According to the Surgeon General's 1999 report on mental health, “All services for those with a mental disorder should be consumer oriented and focused on promoting recovery. That is, the goal of services must not be limited to symptom reduction but should strive for restoration of a meaningful and productive life. … Some people do not seek treatment because they are fearful of being forced to accept treatments not of their choice or of being treated involuntarily for prolonged periods” (
www.surgeongeneral.gov/library/mentalhealth/chapter8/sec1.html).
The patient's experience of coercion is becoming increasingly pertinent to psychiatrists. In modern bioethics, autonomy is considered one of the overarching ethical principles (
1) for protecting patients' liberty and right to make their own decisions for better or worse. To do this, physicians need to provide sufficient information to ensure that patients can make informed decisions. Physicians also must aim for a balance of power in the doctor-patient relationship to ensure that the patient feels like an equal partner in his or her own treatment (
2). Judicial interventions such as community treatment orders (
3) can shift this balance of power, extending the possibility of compulsory treatment beyond the boundaries of hospitals, despite mixed evidence of effectiveness (
4). These types of compulsory actions intuitively appear to increase the risk that patients will perceive care as coercive.
One of the difficulties with coercion as applied to medicine is the relatively flexible way the term is interpreted, in that it is used both subjectively and objectively and occasionally simultaneously. This lack of clarity adds challenge and requires one to differentiate between objective, external acts and internal, subjective attitudes. Coercion when conceptualized in this way is best thought of as an internal subjective state, commonly referred to as “perceived coercion.” One condition for perceived coercion is an action, often a compulsory action (
5). Such actions are a necessary pretext for perceived coercion, which can be considered a side effect of the actions taken by health care professionals. The judicial mandate to treat is the obvious intervention that would be expected to be correlated with perceived coercion, although this is not always the case, even in instances such as compulsory or involuntary treatment orders (
6).
It does not seem to serve patients' best interests to diminish their freedom to make decisions. A justification for any action with this consequence therefore needs to be a “best interests” argument. In a similar way that psychiatrists are aware of and consider the potential side effects of pharmacotherapy when prescribing, an understanding of which actions lead to the experience of coercion can inform our decision making. Understanding what may increase or decrease the experience of coercion will help psychiatrists to understand what actions are least likely to cause this harm and consequently improve their practices.
The aim of this study was to systematically synthesize the evidence regarding perceived coercion in the empirical literature. Thematic articles regarding coercion allow assessment of the hypothesis that coercion is viewed negatively by patients, because they might, for example, experience both coercion and protection associated with the same action. Quantitative studies assessed the hypothesis that interventions associated with coercion can in fact improve a patient's well-being, given that it is commonly measured by examining social functioning or psychopathology. Quantitative studies also enable weighting of the degree to which particular acts may lead to perceived coercion. This supports the “best interest” argument for these compulsory actions, despite any perceived coercion that may result. By addressing both the qualitative and quantitative data sets, a clear view of the lived experience associated with coercion and the possible correlates associated with perceived coercion can be reached.
Methods
We conducted a systematic review of the literature in order to access all studies that have empirically examined perceived coercion of psychiatric patients. By undertaking a structured systematic review, we hoped to overcome any potential for bias that may exist within narrative reviews. We therefore defined inclusion criteria for extracting data and collating them in a uniform manner.
Inclusion criteria
The inclusion criteria for adding an article to this review were kept broad to ensure that all articles reporting on the subjective experience of patients were included. Inclusion criteria were as follows: participants were adults between age 16 and 65; patients were in secondary psychiatric services (or coercion was reported about such care); the article identified how information on coercion was gathered; the study was reviewed for ethical processes and received approval; for qualitative studies, the patient's personal experience of coercion was the primary focus; the article was written or published in English; peer-reviewed tools were used for quantitative data collection; and published peer-reviewed methods were used for qualitative data.
No specific exclusion criteria were identified at the onset of the systematic review.
