Seclusion is defined as locking a patient into a special unfurnished room until staff permit the patient to leave (
1,
2). Reducing seclusion rates in mental health settings is a challenging but essential task for professionals and policy makers. Use of seclusion has been criticized for several reasons—first, because patients have reported its negative impact, such as fear, anger, shame, overwhelming feelings of being abandoned, and even traumatic experiences (
1,
3,
4), and second, because many professionals who have been involved in this practice have expressed doubts about the benefits of such invasive measures (
5,
6). Moreover, no scientific evidence is available for therapeutic effects of seclusion as a treatment intervention (
7,
8).
Nevertheless, seclusion continues to be a commonly used intervention on Dutch psychiatric wards. It is difficult to find reliable aggregate data from all Dutch institutes; however, according to estimates based on data from 12 institutes, one in four hospitalized patients, on average, experienced a seclusion episode, with a mean duration of 16 days (
9).
Pragmatic, top-down-implemented seclusion reduction programs have been established and evaluated in recent years (
10–
18). Overall, these programs have succeeded in reducing seclusion rates. However, they are typically multifaceted, and studies have not pinpointed with certainty the program factors that increase professionals' reluctance to use seclusion. In addition, concerns have been raised that seclusion rates may rise again when specific reduction programs end.
To effect a “deep change” (
19) in actual practice—that is, a sustainable change in the attitudes of mental health professionals toward use of seclusion—we must gain insight into factors that influence professionals' decision to use this invasive measure. Mental health professionals who work on inpatient wards regularly face a number of complex situations that involve patients with diverse problems and needs for care. Handling emergency situations is part of the daily work of these professionals (
20,
21). Decisions made in such situations are the result of complex interactions between patient, professional, organizational, and environmental factors (
22–
25).
Recently, Larue and colleagues (
22) reviewed the literature on factors considered to play a role in seclusion and restraint decisions. On the patient side, they found several factors that increase the likelihood of a decision to seclude: age (young and middle aged), gender (male), nationality (immigrant), and diagnosis (schizophrenia or bipolar disorder). Among mental health professionals, they also found several important factors: education level (low), work experience (limited), stress level (overworked and stressed), training, and attitude (negative attitude toward people with mental health problems). However, no empirical evidence has been reported on the impact of these different factors (
22,
26).
The aim of our vignette study was to construct an explanatory model of factors that contribute to the decision of mental health professionals to use seclusion. We addressed the following questions: What is the impact of professional factors on the decision that seclusion is necessary? What is the impact of patient and environmental factors on this decision? Which of these factors have the strongest impact on the judgment that seclusion is necessary?
Methods
We conducted a vignette study to assess professionals' judgment about the necessity of using seclusion. Vignettes are written cases that describe patient, environment, and team characteristics. Vignette studies are increasingly used to gain better insight into the clinical decision-making process of professionals (
27,
28). To select relevant vignette variables, we used an adapted form of the RAND Appropriateness Method, which is a formal group judgment method (
29,
30).
The design of the study can be summarized in four steps: a Delphi procedure to select the variables for vignette construction, construction of the vignettes, data collection, and statistical analysis. [A figure depicting the four steps is available in an online supplement to this article at
ps.psychiatryonline.org.]
Step 1: Delphi procedure
Seven Dutch mental health professionals (three psychiatrists, three mental health nurses, and one psychologist) were invited to participate in an expert panel on the topic of seclusion. All agreed and were present at two separate in-person meetings in June and August 2004. This panel consisted of three mental health nurses, three psychiatrists, and one psychologist. In a modified Delphi procedure consisting of two rounds, these experts were first asked to rate the most important variables influencing practitioners' decision to seclude a patient. The panel reached consensus in the second round on 18 variables, which are described below.
Step 2: construction of the vignettes
Vignettes were constructed by combining the various categories of the 18 variables in unique ways. Because this procedure resulted in too many combinations, we used the generate orthogonal design procedure in SPSS, version 16.0, to reduce the number of vignettes. A series of 64 vignettes was created. Each consisted of four parts, and all were structured identically. The first part described patient characteristics: age, gender, primary diagnosis, psychiatric comorbidity, status of the patient (voluntary or involuntary), seclusion history, and the option of using seclusion in the treatment plan. The second part described the patient's problem behavior: the nature of the problem behavior and the seriousness and direction of danger (toward the patient him- or herself or toward the surroundings). In addition, the possibility of communicating with the patient was described—that is, whether the patient was approachable. The third part of the vignette described characteristics of the context: the type of ward, rooms and space available to patients, atmosphere in the group, and whether the patient's friends or family were supportive of the patient during his or her stay on the ward. The fourth part described the professional team: the culture (open or closed), work shift (day, evening, night, or weekend, including differences in staff-patient ratio during shifts), and the perceived trust of staff in their colleagues.
