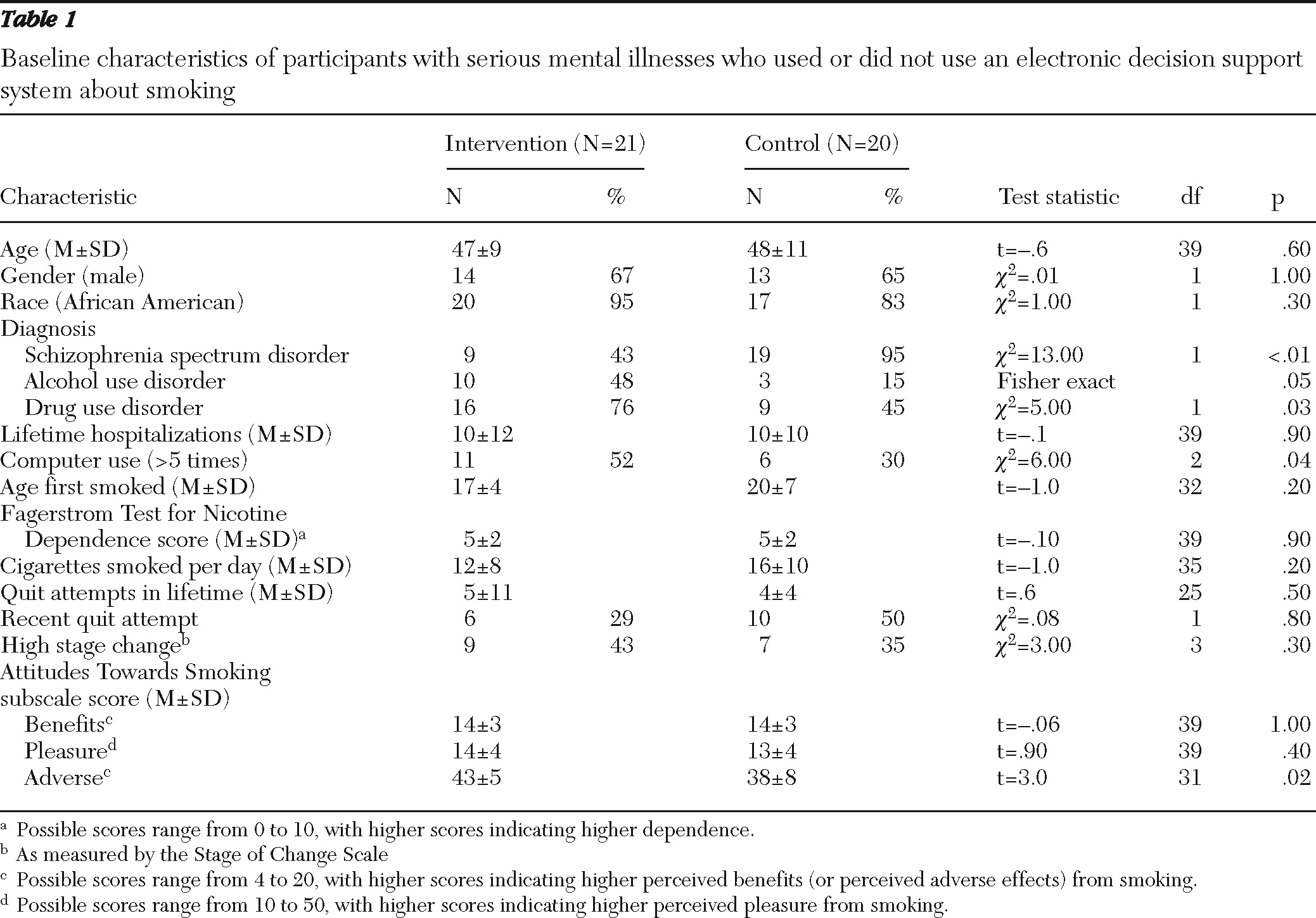
The study group consisted predominantly of middle-aged African Americans with long-term schizophrenia spectrum disorders (
Table 1). Compared with the control group, the intervention group included a lower proportion of individuals with schizophrenia spectrum disorders and a higher proportion of individuals with an alcohol or drug use disorder. The intervention group had a significantly higher mean score on the adverse subscale of the Attitudes Towards Smoking Scale, indicating that the intervention group expressed more concern than the control group about the negative effects of smoking. With computers available in the residence for those in the intervention group, more participants in that group indicated that they had used a computer. Smoking characteristics did not differ between groups.
