Postpartum depression is a serious and debilitating illness that affects appproximately 10%–20% of women who give birth (
1). Available evidence suggests that rates of postpartum depression do not differ by race and ethnicity, but it does not conclusively demonstrate equal rates of illness across groups. Studies in which low-income mothers were systematically screened for clinical criteria indicate that rates of depression during the postpartum period are similar among Latinas, black women, and white women—8% for major depressive disorder and 23% for all depressive disorders in the first three months after delivery (
2,
3). Effective screening tools and treatment strategies for combating postpartum depression have been developed (
4,
5). However, detection and treatment rates for this condition are low (
6–
8), particularly among high-risk women (
9). Untreated postpartum depression can have severe impacts on the health and well-being of the affected woman and her family, including long-term consequences for the cognitive, emotional, and behavioral development of her child (
10–
13).
Although racial and ethnic disparities in depression care are well known and well described (
14–
16), information on treatment of postpartum depression among women from racial and ethnic minority groups is limited (
2,
17,
18). Varying rates of postpartum depressive symptoms reported by women from racial and ethnic minority groups may reflect differences in cultural expectations and perceptions of both motherhood and mental health (
17,
19–
21). Reasons for the complex relationship between race-ethnicity, depressive symptoms, and mental health treatment may include differences in risk factors, perceived need for care, socioeconomic status, and access to health insurance, as well as provider factors and patient-provider communication (
19,
22–
26).
The purpose of this study was to characterize racial and ethnic differences in patterns of postpartum depression-related mental health care among low-income mothers covered by Medicaid who had new-onset depression after delivery (excluding women with bipolar disorder, schizophrenia, or a prenatal history of depression or anxiety). Our primary outcomes included racial-ethnic differences in rates of treatment initiation, follow-up, and continued care. We also examined differences in timing of initiation, as well as the use of medication versus outpatient therapy.
Methods
Data
Data for this study came from the administrative databases of New Jersey's Medicaid program and included deidentified eligibility and enrollment information, as well as medical claims for visits, procedures, and prescription medications from January 2004 through November 2008.
The institutional review board (Office of Sponsored Research) at Harvard Pilgrim Health Care Institute reviewed and waived approval of this study, because the analyses involved the use of only deidentified administrative data.
Study population
Our study population consisted of 29,601 women (13,001 white, 13,416 black, and 3,184 Latina) who gave birth between July 1, 2004, and October 31, 2007, whose deliveries were covered by New Jersey's Medicaid program, and who were continuously enrolled in Medicaid for at least six months before and one year after delivery. All measures were assessed over this period. Women who met the criteria for continuous enrollment had incomes less than 115% of the federal poverty level ($23,747 for a family of four in 2007). By focusing on a population of Medicaid beneficiaries, we were able to examine study outcomes in a group of women of similar socioeconomic status with no variation in insurance coverage—factors that have been sources of confounding in prior studies of disparities in mental health care (
27).
We excluded 841 women with a diagnosis of bipolar disorder or schizophrenia because specific treatment requirements for these illnesses differ from recommended care for depression (
7,
28). In addition, in order to distinguish new onset of depressive illness in the postpartum period from an ongoing episode, we excluded 1,193 women who received any antidepressant medication during pregnancy or who had any prenatal diagnosis of depression or anxiety, because anxiety is often a feature of depressive episodes and may be prone to misclassification in administrative claims data (
7,
29).
Outcome variable definitions
Primary outcomes included postpartum mental health treatment initiation, follow-up, and receipt of continued care. We defined initiation of treatment as having filled a prescription for an antidepressant medication or having had an outpatient mental health visit in the six months after delivery. New Jersey's Medicaid program does not require a diagnosis code for claims payment, and depression diagnoses are generally underreported in claims data (
30,
31). Therefore, a depression diagnosis was not required to indicate treatment initiation.
