Serious mental illnesses (including schizophrenia, bipolar disorder, and other psychotic disorders) are associated with substantial functional impairment, high health care costs, and poor outcomes, including premature mortality (
1,
2). Poor outcomes have been attributed to co-occurring medical conditions, notably cardiovascular disease, which is the most common cause of mortality in this group (
3). Still, evidence suggests that in general, persons with serious mental illness are less likely than those without serious mental illness to receive adequate care for medical conditions (
4–
7), and there has been an increased call to improve medical outcomes for persons with serious mental illness (
8).
Given the intensity of treatment and management required for serious mental illness, many of these individuals consider the mental health program their “home” site for care, even within highly integrated health care systems such as the Veterans Health Administration (VHA) (
9). Medical services for persons with serious mental illness are often provided by primary care clinicians who are typically external to a mental health clinic. Moreover, many individuals with serious mental illness may have trouble navigating general medical services when referred for care (
10), and many general medical providers lack the time or tools to effectively address the general medical needs of those with serious mental illness that can be complicated by psychiatric symptoms (
11).
Integrating general medical care into mental health specialty programs is an optimal strategy for improving quality of care for individuals with serious mental illness (
12). Prior studies on integrated care models in mental health settings have chiefly involved randomized controlled intervention trials of colocated medical teams in mental health clinics compared with usual care. Notably, in two studies, colocation compared with usual care (
12,
13) was associated with improved processes of care for patients with mental disorders.
However, the extent to which general medical colocation models have been further disseminated beyond the research trial stage, and whether they are associated with improved quality of care in routine care settings beyond intervention trials, have not been demonstrated. Several federal agencies, including the Substance Abuse and Mental Health Services Administration (
8) and the U.S. Department of Veterans Affairs (VA), have called for programs to improve the quality of medical care for persons with serious mental illness. Colocated medical programs have the potential to improve quality by increasing access and continuity of medical care and in turn constitute a medical home for those with serious mental illness. The VA, with its single-provider network and common electronic medical record system, provides an optimal, naturalistic setting to assess whether colocated programs are associated with improved quality of care for persons with serious mental illness. Using data from the largest national survey of VA mental health programs to date and from the VA's extensive electronic medical record resources, we conducted this observational study to determine the association between colocation of general medical services and quality of medical care for patients with serious mental illness receiving care in VA mental health clinics.
Methods
This cross-sectional study is based on data from the VA National Psychosis Registry (NPR), which includes all patients who had a diagnosis of serious mental illness in fiscal year (FY) 2006 or 2007, who were also included in the VA's External Peer Review Program (EPRP) FY 2007 random sample, and who received care from VA facilities with complete data from the 2006 VA Mental Health Program Survey (
14). EPRP is a comprehensive chart review for guideline-based processes and outcomes of care for general medical conditions and prevention screens for patients receiving care in the VHA (
15). The Mental Health Program Survey is a national survey on organization and integration of care of VHA mental health programs throughout the 50 states (
14). This study was reviewed and approved by local institutional review boards.
Patient selection: NPR
Patients with at least one diagnosis of serious mental illness in FY 2006 or 2007 were identified from the NPR. Serious mental illness diagnoses included schizophrenia, including schizoaffective disorder (
ICD-9 codes 295.0–295.4 and 295.6–295.9), bipolar disorder (codes 296.0–296.1 and 296.4–296.8), or other psychotic disorders (297–297.9 and 298–298.9) (
16,
17). The NPR also includes information on diagnoses (
ICD-9 codes) of medical conditions and other psychiatric disorders, as well as data on inpatient and outpatient utilization and demographic characteristics. To link patient-level data from EPRP with facility-level data from the Mental Health Program Survey, a primary facility was assigned to patients on the basis of where they made most of their mental health outpatient visits in FY 2007.