Step 3: data collection
In September 2004, a total of 128 vignette series with 64 randomly ordered vignettes, accompanied by an instruction manual, were sent to team leaders of 17 different wards of four mental health institutes located in the Netherlands. These team leaders were instructed to ask professionals on their staff to individually read and rate the vignettes on a 9-point Likert scale anchored at the extremes (1, seclusion is absolutely not necessary, to 9, seclusion is absolutely necessary). Also, respondents were asked for sociodemographic data (age and gender) and other background information about their profession, such as education and training, institute, type of ward (open or closed, or a combination), type of care provided, employment hours, work experience, and experience with the use of seclusion, including both the current frequency of participation in seclusion and the number of years of experience in use of seclusion.
Step 4: statistical analyses
In the first step, we analyzed the data with a univariate general linear model (GLM) in which the influence of all factors (the vignette variables and rater characteristics) on outcome (score on the Likert scale) was computed. This method calculated the variance of the scores that can be explained by all factors (R2), as well as the variance explained by specific factors separately (partial η2). The interaction effect of the rater characteristics and the vignette variables was calculated by computing the explained variance of the two groups (vignette and rater variables) and then subtracting the total explained variance.
To identify the specific vignette variables and rater characteristics that most strongly influenced the decision to use seclusion, we conducted two separate univariate GLM analyses. All calculations were done with SPSS, version 16.0.
Results
Raters
A total of 82 of the 128 invited raters (64%) returned the vignettes and provided the requested sociodemographic and background information. The 44 women (54%) and 38 men (46%) had a mean±SD age of 36.9±9.7 years (range 22–59). Most were nurses (N=72, 88%). In addition, three physicians (4%), four psychiatrists (5%), and three social workers (4%) participated. Only four (5%) of the raters were in training. On average, they worked 33.2±4.7 hours a week. Most raters (N=54, 66%) worked on a closed inpatient admission ward. Mean years of clinical work experience was 9.9±8.7.
The model
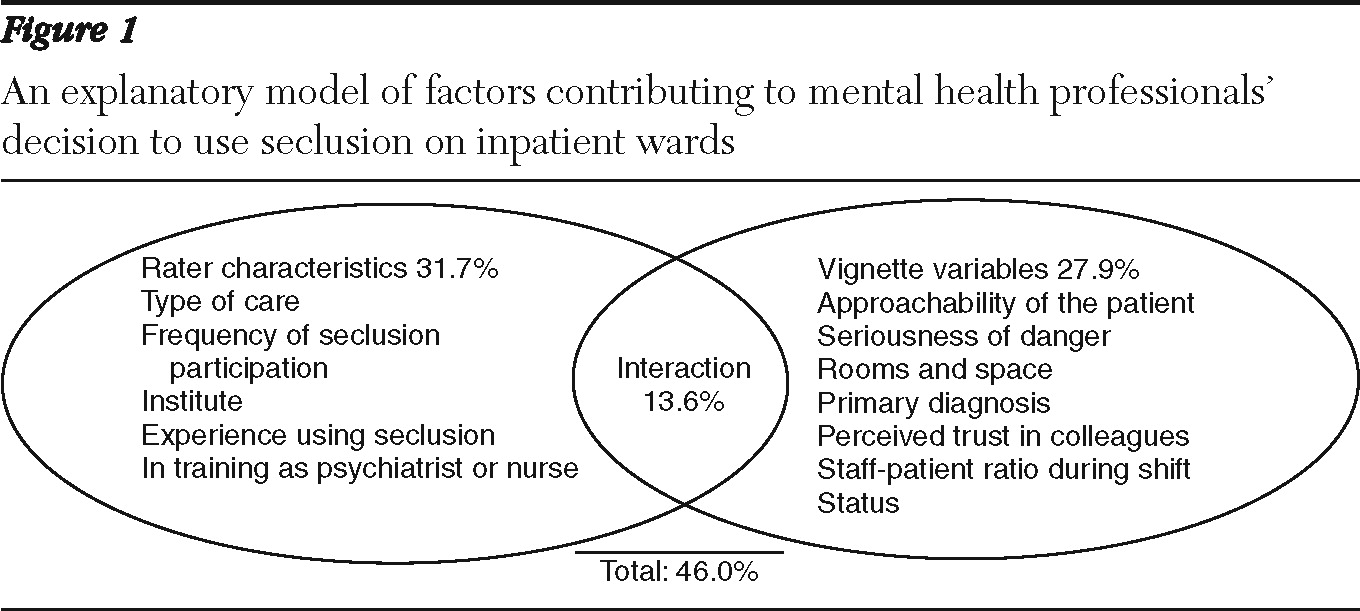
A model that used all data on rater characteristics and vignette variables was constructed that explained 46% of the judgments of these mental health professionals about the necessity of seclusion; 28% could be explained by the variables used in the vignettes, and almost 32% could be explained by the characteristics of the raters. An interaction effect of 13.6 % between the vignette variables and the rater characteristics was found (
Figure 1).