We identified pharmacy claims for antidepressants by using national drug codes (NDC) and data from First DataBank (San Bruno, California) and the American Hospital Formulary Service (American Society of Health-System Pharmacists). Outpatient mental health visits were defined with codes from the International Classification of Diseases, Ninth Revision (ICD-9), Healthcare Common Procedure Coding System, and Current Procedural Terminology. All individual, family, and group outpatient psychotherapy visits were considered outpatient mental health visits unless they were coded as treatment for substance abuse. Other office visits were considered outpatient mental health visits if the claim included a diagnosis of depressive disorder, dysthymic disorder, or depressive adjustment disorder (ICD-9 codes 296.2, 296.3, 300.4, 301.12, 309.1, and 311).
Among women who initiated mental health treatment in the postpartum period, we defined an acute treatment phase beginning on the date of treatment initiation and extending for 120 days (
32). We examined two measures of continuity of care within the acute treatment phase. First, we measured follow-up, which was defined as either filling an antidepressant prescription for the second time (refill) or receiving a second outpatient mental health visit. Second, we examined rates of continued care, defined as having filled a prescription for an antidepressant medication at least three times or having had at least three outpatient mental health visits during the acute treatment phase. This measure was constructed as a minimum threshold of clinically adequate depression care based on randomized controlled trial evidence on psychotherapeutic treatment of postpartum depression (
33), Healthcare Effectiveness Data and Information Set measures for antidepressant use (
34), and recommendations for the care of women with postpartum depression (
4).
Among those initiating care, secondary outcomes included timing of treatment initiation and the use of different treatment modalities (medication versus psychotherapeutic care). Time from delivery to treatment initiation (measured in days) was assessed among all women who initiated care, because earlier initiation may mitigate the potential negative maternal and child impacts of untreated illness (
35,
36). Given evidence of racial-ethnic differences in depression treatment patterns among pregnant Medicaid enrollees (
18), we also examined racial-ethnic differences in whether women received at least one antidepressant prescription or one outpatient mental health visit in the acute treatment phase as well as the odds of receiving a medication refill or second visit among women initiating each treatment modality.
Race-ethnicity
We used each woman's race and ethnicity as self-reported on enrollment in Medicaid, which were categorized as black, white, or Latina. We excluded women in the six other race-ethnicity categories from this analysis because of small numbers (N=1,354). Studies using administrative data support the validity of self-reported race and ethnicity variables for white, black, and Latina categories (
37–
39). Consistent with prior research, our statistical analyses used white women as a comparison group for both black women and Latinas.
Covariates
Other covariates included age at delivery, drug dependency, diabetes, high-risk pregnancy, preterm birth, and cesarean delivery. Age was self-reported at enrollment, and other covariates were defined according to diagnosis and revenue codes. We defined drug dependency by diagnosis of substance use disorder (ICD-9 codes 303, 304, or 305 and excluding 305.1 and 305.8). Diabetes was defined as having a diagnosis of diabetes mellitus or gestational diabetes (ICD-9 codes starting with 250 or 648.0) or filling a prescription for a diabetes medication (that is, American Hospital Formulary Service designation as an antidiabetic agent). We identified high-risk pregnancy by ICD-9 diagnosis (ICD-9 codes starting with V23). ICD-9 codes 644.20 and 644.21 indicated preterm birth before 37 weeks gestation, and diagnosis-related group codes (370, 371, 650, and 651) indicated cesarean delivery.
Statistical analysis
We used patient-level logistic regression models and Cox proportional hazards models in our analyses of racial-ethnic differences in study outcomes. All regression models controlled for the covariates mentioned above. Logistic regression models including potential interactions were evaluated with likelihood ratio tests, which indicated that such models did not provide additional information. Therefore, results from models excluding interaction terms are presented. County of delivery was not included in final regression models, per recommendations for disparities research (
27,
40). We examined this variable in sensitivity analyses, however, and the results were consistent with the findings reported below. On the basis of final logistic regression models and mean covariate values, we also present results as predicted probabilities for an “average” white, black, or Latina woman: age 25–29 at delivery, without diabetes, high-risk pregnancy, or drug dependency and no evidence of a preterm or cesarean delivery. This method has been used in mental health disparities research to highlight racial-ethnic differences in predicted health care utilization and expenditures among patients with the same clinical characteristics (
27,
41).