Dependent variables: patient-level EPRP data on quality of care
Data on quality (processes and outcomes) of care were ascertained from the EPRP FY 2007 chart review data. EPRP involves a yearly random sample of medical record reviews on quality of care of VA patients throughout the 50 states. Details regarding the EPRP sample are available elsewhere (
15). In brief, EPRP medical record reviews are conducted quarterly for each fiscal year by trained nurses for a randomly selected national sample of patients who made at least one outpatient visit in the quarter. Patients are eligible for EPRP chart review if they had an outpatient visit in the immediately preceding month, had an outpatient visit 13–24 months before the chart review month, and did not have a chart review in the preceding three months. Women as well as those with chronic medical conditions, such as diabetes, are oversampled in order to obtain sufficient sample sizes. Random selection is conducted monthly and stratified by VA facility to allow for a minimum number of patients at each facility for each quarter.
EPRP chart abstractors ascertain quality-of-care information (examining processes and intermediate clinical outcomes of care in accordance with clinical practice guidelines). For this study, nine available EPRP quality indicators were included because they strongly reflect elements of integrated care for general medical conditions and represent conditions that disproportionately affect patients with serious mental illness. EPRP process-of-care indicators included diabetes-related foot exam; diabetes-related retinal exam; screenings with a standardized assessment for colorectal cancer (ages ≥50, defined as receipt of a colonoscopy), breast cancer (women only, defined as receipt of mammogram), and alcohol misuse; and receipt of at least three tobacco-cessation counseling sessions. Outcome indicators included good control of hypertension (blood pressure <140/90 mmHg), glycosylated hemoglobin level (HbA1C <9%), and lipids, particularly low-density lipoprotein (LDL <120), for patients with diabetes. All of these indicators pertained to processes of care received or outcomes experienced within the past 12 months, to reflect minimum necessary standards of care. Each indicator has a different denominator depending on the eligibility criteria of that measure. [Details on EPRP results among patients without serious mental illness are available as an online supplement to this article at
ps.psychiatryonline.org.]
Independent variables: facility-level Mental Health Program Survey
The Mental Health Program Survey is a comprehensive assessment of organization and integration of general medical and substance use disorder services within mental health clinics or programs in VA facilities. Details of the survey are described elsewhere (
14). In brief, survey questions were derived from two previously established program surveys widely used in the VA to assess the organization and integration of VA services: the Primary Care Practices Survey (
18) and the Drug and Alcohol Program Survey (
19). Content validity was further evaluated on the basis of input from ten experts in the VHA with extensive knowledge regarding integrated mental health, substance use disorder, or general medical services for persons with serious mental illness.
After refinement, the survey was sent to directors of VA mental health programs. As of FY 2007, 133 out of 139 VA medical centers had a mental health program and thus were eligible to receive the survey. Consistent with previously established organizational surveys (
20), in this survey the director of each VA mental health program was designated as the key informant for the program survey and defined as the person who was chiefly responsible for the management and implementation of policy decisions regarding the organization and delivery of care for veterans with serious mental illness at their facility. Overall, 107 (81%) out of 133 mental health program leaders completed the survey.
Colocation of general medical services was defined on the basis of response options to the survey question, “Which of the following best describes the location of the nearest VA general medical services available for your patients in your mental health program?” Response options included “within the mental health clinic,” “in a different clinic but the same building,” “in a different building but same medical complex,” or “different location/complex.” Colocation was defined as whether the general medical services were located within the mental health clinic only. Other organization-level covariates ascertained from the survey included academic affiliation, defined as whether the program had a psychiatric residency program (yes or no), program staffing ratio (ratio of nurses, nurse practitioners, and physician assistants to physicians), and VA facility size (defined as the number of unique patients at the facility, categorized as >1,000 or ≤1,000 patients), all of which have been found to correlate with quality of care based on previous organizational studies (
20–
22).