Search strategy
In light of the diverse nature of the literature on coercion and the reporting of it, a broad-based search strategy was used. The search was conducted electronically, and the references in identified articles were examined for other potential papers. MEDLINE, PsycINFO, and CINAHL bibliographic databases were accessed on February 22, 2009, via the EBSCO platform. The key words “coerci*,” “liberty,” and “duress” were used to identify articles on coercion. The term “psych*” was used to identify the psychiatric literature. Searches were conducted in free-text. These sets of articles were combined with the Boolean term “AND,” and the titles of all identified articles were read. The abstract of any article that was considered to be a candidate for inclusion was then read, as was the full text of all articles deemed suitable after review of the abstract. The references of all read articles were then examined to identify other papers to include.
Data extraction
Data were extracted with a standard tabulated form in order to ensure that similar data were extracted from every paper. The inclusion criteria were checked first to confirm that the paper qualified for inclusion. On confirmation, the data were extracted in a structured fashion.
For qualitative studies, major themes were recorded with key words or phrases that the articles' authors identified. Considering the diversity of thematic interpretation, we extracted the themes that the authors identified and followed the order of importance that the authors assigned to these themes. We then collated the results for side-by-side comparison, rather than synthesizing them together, so that we could examine the complete set of concepts identified.
Quantitative data were extracted in two ways. For correlational and cross-sectional data, all correlations between coercion and other variables were extracted, and the direction and magnitude of connection were noted. For longitudinal data, the primary outcome, an action under investigation, was extracted and its relationship to coercion assessed.
We decided not to undertake secondary analysis of data sets in this review because such analyses would be likely to falsely increase the rates of perceived coercion and thereby make interpretation of the results more difficult. Where it was not clear how data related to coercion—for example, in some articles reporting coercion and multiple outcomes—the authors were contacted for clarification.
Data synthesis
Qualitative and quantitative data were assessed separately—the former to identify themes and the latter to measure correlations and, if possible, effect size. For outcome data, the primary study end points provided the outcomes considered most important by the researchers who conducted the studies. Combination statistical analysis, such as regression analysis, was considered only if the data sets identified were sufficiently homogeneous.
Results
Outcome of the search
The initial electronic search terms identified 5,032 articles. After review of the titles and abstracts, 75 articles were read in full. Of these, 27 articles, providing data on 23 studies, were included in the final analysis. Five of these articles were qualitative and explored the themes of patients experiencing coercion. Twenty-one articles examined coercion by using a broad number of biopsychosocial correlates. Five articles included outcome data. Some studies undertook a variety of quantitative analyses, although none of the qualitative articles included quantitative data. The total number of patients per study ranged from 11 (
7) to 733 (
8). A number of authors were contacted for further information about their studies, although only two (Priebe and Lidz) provided additional information. Others either did not respond or no longer held the original data.
Characteristics of the patients and studies analyzed
Four of the five thematic articles originated from Nordic countries, and one was from the United States. The articles were published between 1993 and 2007. A total of 145 patients were included. All five studies examined the views of patients regarding coercion in association with their hospital care for a major mental disorder. All articles used a formal qualitative analysis technique to extract major and minor themes. These articles focused on patients' lived experiences, rather than objective intervention, although the experiences reported tended to cover forced hospitalization and the involuntary use of psychotropic medications.
The quantitative studies were significantly more diverse in their geographical setting, the care provided, and the methodological design and follow-up. The studies came from ten Nordic, three other European, eight American, and two Australasian research teams. Of these studies, four examined an outpatient population, whereas the remainder looked at coercion associated with hospital-based care. All of the included articles examined perceived coercion as a variable of interest but as part of broad statistical analyses of correlates associated with varied psychiatric intervention, including forced medication, forced admission, and community-mandated treatment. The statistical methods used were heterogeneous; therefore, it was not appropriate to use meta-analytic tools to combine the data for analysis. Although most articles reported simple correlations, some reported regression analyses of various types. Nonetheless, the data provided could be compared in a side-by-side manner. All articles reported on patients in secondary psychiatric care whose treatment was being managed by a consultant psychiatrist. The quality of reporting was inconsistent as to the specific disorders of individual patients, although measures of psychopathology were present for most studies.