We used Cox proportional hazards models to examine racial differences in time from delivery to treatment initiation among women who received at least one antidepressant prescription or outpatient mental health visit. In these models, we evaluated and could not reject the proportional hazards assumption. All analyses were conducted with SAS Statistical Software, version 9.1.
Results
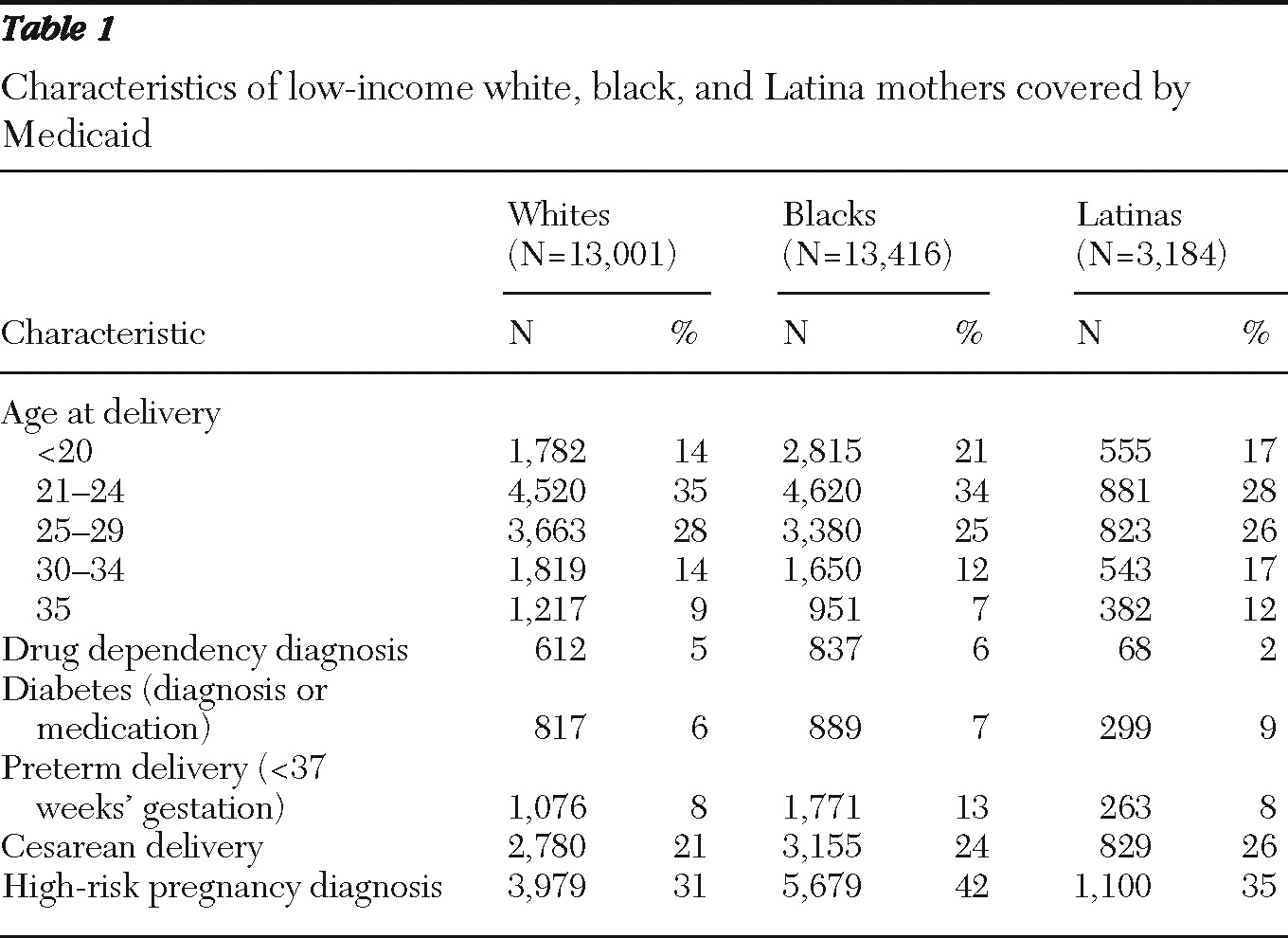
Descriptive statistics for women in the study population are presented in
Table 1. Overall, white, black, and Latina women had comparable demographic and clinical profiles. However, white women tended to have slightly lower rates of pregnancy- and delivery-related complications, compared with black women and Latinas.
