Over the past 50 years the importance of a supported transition from hospital-based to community-based mental health care, with an integrated network of outpatient, daytime, residential, and hospital facilities, has gradually become an established principle in international mental health social and health care policies (
1). Scientific and economic interests in the issue of what constitutes the ideal “balance of care” (the optimal hospital-based and community-based system equilibrium) have also grown rapidly (
2).
Although the Italian National Reform Law of 1978 enforced the closure of psychiatric hospitals and set out general principles and guidelines for the integration of persons with severe mental illness into the community, it was only in the 1990s that two National Mental Health Plans (
3) in Italy defined the organizational model and provided some quantitative standards (
4). During the past decade, the planning of health care in general (including mental health care) was assigned to the regional authorities, who were asked to promulgate their own regional mental health plans.
Mental health care in Italy is delivered by mental health departments that are in charge of the management and planning of all medical and social activities related to prevention, treatment, and rehabilitation in a defined catchment area. Within the departments, community mental health centers (CMHCs) cover all activities pertaining to adult psychiatry in outpatient settings and manage therapeutic and rehabilitation activities delivered by day-care services and nonhospital residential facilities. [A diagram showing the CMHC processes of care is available as an online supplement to this report at
ps.psychiatryonline.org.]
In Italy and other European countries, at both the local and national levels, the process of deinstitutionalization and implementation of a community-based model was characterized by a lack of evaluation mostly resulting from insufficient attention to the development of systematic data collection (
5,
6). There has been no deliberative action to develop or maintain standards of quality of care. To fill this gap, two Italian national surveys were carried out in 2002 and 2003 to provide a descriptive overview of the characteristics of inpatient and residential facilities (
7,
8) and of patients admitted to and discharged from these facilities over an index period (
9,
10). A third national survey, named PROG-CSM (Progetto Centri di Salute Mentale), was subsequently undertaken in all Italian CMHCs in 2005 with the aim to examine the extent to which these facilities adhered to the standards defined by the National Mental Health Plan.
Methods
To develop an instrument to assess adherence to the standards of the National Mental Health Plan, a large research group including mental health professionals, biostatisticians, and epidemiologists translated the plan's policy recommendations into operational definitions of the key domains of interest; the group then generated questions to explore these domains. This process was carried out in small-group and plenary work sessions and consisted of analyzing existing instruments and defining specific indicators.
Consensus was reached on the following domains: continuity of care, coordination with other community-based services, accessibility, implementation of specific programs, and provision of care. Continuity of care refers to the level of integration of the CMHC with the other services in the mental health departments, which include day centers, day hospitals, residential facilities, and inpatient facilities. It is defined as the ability to cooperate with other services and take a long-term perspective in offering an integrated sequence of crisis management interventions and support in settling discharged patients in the community. These interventions include developing procedures for admission and discharge to mental health department facilities as well as monitoring and follow-up procedures after patient discharge. Coordination with other community-based services refers to the ability of each CMHC to create and maintain a network with other community-based services (outside the mental health department) to coordinate long-term interventions for problems such as housing, employment, general medical illness, and poor social networks. Accessibility denotes the capacity of the CMHC to ensure that needs of the population are managed rapidly and adequately. Characteristics that could facilitate or hamper access to services (opening hours, procedures for immigrants, and local and decentralized branch services of the CMHC) are explored. Specific programs denote the capacity of the CMHC to implement care or prevention programs to meet specific population needs (stigma prevention, training of general practitioners, and self-help). The provision of care includes the number of patients seen and treated. [An appendix summarizing the operational definitions and coding of the domain indicators is available as an online supplement to this brief report at
ps.psychiatryonline.org.]
Several questions were then generated to explore these domains, and two questionnaires were developed, one for the CMHC and the other for the mental health department. A pilot study was carried out in 22 CMHCs and 22 mental health departments (one per region) to test the face validity of the questionnaires and the procedures for data collection. From the feedback received during the pilot study, some items were rephrased, and other specific programs were added to the list.
The survey was conducted between July 2005 and December 2006 by two researchers per region, who were recruited from an existing network of experienced interviewers that had been established for two previous Italian national surveys. Researchers completed a day of training in use of the instruments and the procedures of data collection. Their task consisted of rating the questionnaire items and retrieving data from the mental health information systems when available. Data from local information systems were used to estimate the prevalence and incidence of psychiatric disorders.