Analyses
Bivariate analyses were used to assess the association between program and patient factors and colocation and quality of care. Patient-level independent variables available from the NPR included age, sex, race (African American versus another race), marital status (married or not married), service-connected disability (any versus none), Charlson Comorbidity Index score, co-occurring psychiatric diagnoses (any anxiety disorder, including posttraumatic stress disorder, or a substance use disorder), and number of primary care visits made in FY 2007. Multivariate logistic regression analyses were run to determine the independent association between colocation of services and quality of care, which was based on each EPRP indicator; analyses adjusted for site organizational factors from the survey and patient-level characteristics from the NPR. Generalized estimating equations based on SAS Proc GENMOD were used in the multivariate analyses to account for the clustering effect of facilities (in other words, patients from the same facility may share similar characteristics).
Results
A total of 241,683 patients had diagnoses of serious mental illness in FY 2006–2007, and of those, 105,100 (44%) received care from the 107 sites with complete mental health program survey information. Of the 105,100 patients with serious mental illness, 7,514 (7.1%) were included in the FY 2007 EPRP random sample cohort. The 105,100 patients did not differ significantly in demographic characteristics compared with those in the overall cohort of 241,683. [Details on demographic characteristics are available in an online supplement to this article at
ps.psychiatryonline.org.] The 7,514 patients from the EPRP random sample also did not differ significantly from the cohorts of 105,100 or 241,683 patients, with the exception of gender and Charlson Comorbidity Index score. In the EPRP sampling frame, women and those with key medical comorbidities such as diabetes were oversampled in order to achieve sufficient numbers for analyses (data not shown).
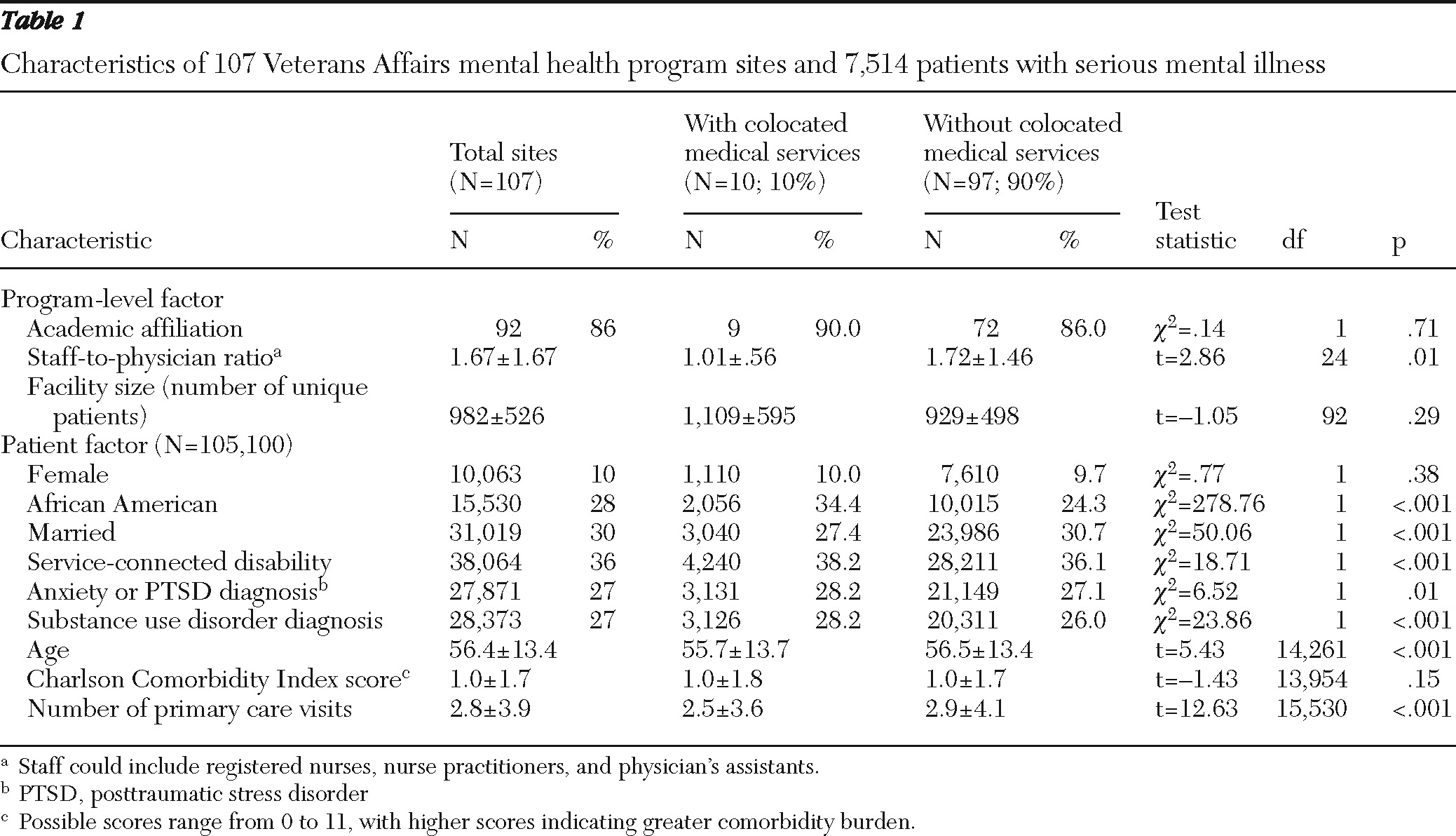
Of the 107 mental health programs, ten (10%) had colocated general medical clinics. Programs with colocated clinics had a lower staff-to-physician ratio than programs that were not colocated, yet no other organizational factors were associated with colocation (
Table 1). Although patient factors were significantly different across programs by colocation status, the magnitude of these differences was small for the most part because of the large sample size (
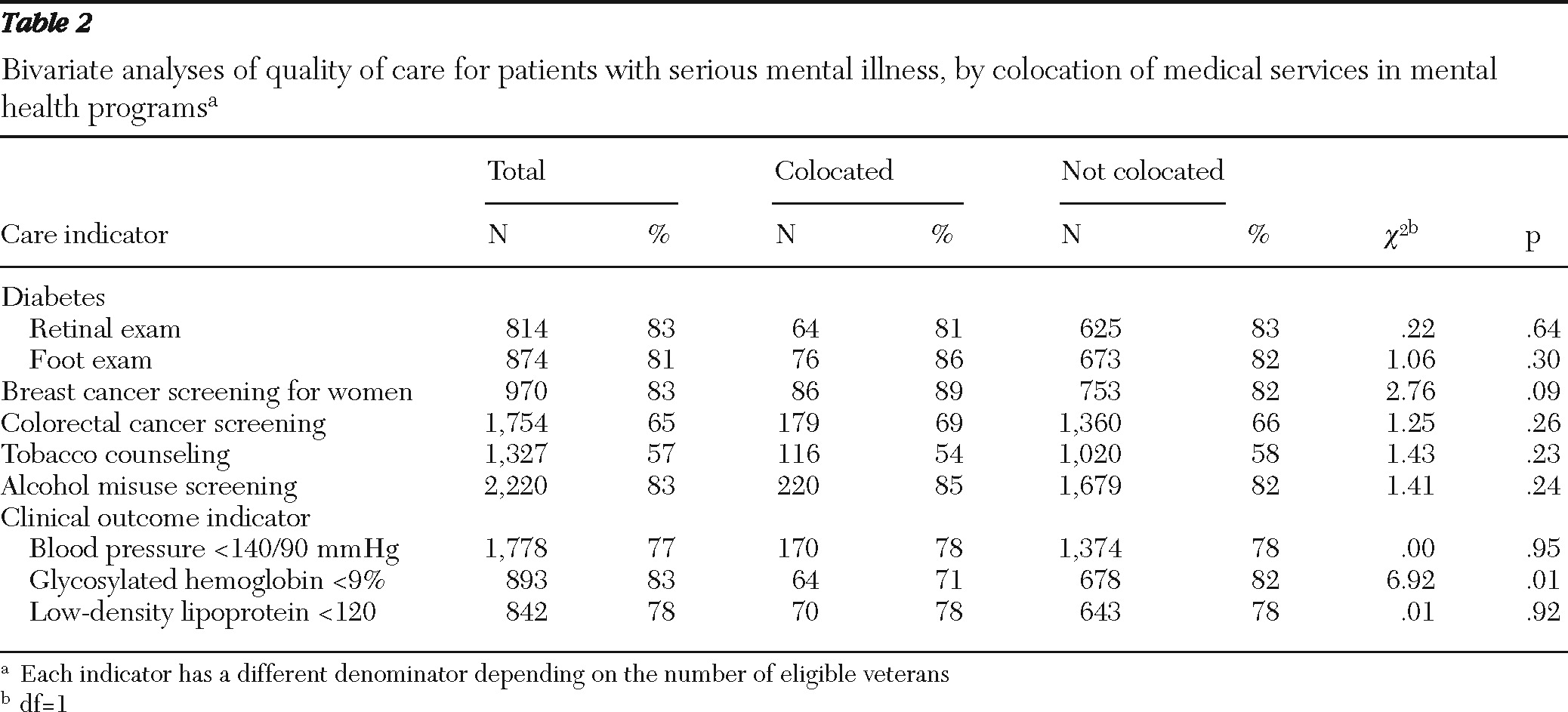
Table 1). Unadjusted analyses revealed that colocation of services was associated with a higher average number of patients with HbA1C <9%, compared with services that were not colocated (
Table 2).
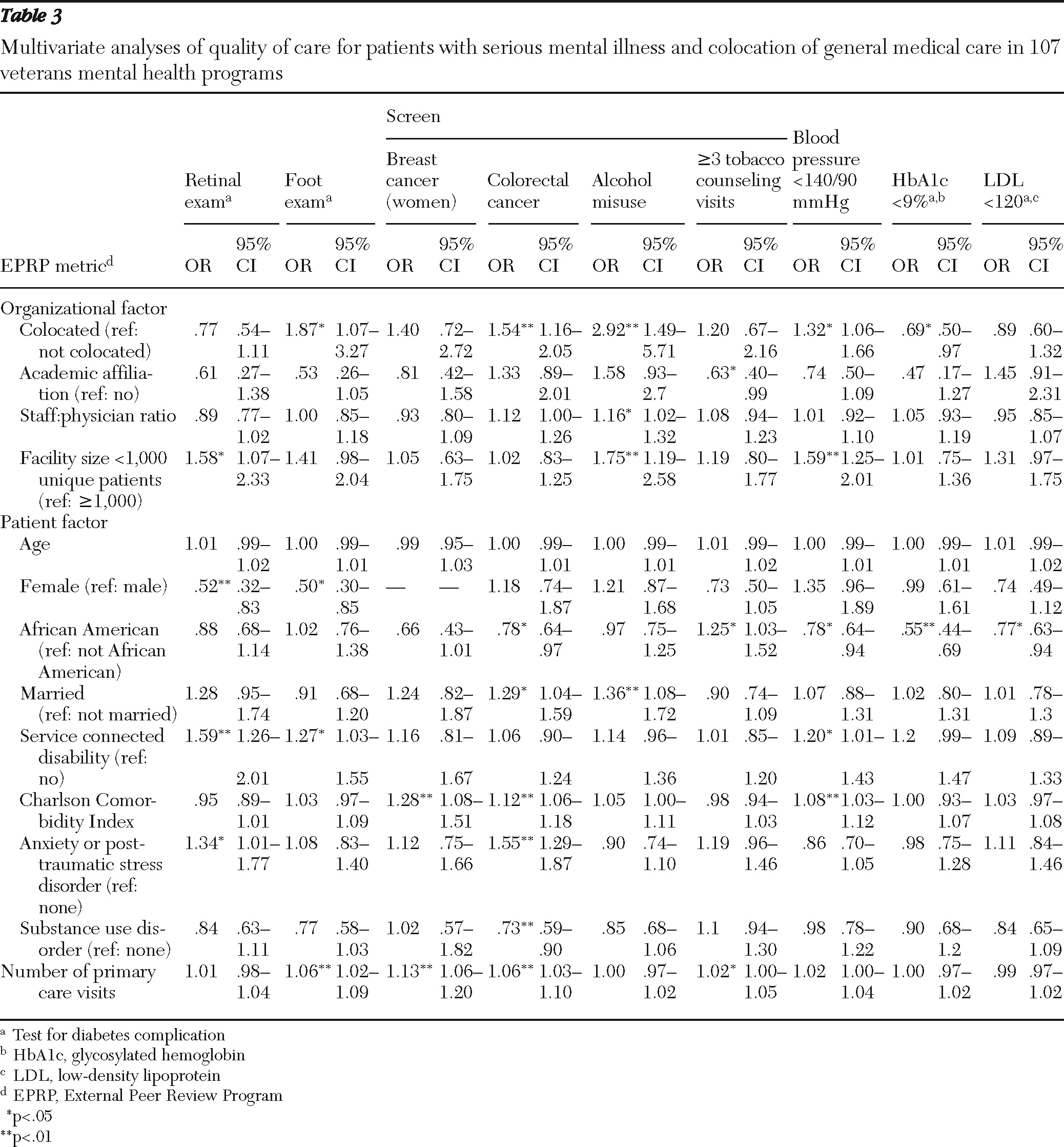
After adjustment for other organizational factors, patient demographic characteristics, and clinical severity, the analyses showed that patients with serious mental illness and receiving care from colocated clinics were more likely to receive diabetes-related foot exams (odds ratio [OR]=1.87, p<.05), colorectal cancer screenings (OR=1.54, p<.01), and alcohol misuse screenings (OR=2.92, p<.01) than patients from clinics without colocated services (