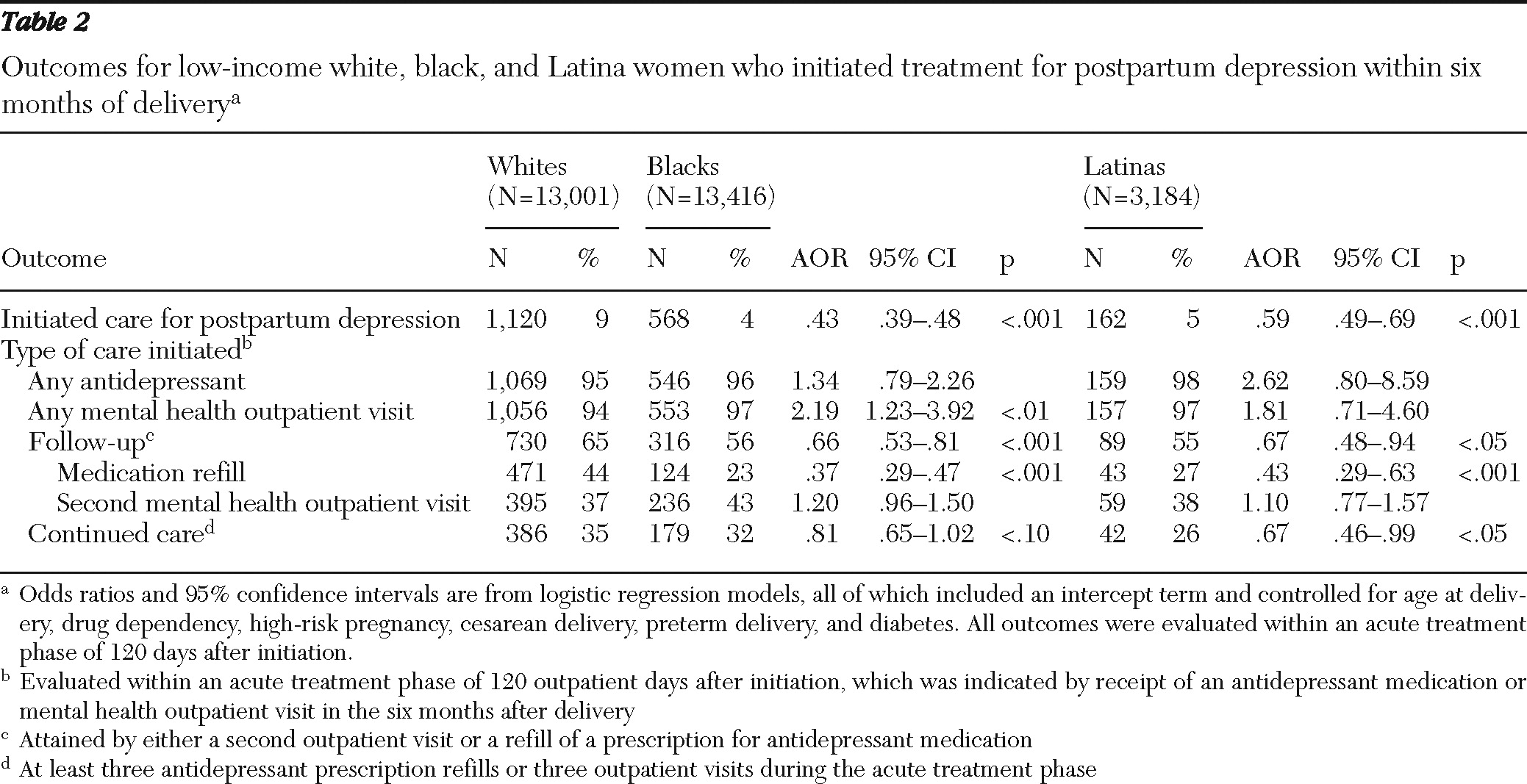
Table 2 presents mean values for study outcomes as well as adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from patient-level logistic regression models for the primary study outcomes, enabling comparison of black women and Latinas with white women. A higher percentage (9%) of white women initiated antidepressant treatment or outpatient mental health services in the six months after delivery, compared with black women (4%) and Latinas (5%). Among those who initiated treatment, there were differential rates of follow-up and receipt of continued care by race-ethnicity. Also, there were markedly higher rates of follow-up on initial antidepressant use among whites (44%) than among blacks (23%) and Latinas (27%).