Rater characteristics contributing to the model
Rater characteristics were found to play a prominent role in the judgments of professionals. The work setting (type of care) of the professionals explained 3.6% of the decision to seclude. Professionals who worked on a crisis-intensive care unit or an observation-diagnosis unit provided higher scores on the necessity scale than those who worked on other types of inpatient ward, such as child and youth, forensic, continued care, addiction, and geriatrics wards. Frequency of participation in the practice of seclusion explained 3.5% of the decision. Professionals who used seclusion frequently (more than once a day) also provided higher scores than those who used seclusion less routinely. The institute where professionals worked accounted for 2.5% of the judgment. Those who worked at one of the four institutes participating in the study provided significantly higher scores on the necessity scale than those at the three other institutes. Experience with use of seclusion (number of years) explained 1.8% of the judgment. Professionals who had more seclusion experience provided higher scores. Finally, education accounted for 1.2% of the decision to seclude. Professionals scored higher than their colleagues who were still in training to be a psychiatrist or a community mental health nurse.
Vignette variables contributing to the model
Several vignette variables played a prominent role in judgments about the necessity of seclusion. Approachability was the vignette variable with the most impact (7.6%); the variable specifies whether communicating with the patient was possible or not. The seriousness of danger was the second important variable, accounting for 6.6% of the judgment. Professionals more often decided that seclusion was necessary in cases of acute danger than in cases of imminent danger.
A more practical variable that was also statistically significant and contributed to the model was the availability of individual rooms and space, which explained 2.7% of the judgment. When there was only one living room and patients had to share a bedroom, professionals were more likely to rate the necessity of seclusion as high. Primary diagnosis accounted for 1.6% of the judgment. Raters gave higher necessity scores when the vignettes involved patients with schizophrenia or other psychotic disorders than when they concerned patients with a personality disorder or bipolar disorder.
Perceived trust in colleagues accounted for 1.3% of the judgment. Vignettes stating that professionals had little confidence in their colleagues received higher necessity scale scores. Work shift explained 1.2% of the decision. Raters gave higher necessity scores to vignettes that described a work shift (day, evening, night, or weekend) for which staff-patient ratio was low than to vignettes that described a more adequate ratio. Finally, status of the patient explained 1.1% of the judgment. Patients who were involuntarily admitted received higher scores from the raters than those whose admissions were voluntary.
Discussion
To our knowledge, this is the first study to provide empirical evidence of the relative impact of multiple variables on mental health professionals' judgments about the necessity of seclusion. Use of vignettes allowed us to manipulate an array of realistic variables and to collect information that is difficult to gather in real-life situations (
27).
A model that included variables on patients, the environment, and mental health professionals explained 46% of the decision to seclude. The most notable finding is that characteristics of the mental health professionals contributed at least as much as the combination of patient and environmental variables in the vignettes (32% compared with 28%). The importance of clinicians' characteristics has only been hypothesized. Larue and colleagues (
22) noted that these characteristics might be important factors in the decision to use seclusion but that few studies had examined them. Our results show that professional characteristics are indeed relevant in judgments about the necessity of seclusion.
We found that the treatment setting where professionals work (that is, the type of care provided and the specific institute) was particularly influential in judgments about the use of seclusion. This finding is in line with the idea that the decision to use seclusion is a function of the broader culture (
26,
31,
32). Studies have shown that in cultures where seclusion is a generally accepted practice, both in the workplace and on a national policy level, it is very likely that professionals will use seclusion with little discussion of its merits. Also, professionals' experience with seclusion and the frequency with which they currently used it were important variables in the model. This finding adds to those of other studies in the Netherlands and United Kingdom (
33,
34), which indicated that habit was among the most important factors in professionals' acceptance of this coercive measure.