Results
The PROG-CSM survey was carried out in 707 Italian CMHCs and 211 mental health departments. All the Italian regions participated in the survey except Molise, which did not participate because its community services were only partially set up. Forty-three CHMCs were unable to provide any usable information, and 28 provided partial information for a variety of reasons, including the lack of a local information system. In total, 636 CMHCs provided usable data to define the indicators.
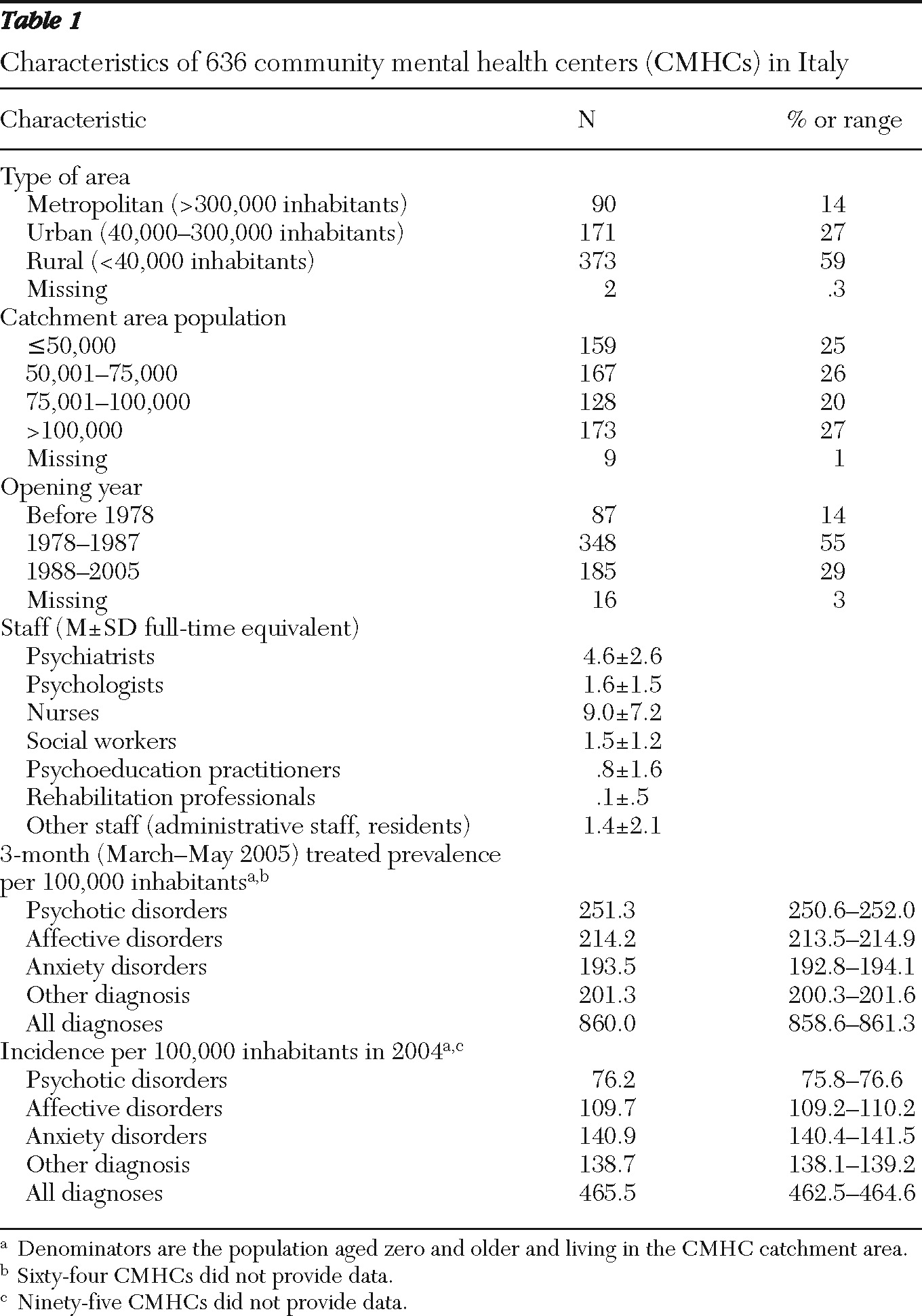
The 636 CMHCs were from 195 of 211 mental health departments, one half of which included services for childhood and adolescence and for drug addiction. They covered the full Italian territory, with about 60% located in small towns or rural areas (
Table 1). About 50% opened in the decade after promulgation of the National Reform Law of 1978, and 30% in the subsequent decade. On average, the full-time-equivalent staff (38-hour week for psychiatrists and 36-hour week for other staff) included five psychiatrists, nine nurses, two psychologists, 1.5 social worker, seven psychoeducation practitioners and less than one rehabilitation professional and psychoeducation professional (
Table 1). The overall three-month treated prevalence was 860 cases per 100,000 inhabitants, and the overall one-year incidence was 466 cases per 100,000 inhabitants (
Table 1). The diagnostic distribution indicates that psychotic disorders accounted for more than one-third of the diagnoses of patients seen in the index period and about one-sixth of the diagnoses of new patients.