After analyses controlled for relevant demographic and clinical factors, the odds of initiating treatment remained significantly (p<.001) lower for blacks (AOR=.43) and Latinas (AOR=.59), compared with whites. Other predictors of treatment initiation included pregnancy- and delivery-related complications (results not shown). As for care received by those who initiated treatment, blacks and Latinas were less likely than whites to have any follow-up treatment (blacks, AOR=.66, p<.001; Latinas, AOR=.67, p<.05) or continued care (blacks, AOR=.81, p=.069; Latinas, AOR=.67, p<.05).
Focusing on differences in treatment modality, we found that most women who initiated treatment received at least one antidepressant prescription and at least one outpatient mental health visit. However, compared with white women, black women receiving treatment had higher odds of having an outpatient mental health visit (AOR=2.19). Also, black women and Latinas who filled an initial antidepressant prescription had significantly (p<.001) lower odds than whites of refilling a prescription within the 120-day acute treatment phase (black women, AOR=.37; Latinas, AOR=.43).
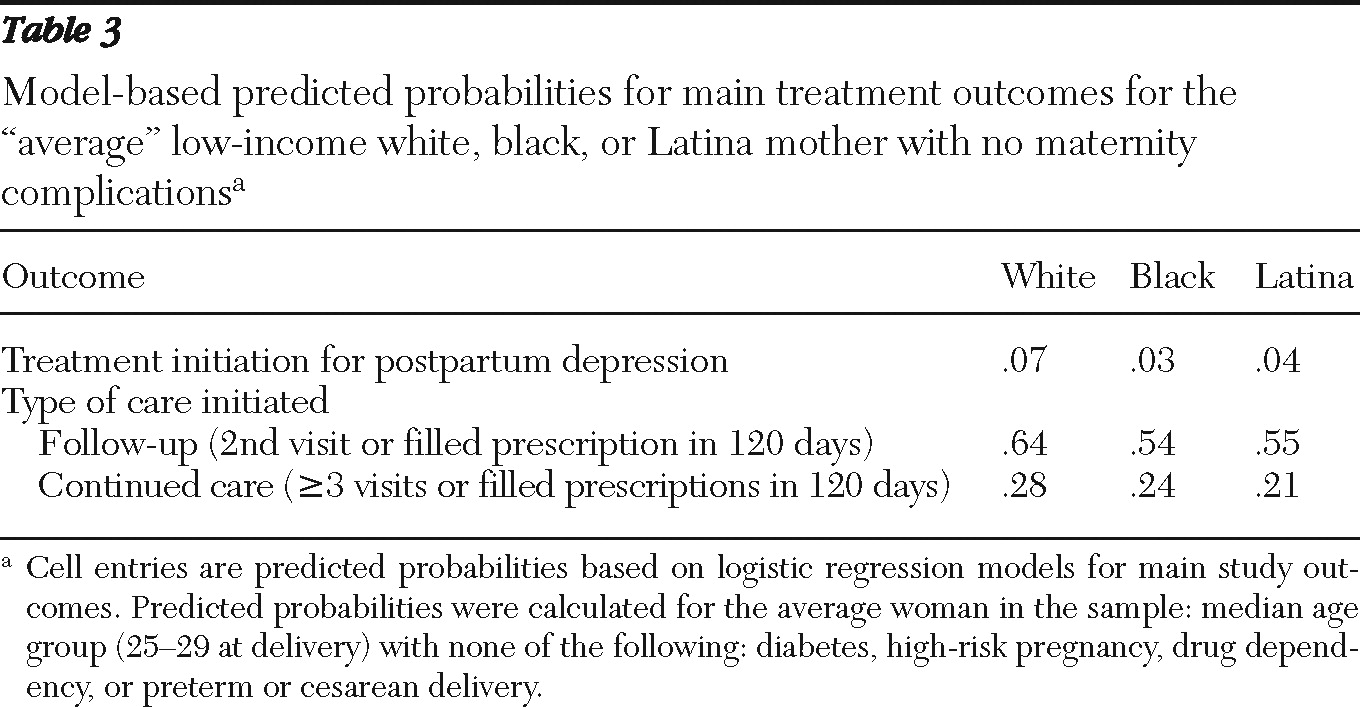
Table 3 presents predicted probabilities of experiencing the main study outcomes by race-ethnicity for an “average woman,” with mean covariate values (see
Table 1). The predicted probability of treatment initiation differed by race: 3% for a black woman, 4% for a Latina, and 7% for a white woman. Racial-ethnic differences in the predicted probabilities of follow-up and continued care persisted among women who initiated care, with an average white woman being more likely to receive follow-up (64%, compared to 54% and 55% for a black woman or Latina, respectively) and continued care (28% versus 24% and 21%, respectively). Racial-ethnic variations in predicted probabilities were similar for black women and Latinas who had pregnancy-related conditions or delivery complications compared with white women who had the same clinical profile.
Results of a survival analysis indicated that among those who initiated care, time from delivery to treatment initiation was longer for blacks (hazard ratio=.89, CI=.81–.99) and Latinas (hazard ratio=.82, CI=.69–.96) than for whites.
Discussion
We found low levels of postpartum depression treatment among all low-income women in our study, with particularly low treatment initiation rates for black women (4%) and Latinas (5%). Although underlying rates of illness could not be identified in this study, prior research indicates a diagnosed prevalence of approximately 23% among low-income women (with half characterized by postpartum onset of illness) (
3) and similar rates of illness across racial-ethnic groups (