The vignette factors with the strongest impact on seclusion decisions were the patient's approachability, specifically the impossibility of communicating with the patient, and the seriousness of danger, particularly when the danger was described as acute. Although these factors are not described in these terms in the literature, we found several qualitative studies in which professionals used terms such as “agitation” and “disorientation” in describing their decision to use seclusion (
2,
35). These terms might refer to comparable perceptions of “approachability” and “danger.” In line with other researchers (
2,
36), we found that a schizophrenia diagnosis partly explained the decision to seclude, as did involuntary admission status (
37).
We also found that practical factors, such as the type of rooms and the space available to patients, were important variables in the decision to use seclusion. To our knowledge, these factors have not been described in the literature on seclusion, although several studies have shown that factors such as lack of space increase aggressive incidents (
38,
39). Finally, staffing issues on the ward (staff-patient ratio and work shift) and trust in colleagues played a role in the decision to use seclusion but were on their own less important variables than might be expected. This finding may explain why previous, retrospective studies on the specific influence of staff-patient ratio and experience of staff with the use of seclusion yielded contradictory results and did not explain the complex situation of the influence between the different factors (
37).
Limitations
Although vignette studies of clinical decision making may provide new insights into the judgment of professionals (
20–
22,
24), we cannot be certain that participants' decisions in a real-life setting would be identical to those made in response to the vignettes. Furthermore, although we included a variety of variables selected by experts on the use of seclusion, the list may be incomplete. In addition to the limited number of variables, the number of options per variable was limited. For example, the age of the patient was not a significant factor in the model; however, the vignettes described patients only as older or younger than 50 years. More nuanced manipulation of the age variable may have produced different results.
This study was conducted in 2004 before seclusion reduction programs were implemented. However, we believe that the factors that influenced decisions to use seclusion continue to be relevant. A follow-up study to assess the impact of seclusion reduction programs is in progress.
In addition, our results are primarily based on the judgments of mental health nurses (89% of the participants) in the Netherlands. The study did not include a range of professionals from various countries, which could limit the generalizability of our findings. However, Steinert and colleagues (
26) studied the attitudes of professionals from various disciplines toward use of compulsory procedures in general and found that support for these measures was significantly lower among psychologists and social workers than among psychiatrists and nurses. In light of our findings, this may be explained by the fact that psychologists and social workers generally do not have any experience with the use of seclusion.
Recommendations
On the basis of our findings, we can suggest areas where seclusion reduction programs have a good chance of being successful, thus providing a theoretical framework for the wide range of measures tested in pragmatic seclusion reduction programs.
First, professionals should be trained in methods of communicating with patients, particularly in situations where they perceive the patient as unapproachable. Such training has already been successfully employed in several seclusion reduction programs (
12,
13,
15,
17,
18). Second, professionals should be trained to use deescalation techniques in emergency cases. Examples of successful approaches are positive reinforcement, motivational conversation, cognitive-behavioral change, active listening, and systematic risk assessment (
10,
16,
18). Third, professionals should learn appropriate interventions that are tailored to different situations to calm patients, especially those who are involuntarily admitted and who have a diagnosis of schizophrenia (
15,
40). National guidelines and decision-making frameworks could be important in ensuring use of such interventions (
41). Because psychiatry residents and nursing interns were less likely to deem seclusion necessary, continuing education and career development for mental health professionals are important, and knowledge from individuals training to be psychiatrists or nurses should be shared for this purpose.
Professionals who work on wards where seclusion is common practice—that is on crisis-intensive care and observation-diagnostic units—should regularly have opportunities for supervision. Supervision is also helpful in the process of team building, where professionals learn to trust each other (
42,
43). The finding that experience using seclusion increased the likelihood that it was deemed necessary emphasizes the importance of regularly rotating professionals. Teams should be well balanced with respect to work experience in general and experience with seclusion in particular (
14,
37). Our findings point to other important factors in reducing the use of seclusion, such as ensuring an adequate staff-patient ratio and sufficient individual and group rooms and space for patients. Many countries now use alternative rooms tailored for patients with aggressive behavior (
44).
Conclusions
Our model explained nearly half of mental health professionals' decision to use seclusion. The characteristics of professionals were at least as important as patient variables, such as dangerous behavior and diagnosis, and ward features. Because the perceived approachability of the patient was a key factor, seclusion reduction policies should focus on supporting mental health professionals in their efforts to manage inpatients with problem behaviors in an appropriate way.
Acknowledgments and disclosures
The authors report no competing interests.