Table 3). Patients with serious mental illness and receiving care from colocated clinics were more likely to have good blood pressure control (OR=1.32, p<.05) but less likely to have HbA1C <9% (OR=.69, p<.05).
Discussion
Colocation of primary care services in mental health clinics was associated with improved quality of care, notably for key processes of care (foot exams for diabetes complications, colorectal cancer screening, and screening for alcohol misuse) as well as clinical outcomes related to blood pressure control. Observed rates of quality of care in this sample exceeded national averages, where in one report only half of patients received recommended processes of care for chronic conditions (
23).
This is one of the first national studies assessing the direct impact of integrated medical care on quality of care among persons with serious mental illness. These findings suggest that colocation of services is associated with improved quality of care, particularly for processes of care for common general medical problems among patients with serious mental illness. Despite the increased attention given to integrated mental health treatment in medical care settings, few studies exist on the availability of integrated medical care models in mental health settings and their subsequent impact on quality or outcomes of care for persons with serious mental illness, who primarily use mental health specialty settings as their medical home (
24). In a recent study of availability of medical care among community mental health centers, Druss and colleagues (
25) found that among 181 community mental health centers, only half were able to provide medical care for cardiometabolic conditions. Unlike the VA, community mental health centers face a number of barriers to integrated medical care, including separate payment and insurance structures, provider networks, and limited availability of primary care providers (
26).
In general, the VA, with its single-provider network, is able to provide seamless transition between general medical and mental health services. The VA Office of Mental Health Services and Mental Health Quality Enhancement Research Initiative consider improvement of medical care for veterans with serious mental illness a priority as stated in the Uniform Mental Health Services Handbook. As one of the largest single providers of mental health services in the nation, the VA has invested in a number of comprehensive programs for persons with serious mental illness, including psychosocial rehabilitation and recovery and intensive case management, over the past several years, but to date a medical home model for veterans with serious mental illness has not been articulated. Although only ten VA mental health programs in this sample had a colocated general medical clinic, all VA patients are assigned a primary care provider. Still, findings suggest the potential added benefit of colocated medical services in terms of improved quality of care.