2). The differences in initiation and continuation of care uncovered in this study imply that a disproportionate number of black women and Latinas who suffer from postpartum depression do not receive needed services. These differences represent stark racial-ethnic disparities potentially related to outreach, detection, service provision, quality, and processes of postpartum mental health care. Although suboptimal detection and treatment rates are not uncommon for this condition or in this population (
7,
42,
43), these results emphasize that postpartum depression remains an underrecognized and undertreated condition for all low-income women, especially for those from racial and ethnic minority groups.
Whereas extensive prior literature has detailed racial and ethnic disparities in mental health care (
14–
16,
44), this study presents the first evidence of racial-ethnic differences in the utilization patterns of postpartum depression-related mental health services. We found that blacks and Latinas were less likely than whites to initiate mental health care after delivery, with whites having approximately twice the odds of starting treatment, in spite of evidence of similar rates of underlying illness (
2,
3). In the context of postpartum depression, time from delivery to treatment initiation is of particular importance, in that early detection and treatment can minimize the potential negative impacts of the illness (
35,
36). In our study population, black women and Latinas were less likely to initiate care, and among those who initiated care the time from delivery to treatment initiation was significantly longer for blacks and Latinas than for whites.
We also found that racial and ethnic differences in care persisted among those who began treatment. Even though they initiated care at lower rates than whites, black women and Latinas who started treatment had lower chances of receiving follow-up or continued care compared with white women who initiated treatment. This study also revealed racial-ethnic differences in type of care (antidepressant medication versus outpatient visits) among those initiating treatment. Black women had higher odds of initiating care in an outpatient mental health setting, but blacks and Latinas who initiated antidepressant use had much lower chances than white women of refilling a prescription. Prior research has revealed that preferences for depression treatment modality differ by race, with blacks and Latinas generally preferring psychotherapy over antidepressant medications (
15,
45–
47) As such, this finding may provide information about patient desire or willingness to refill a prescription or clinician response to patient preferences.