Thematic analysis
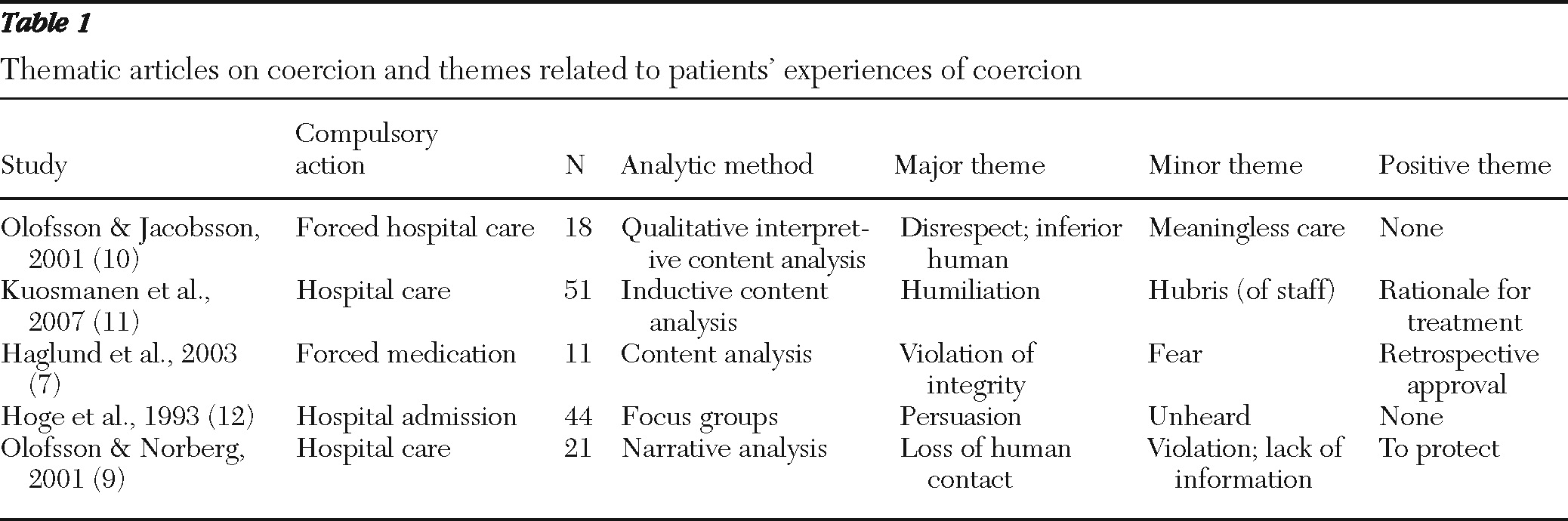
Characteristics of the five thematic articles (
7,
9–
12) are shown in
Table 1. The aspects of care leading to the experience of coercion were broad, but all involved the forcing of “treatment” onto patients against their will. The themes from these articles highlight feelings of violation, disrespect, and not being heard by their clinicians. The most common conceptualization was that of being dehumanized through a loss of normal human interaction and isolation. Using a wide range of thematic analyses, we found that these themes emerged in each article for a range of treatment interventions; this finding was robust. Positive themes were mentioned in three of the five articles from a minority of patients. These tended to emerge in retrospect, well after a patient's hospitalization, and focused on the need or rationale for treatment. These positive themes tended to reflect the social norms and explanations for compulsory care's leading to coercion, rather than the emotive or subjective responses elicited by such care.
Longitudinal analysis
Five articles (
8,
13–
16) examined patients' subjective experience of coercion in prospective trials. These studies, by geographical location, measures used, reporting of data, and time frames, were too heterogeneous to permit meaningful statistical analysis.
Wallsten and colleagues (
13) studied coercion in the context of brief inpatient admission, to a maximum of three weeks, using change in Global Assessment of Functioning (GAF) scores to measure outcome. Coercion was measured with the MacArthur Perceived Coercion Scale (MPCS) and Coercion Ladder. Increasing levels of coercion were not associated with improved or poorer well-being as measured by the GAF. The article gave no indication that coercion was therefore associated with an improved or poorer outcome. Priebe and colleagues (
8) studied one-year outcomes of a large cohort of compulsorily admitted patients after discharge from psychiatric hospitals in Britain. The MPCS was used to measure coercion. In this study readmission was the principal outcome, which was used as a proxy measure for overall well-being; as readmission increases, well-being decreases. This study found no relationship between readmission and coercion once other variables were taken into account by multilevel analysis. The experience of coercion was not associated with readmission, suggesting that feeling coerced into treatment was not associated with improved well-being, which was indicated by a lower rate of hospital readmission.