Our findings suggest that colocation was associated with improved processes of care, notably for diabetes (foot exams), colorectal cancer, and alcohol use screenings, and improved outcomes for hypertension control among patients with serious mental illness. Although these types of services may seem disparate, they represent services in the VA that chiefly require a handoff to another provider. It is likely that because of proximity, the general medical clinic within the mental health program facilitated these handoffs. However, colocation was not associated with better outcomes (HbA1C levels) among those with diabetes, even after we controlled for organizational and clinical severity factors. This finding suggests that colocated care may not be beneficial to patients with co-occurring chronic medical conditions such as diabetes and that additional support for these conditions might be warranted. At the same time, this finding might be attributed to potential ascertainment bias, given the increased awareness of potential cardiometabolic risk factors from second-generation antipsychotics, and may lead to more cases of diabetes as a result of increased HbA1C monitoring.
Despite the use of comprehensive, national data on organization and quality of care, the findings from this study need to be interpreted with caution. First, misclassification bias arising from key informant responses is an important limitation when measuring health system features based on any survey, because the responses may or may not represent actions made by all providers at the particular site. The EPRP sample may have missed some patients with serious mental illness, because EPRP's sampling frame did not include patients who received care only from VA clinics for homeless veterans, mental health-related vocational assistance, mental health incentive therapy, or compensated work or vocational group visits resulting from mental health services. The Mental Health Program Survey was conducted in early 2007, and since then the VA has initiated several programs related to integrated medical care for persons with mental disorders, including the VA's Patient Aligned Care Team (the medical home) initiative and the Mental Illness Research, Education and Clinical Center Initiative on Antipsychotic Management Improvement. Hence it is difficult to draw inferences about the current quality of VA care from these data. Data for additional outcomes, including hospitalizations, disease incidence, or mortality, were not readily available. Finally, findings from this study may not generalize to non-VA providers or patients because the study sample was mostly male.
Conclusions
Overall, colocation of medical care in VA mental health clinics was associated with improved quality of care among patients with serious mental illness for four out of nine indicators (diabetes, colorectal cancer screening, and alcohol misuse screenings and hypertension control). These findings suggest that in a naturalistic setting, colocation of general medical services within mental health programs is associated with improved quality of medical care, particularly processes of care for a variety of conditions.
However, colocation had an inverse association with diabetes control, suggesting that additional strategies are warranted for chronic medical illnesses. The chronic care model, which includes systematic care management, self-management education, and guideline implementation, has been shown to improve diabetes and other medical outcomes among persons with mental disorders (
27,
28). Central to this model is a care manager (usually a nurse) who coordinates services across different providers regardless of their relative location. Of course, colocation may not automatically lead to greater coordination of services and because not all sites have colocated medical providers, additional efforts are warranted to develop a chronic care model to promote outcomes self-management in conjunction with medical care processes. Notably, the VA's recent mandate for integrating mental health care into primary care programs includes both colocation of mental health professionals as well as chronic care model-based care management (
29). Future research should focus on whether systems-redesign models such as the chronic care model can improve medical outcomes if offered in tandem with colocated general medical services for veterans with serious mental illness. Through these investments in state-of-the-art integrated care programs, the VA is ultimately well positioned to influence the next generation of medical home models for persons with serious mental illness.
Acknowledgments and disclosures
This work was supported by grant 07-115 from the VA Health Services Research and Development Service and by grant R34 MH74509 from the National Institute of Mental Health. The authors acknowledge the VA Office of Quality and Performance for providing access to the VA EPRP data. The views expressed in this article are those of the authors and do not necessarily represent the views of the VA.
The authors report no competing interests.