By using data for continuously eligible Medicaid recipients, we were able to measure racial-ethnic differences in care among women with similar income levels and health insurance coverage. However, Medicaid administrative claims data present a number of limitations. The data in our study lack personal variables (such as information on treatment preferences and perceived need) as well as clinical variables (such as prior history of depression or severity of symptoms), which may have enhanced our analysis and interpretation. Services not reimbursed by Medicaid are not captured in claims data, and thus we were not able to measure sources of community-based support for postpartum depression. We used the gold standard of self-reported race-ethnicity data in this study. However, because women in the study were allowed to identify themselves using only one racial or ethnic category upon enrollment in Medicaid, there is a potential for misclassification, particularly for multiracial or multiethnic women.
A limitation of this study is that we could not use depression diagnoses to define women who suffered postpartum depression, because depression is often undercoded in administrative data (
30) and New Jersey's Medicaid program does not require a diagnosis for payment of utilization claims. Therefore, it is possible that we included in our study women with a mental health condition that was not related to depression or women with some treatment claims for non-depression-related mental health services. However, we addressed this limitation through several means. First, we excluded patients with a diagnosis of schizophrenia or bipolar disorder, conditions that are generally more reliably coded than depression in claims (
31). Also, in New Jersey's Medicaid program, providers receive higher reimbursement for diagnoses such as bipolar disorder and schizophrenia, thus improving the likelihood that these diagnoses will be coded in the claims (and that such patients would be excluded from our study sample). Further, 95% of women in our study sample who initiated care received at least one antidepressant prescription, indicating that for nearly all of these women, the treating clinician's diagnostic impression was of a postpartum clinical syndrome in the depression-anxiety spectrum.
Conclusions
Our study presents evidence of low rates of postpartum depression treatment initiation and continuation, indicating barriers to care among low-income mothers; racial-ethnic disparities imply additional challenges for black women and Latinas. The presence of such disparities points to the need for clinical and institutional policies and programs to address the particular barriers to mental health care faced by black women and Latinas in the months after delivery.
The prenatal and postpartum periods represent a time of unique vulnerability to mental illness as well as complex emotions and expectations about motherhood (
20,
29). Regular contact with the health care system during this time provides a feasible opportunity to address potential underdetection and undertreatment of postpartum depression in the clinical context, and alternate models of and innovations in postpartum health care delivery (such as home health visits after childbirth) may allow for more flexible and responsive care for new mothers. Specific barriers to care among low-income black women or Latinas may include stigma, communication problems, and logistical issues (including insurance coverage, time constraints, child care, and transportation) (
48,
49). Prior literature suggests that addressing logistical challenges, cultural beliefs, and patient-provider communication may be helpful in meeting mental health treatment needs (
50), and such efforts should be incorporated into the provision of postpartum health care, both in primary care and specialty mental health settings. However, there is a need for further research on barriers to postpartum depression care, on interventions aimed at reducing barriers, and on racial-ethnic differences in patient perceptions and experiences of both mental health and motherhood among low-income women.
Acknowledgments and disclosures
The authors gratefully acknowledge support from the Thomas O. Pyle Fellowship and the Fellowship in Pharmaceutical Policy at Harvard Medical School and the Harvard Pilgrim Health Care Institute (Dr. Kozhimannil); the Community Benefit, Kaiser Permanente Northern California (Dr. Adams); grant K01HS018072 from the Agency for Healthcare Research and Quality (Dr. Trinacty); the Robert Wood Johnson Foundation Investigator Award in Health Policy Research (Dr. Huskamp); and grant K01MH071714 from the National Institute of Mental Health (Dr. Busch). The authors acknowledge input and advice provided by Bernard Harlow, Ph.D., Michael Law, Ph.D., and Stephen Soumerai, Sc.D. They are also grateful for the assistance of Dominic Magnolo in facilitating access to New Jersey's Medicaid administrative claims databases.
The authors report no competing interests.