Using a note-review process to collect data, Bindman and colleagues (
14) studied engagement with community services at one year after hospital admission. Coercion was measured in relation to the compulsory act of admission. The investigators used engagement as the proxy measure of overall well-being from a mental health perspective. As with the above studies, no positive or negative outcomes were associated with perceived coercion. The Health of the Nation Outcome Scale scores, time out of contact with services, degree of compliance, and length of hospital stay all provided no correlation. Using psychopathology as an independent variable in regression analysis, Link and colleagues (
15) examined the association at multiple time points between MPCS score and both quality of life and social functioning. Unlike the above studies, which were embedded in the British social context, the Link and colleagues study was based in America. This study also differed from the above studies in that it examined coercion as experienced in an outpatient setting, both voluntary and involuntary, as opposed to being linked to involuntary hospitalization. Link and colleagues found that the experience of coercion was weakly and negatively related to both quality of life and social function. This effect was independent of whether patients were mandated by a court to receive treatment. The study showed that over time, poorer quality of life was linked with perceived coercion. The researchers concluded that perceived coercion, “generates a cascade of untoward consequences” and is best considered both a consequence of and factor in compulsory psychiatric care over time.
Swanson and colleagues (
16) looked primarily at the effects of involuntary outpatient commitment, examining the relationship between this and quality of life in the context of perceptions of coercion. As part of their analysis they were able to show that although involuntary outpatient treatment improved quality of life, this effect was attenuated by perceived coercion. They noted a relationship between an increase in the assertiveness of treatment providers and mandated community treatment and pointed out that the perception of coercion was not solely related to the judicial requirement of treatment. Their finding raises the vexing question of whether the treatment gains among the patients who experience coercion are unavoidably linked to practices that necessarily lead to perceptions of coercion.
Correlational analysis
The 19 articles providing correlational data (
6,
14–
32) were extremely diverse in their reported findings. Characteristics positively correlated with coercion in one study would have no such correlation, or a negative correlation, in another.
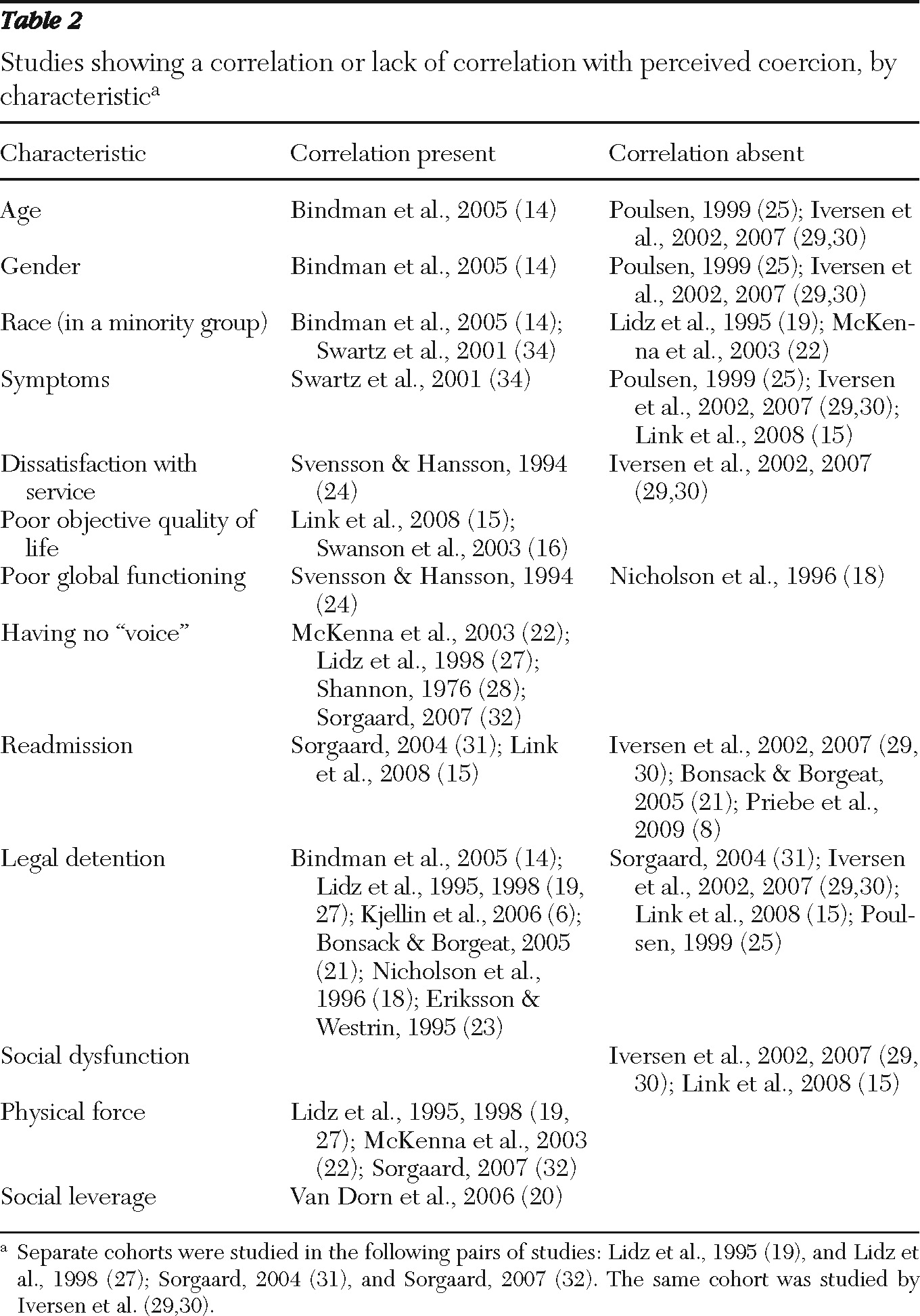