Baseline smoking cessation motivation behaviors
In the two months before the baseline assessment, six participants (29%) in the intervention group and ten participants (50%) in the control group had tried to quit smoking, either with treatment or on their own, with some using multiple quit strategies. This difference was not significant, suggesting that the treatment and control groups had similar levels of motivation to quit smoking at baseline. The most common baseline motivation behaviors were quit attempts without treatment (N=12, 29%) and use of medication without behavioral treatment (N=8, 20%). Stated intention to quit smoking was also not different between the two groups at baseline.
Outcomes
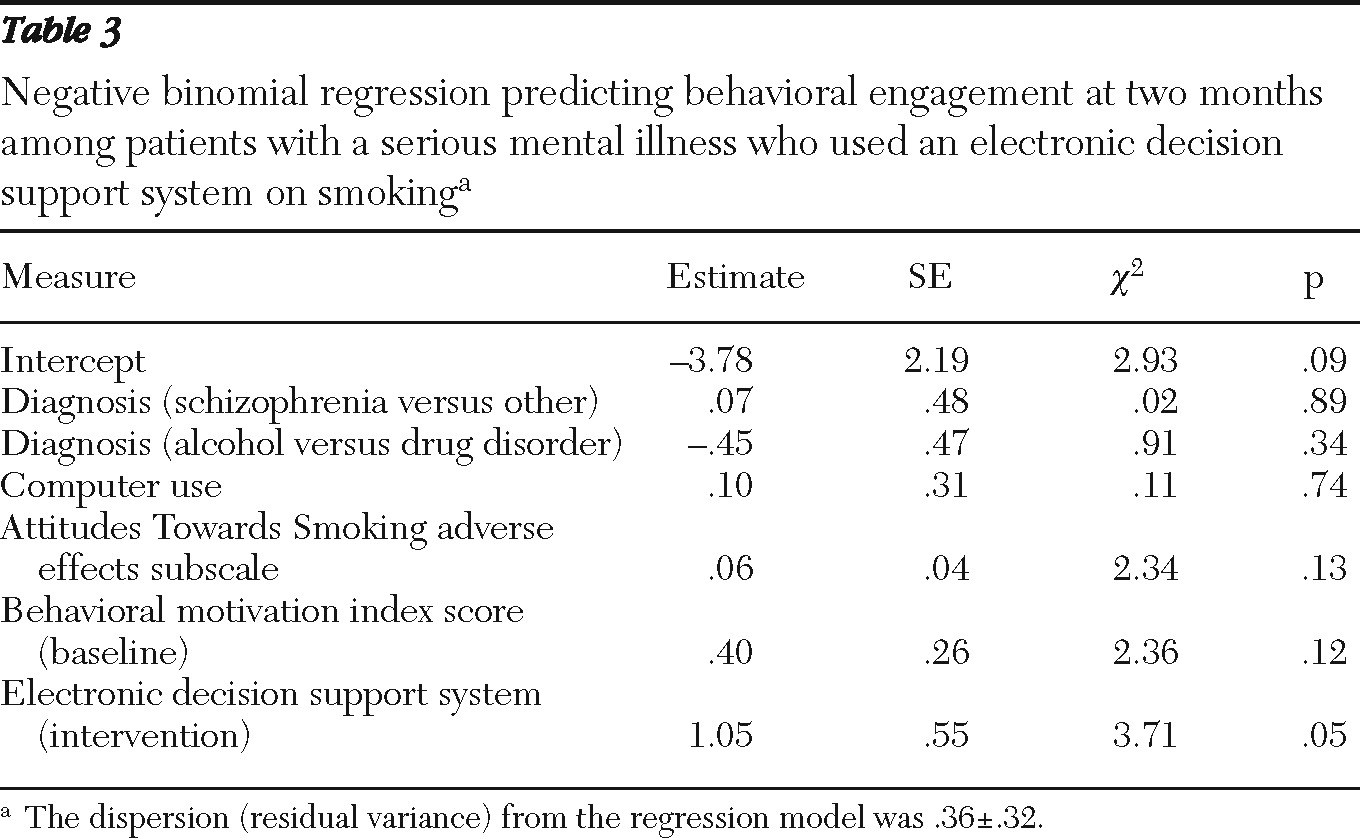
As shown in
Table 2, at the two-month follow-up, participants who had used the decision support system were more likely to have engaged in at least one smoking cessation motivation behavior (67%) than those in the control group (35%) (
χ2=4.11, df=1, p=.04). The effect of the electronic decision support system remained significant in an analysis that controlled for baseline group differences (
Table 3). Further, this analysis indicated that using the electronic decision support system increased the number of expected ways of showing motivation by a factor of 2.97 (exp=1.09), or by about 300%, holding other variables constant. Because the purpose of the system was to engage participants in evidence-based smoking cessation treatment, we also conducted a follow-up analysis that excluded self-quit behaviors. Participants who used the electronic decision support system were more likely to meet with a clinician to discuss or start treatment (43% versus 10%;
χ2=3.84, df=4, p=.05).
Discussion
In this study, participants with severe mental illnesses who used an electronic decision support system were more likely to become motivated to quit smoking over the next two months than smokers who received a pamphlet and referral only. This study was the first test of a newly developed electronic decision support system on smoking cessation for this population. The findings are similar to previous work that found that one (
37) or four (
38) sessions of in-person motivational interviewing and four sessions of in-person education (
38) resulted in most schizophrenia patients' attending an appointment with a smoking cessation provider. Even in our study group, whose members had relatively little computer experience and poor computer skills, use of the computerized tool resulted in behaviors indicative of motivation. Thus the use of a brief computer-based intervention with motivational and educational components may be an effective substitute for individual sessions with an expert clinician.