The frequency distribution of the indicators revealed a high adherence to the standards of the National Mental Health Plan in terms of continuity of care and coordination with other services. One-third of the CHMCs achieved the highest scores on these indicators. On average, lower levels of accessibility and implementation of specific projects were found. [A figure showing the frequency distributions of the indicators is available as an online supplement to this report at
ps.psychiatryonline.org.]
The four indicators were unrelated to the number of years of activity of the CMHCs, with Spearman's rho correlation coefficients ranging from –.014 to .122.
Discussion
CMHCs were sufficiently developed throughout Italy, and continuity of care and service coordination levels, which are crucial for managing patients with severe mental illness, were satisfactory. The degree of organizational development in Italy was directly proportional to the moment that the process of mental health department articulation actually began in a given area and to the amount of economical resources invested before 2000, when health policies began to take hold that were more oriented toward considerably limiting health care costs (though poorly regulated, to date). However, our results indicate that adherence to the standards was unrelated to the duration of a CMHC's operations.
Many national caregivers' and professionals' associations have demanded that Italy establish a minimum threshold for funding psychiatric care in its national budget (5% of the local health care budget), in line with the average health care budget (5.9%) in European countries (
11). However, this demand has not received the support required to be transformed into a local health care administrator constraint.
The political mental health debate in Italy tends to disregard the importance of evaluating the data available and to focus on modifying appropriateness standards (
12). The availability of assessment instruments can allow, in the near future, a comparison of different national community care models with regard to shared standards, such as those established by a recent green paper (
13). We submit that indicators such as continuity of care, coordination with other community services, and accessibility can be helpful in measuring the equity and appropriateness levels achieved by any public health system (
14).
Several limitations of this study should be acknowledged. The first is the cross-sectional nature of the study and measures of adherence. Second, it is possible that the information collected was biased by social desirability or concerns about feedback to local or national authorities, and no secondary data or sources were used to help interpret or cross-check the data collected. To minimize this bias, we chose to use independent evaluators instead of local staff for the survey, and we phrased items whenever possible as yes-no questions to avoid arbitrary judgment.
Third, prevalence and incidence estimates were based on data provided by the CMHCs with an information system in place. Although it is possible that CMHCs without an information system had a caseload different from those with an information system, this assumption seems unlikely. Moreover, our estimates reflected only the incidence and prevalence treated in the CMHCs. Approximately 50% of mental health disorders, especially mood and anxiety disorders, were managed by primary care physicians and private mental health professionals, and some of the patients were treated in long-term residential facilities or drug addiction services.
In a study carried out in the Lombardy region and based on regional information system data for 2009, incidence and prevalence rates for psychotic disorders (
ICD-10 codes F20–F29) treated in community mental health services were 2.2 per 10,000 and 37.9 per 10,000 adults (
15). Another Italian study using 2007 data from three regional information systems (Friuli Venezia Giulia, Lombardy, and Emilia Romagna) reported a global treated prevalence in these three regions of 33 per 10,000 population aged 14 years or older (
15). In the present study, we used the entire population (aged 0 and up) as the denominator for the calculation of incidence and prevalence, which lowered our rates compared with others (
15) and hindered comparisons.
Conclusions
Our results indicate that CMHCs were sufficiently developed throughout Italy, and continuity of care and service coordination levels were satisfactory. However, adherence to the standards was unrelated to the duration of activity of the CMHCs.
Acknowledgments and disclosures
The PROG-CSM survey was funded by the Italian Ministry of Health.
The authors report no competing interests.