Table 2 summarizes the articles indicating correlations between coercion and mixed biological, psychological, and social comparators. These comparators were either direct measures or proxy measures of wellness as measured in the three domains.
The results of our analysis of the literature indicate that no demographic factor has been consistently found to be associated with coercion (
Table 2). Age, gender, and race all provided mixed results. This was not the case for psychological factors. The objective measures of psychological symptomatology and global functioning provided mixed results; however, the subjective patient-measured tools used in the studies showed a clear link between poorer psychological functioning and experiencing coercion (
15,
16,
22,
27,
28,
32). More specifically, these studies measured general psychological functioning (
15) and a broad domain of “being heard” or “not being stigmatized.” These studies used a variety of tools to measure this domain and present data, using both simple correlational analysis and regression to account for potential confounders. Social measures used as a proxy for well-being included readmission, detention, social functioning, the use of force, and “social leverage.” Unsurprisingly, the use of force and social leverage were clearly positively correlated with coercion. In a similar manner, poorer social functioning was associated with coercion (
15,
29). This was not the case for readmission, an objective measure of symptom control, or legal detention.
Discussion
Although good reviews of objective interventions (compulsory care) have been conducted, this is the first systematic review of the literature on patients' experiences of coercion in mental health, a literature that stretches back more than three decades. As such it gives an overview of what is known about the themes and correlates of coercion. This review highlights patients' perspective on action that leads to coercion and the difficulties in trying to minimize coercion's impact on patients' lives.
The thematic articles provide a clear indication that for patients, coercion is associated with negative concepts, such as feeling dehumanized and unheard. These negative themes do not appear to be in patients' best interests, and this supports the notion that an endeavor to reduce the perception of coercion that may result from interventions is a worthwhile goal. Although some articles report positive themes, these tend to be based on patients' reflections some time after their inpatient experience, indicating a degree of understanding as to why an intervention was undertaken, rather than supporting the notion that patients do not see coercion in a negative way. The conceptualization of coercion for beneficial treatment that some clinicians have proposed (
33) therefore requires a greater body of evidence supporting the notion of beneficial treatment. It could be argued that without such proof, this notion is somewhat flawed.