Extensive research on health behavior change (
46–
48) has shown that attitudes, perceptions of social norms, and perceived behavioral control (or self-efficacy) predict, at least to some degree, motivation or intention to change behavior. We assessed behavioral markers of motivation rather than psychological measures of motivation, because behaviors are a stronger predictor of future smoking cessation among persons with severe mental illnesses (
57). Change in health behavior, including substance use, has not been studied extensively among individuals with severe mental illnesses (
58), although one study demonstrated that attitudes, perceived social norms, and perceived behavioral control predicted antipsychotic medication adherence behaviors in this population (
59). The study reported here was not designed to investigate the mechanisms by which the intervention activated participants, but future work will explore changes in attitudes, perceived social norms, and self-efficacy for engaging in evidence-based smoking cessation treatment.
This pilot study was limited by several factors: the small number of participants, the quasi-experimental study design that involved recruiting participants from different types of residences, the nonequivalent clinical characteristics of the groups, and the differing levels of intensity of the experimental and control interventions. As with all studies using quasi-experimental designs, this study does not rule out the possibility that the findings are a result of site differences. In addition, we did not correct for multiple tests. Nonetheless, this study is the beginning of a stepwise approach to the development of a brief Web-based intervention.
Conclusions
The encouraging results of this pilot study indicate that electronic decision support systems may facilitate the use of evidence-based smoking cessation treatments by people with severe mental illnesses. To confirm and extend these findings, future work should use larger study groups, randomized controlled trials, comparison conditions matched for intensity, longer follow-ups to assess smoking abstinence, and methods that would allow exploration of mechanisms of behavior change.
Acknowledgments and disclosures
This research was supported by the West Family Foundation and the Segal Foundation.
The authors report no competing interests.