The longitudinal studies reviewed above do not overwhelmingly suggest that increased benefits can be found over time for patients who experience coercion. Taken as a whole the studies suggest that there is little improvement among patients to offset the negative experience of coercion. The study of Link and colleagues (
15), however, clearly demonstrated the correlation between assisted outpatient treatment and positive outcomes, and this finding is mirrored in the North Carolina study (
34). Of interest to this review is that these studies also found a negative association between coercion and improved outcomes. This can be interpreted to mean that the beneficial effects of this particular compulsory intervention (community treatment orders) are attenuated by the perception of it as coercive. It also raises the question as to whether it is possible to minimize coercive influences further to increase the benefit that such compulsory actions may have.
Despite a significant heterogeneity in results from associative studies, these articles provide some insight into the patient groups that most commonly experience coercion. Perhaps unsurprisingly, physical force and social leverage were closely correlated with perceived coercion. These are explicit examples where one's options are directly reduced in order to garner compliance. This is, almost by definition, compulsion in action: the necessary action for the perception of coercion. Similarly, the patient's lack of a “voice” in treatment decisions was repeatedly associated with perceived coercion, and this finding is mirrored by the qualitative studies suggesting that the process of feeling dehumanized is closely linked to feeling coerced.
What these studies do not make clear is what group, or subgroup, of patients is at greatest risk of perceiving coercion. Intuitively, we might expect, for example, that groups that have been historically marginalized would be at greater risk of feeling coerced. However, the correlational data examined do not support this hypothesis. We might equally expect involuntary commitment to be very strongly associated with perceived coercion, but again, the data were mixed. Because predicting who will feel coerced is difficult, clinicians should routinely consider that their patients may perceive their interventions as coercive and assess this.
This review has a number of limitations that may have affected its findings. Perhaps the greatest difficulty in undertaking a review such as this is accurately identifying studies and data that examined the subjective experience of patients. The empirical literature in this area tends to blur objective compulsory actions and subjective coercive perceptions, even within the same article. It is not sensible to consider coercion from an empirical perspective without considering the action to which it is linked. Nonetheless, in much the same way that consideration of metabolic syndrome when prescribing antipsychotic medication is important both in research and practice, so too is the patient's experience of coercion, particularly in areas of psychiatric practice that might be sensibly thought to increase the likelihood of perceived coercion, such as mandated treatment or forced medication during hospitalization.
This review specifically examined only studies that directly dealt with patients' own experiences, and the quantitative studies we examined used only the MPCS and Coercion Ladder, effectively providing a homogeneous group of patients who experienced coercion as defined by these instruments. Of note also is the fact that no studies in the review were from low- or middle-income countries. They did, however, come from a wide range of Western countries, and as such are potentially generalizable to this patient demographic. The variability in legislation, practice, and intangible variations in patient expectation and experience make interpretation of the data difficult. This issue can be exacerbated by assuming that the failure to find a correlation indicates that the opposite correlation exists, an assumption tempting to make but clearly not supported by evidence. However, each article stands alone and is comparable with the others. This comparability allows us to at least outline the current understanding in the field, even if any conclusions are best considered speculative. Finally, this review focused on patients' experiences of coercion, and these internal experiences are liable to change as society changes around our patients. Whether the experience of coercion can be reduced or mitigated will become clearer from studies that examine which details of compulsory treatment contribute to this experience.
Conclusions
There is, potentially, an element of coercion in every clinical encounter, and it has been argued to be an inescapable component of any human relationship (
35). In psychiatry, perceived coercion has a variety of determinants, many of which are dependent on the quality of the relationship with the clinician, and so is not wholly predicated by a patient's care (
15,
20,
29). It is important that the experience of coercion is assessed routinely and considered as a part of clinical care. More nuanced research is needed to understand the individual experience of psychiatric patients in their own context to enable psychiatrists to optimize treatment management of their patients while maximizing their autonomy.
Acknowledgments and disclosures
The authors thank Viv Kerr and her team in the Hawkes Bay District Health Board library for their assistance with accessing the articles for this study.
The authors report no competing interests.