Over the past 15 years, reports of peer support services for adults with serious mental illness have increased dramatically. These peer-oriented efforts have been viewed as a response to the 2003 President’s New Freedom Commission on Mental Health (
1), which called for the transformation of mental health services to a recovery orientation. Peer-oriented efforts have been embraced as a promising new resource for people facing the challenge of living with a serious mental illness.
The evidence supporting the effectiveness of peer-provided services, however, has lagged this rapid proliferation. Reviews conducted over the past 15 years revealed that people with histories of mental illness, or “peers,” could provide conventional mental health services, such as case management, that were comparable in effectiveness to those provided by nonpeers, but they found little evidence of the superiority of peer-provided services on a wide range of outcomes (
2,
3).
Recent studies have focused on the use of peer support, a new kind of service in which peers aim to engage, coach, or mentor people who have not benefited from conventional care (
4–
10). Thus far these studies suggest that peer staff might be better able than nonpeers to develop trusting relationships with this so-called “difficult-to-engage” population (
7). Some reviews found moderate evidence that peer support leads to higher levels of empowerment, hopefulness for recovery, engagement with care, and patient activation, resulting in reductions in use of inpatient services and improved relationships with providers (
11,
12). Others purported not to find any differences in outcome between those who were or were not offered peer support (
13,
14).
Fully 40% to 60% of hospitalized psychiatric patients are expected to return to the hospital within a year of discharge. For these “revolving door” patients, peer mentors may offer a particularly effective connection that may help break the cycle of repeated hospitalization (
15). Despite the suffering and expense associated with recurrent hospitalization, the factors contributing to the pattern are poorly understood, although they are known to range widely from individual- to system-level factors (
16,
17). Not surprisingly, one of the best predictors of recurrent hospitalization is prior hospitalization (
15). Previous research suggests that peers may be able to offer effective support to individuals who are rehospitalized because they did not respond to traditional care after discharge. In our initial report of a randomized trial to evaluate this possibility (
18), we demonstrated that compared with standard care, peer mentorship was associated with reduced rehospitalization among a group of patients with a history of repeated overuse of acute services.
This study is the third of three reports exploring dimensions of the effectiveness and experience of peer support for persons with multiple hospitalizations (
18,
19). In this installment, we explore the relationship between a peer mentor intervention and improved clinical outcomes and increased community tenure among a sample of individuals with serious mental illness and a history of multiple hospitalizations (
18).
Methods
This study was a randomized, controlled trial approved by the Yale School of Medicine Institutional Review Board. Details of the design, including a description of the intervention, recruitment and randomization procedures, clinical outcome measures, and results of rehospitalization, are reported elsewhere (
18). Briefly, potential participants were identified and recruited during an “index” inpatient stay at the Yale–New Haven Psychiatric Hospital, a 74-bed psychiatric hospital located in an academic medical center serving south central Connecticut. The index hospitalization was defined as the third or more admission to the psychiatric inpatient unit within an 18-month period or the second admission after three or more psychiatric emergency department visits within an 18-month period. After completing consent procedures, participants were randomly assigned to the standard care condition or the recovery mentor (RM) plus standard care condition (hereafter called the “RM condition”). Each consent packet—labeled 1 or 2 for standard care or the RM condition, respectively—was assigned, a priori, on the basis of a sequence generated by a random number generator.
The Experimental Intervention
RMs were individuals who self-identified as being in recovery from serious mental illness and who were open to sharing their experiences to assist others in the recovery process (
18,
19). Over the course of the study, eight RMs, who competed via formal job postings, were hired and trained to provide community-based support to individuals in this study following the individuals’ discharge from an index hospitalization.
The RM training sessions were conducted by the Program for Recovery and Community Health faculty and focused on the core functions of the “recovery guide” model, developed by Davidson and colleagues (
20,
21). This rigorous training includes instruction in fundamentals of recovery philosophy and recovery promotion, local resources, professional and personal boundary considerations and safety, cultural competence, and gender- and trauma-informed care, with a core emphasis on identifying assets and strengths of the mentees and on providing support in an individualized manner that enables participants to pursue personal goals.
Study supervisors provided ongoing supervision of the RMs through various interactions, but the core component was a 90-minute team meeting each week. The meetings were designed to promote team cohesion and provide a venue to solve problems, identify strategies to develop and enhance relationships with participants, exchange information about resources, discuss concerns, and share successes and failures in a supportive atmosphere.
RMs worked independently of the mental health system and communicated with treatment providers only by the request of the participant. RMs were urged to use their own experiences as the basis from which to provide support to participants and were assigned by project staff to a participant on the basis of that person’s expressed preferences (for example, someone of the same gender or similar psychiatric or personal history). RMs were introduced to the participants they would mentor within a week of study entry and offered services for up to nine months after the participants’ discharge from the index hospitalization. There was no predetermined frequency of contact. However, they were encouraged to meet with a mentee for a minimum of an hour each week, either in person or by telephone. The details of the contact were determined by collaboration between mentor and mentee and varied considerably.
The clinical care received by participants after their discharge consisted primarily of community-based care, which was provided separate and independent of the RMs. Generally, clinical services were publicly supported; however, some participants used fee-for-service insurance benefits. In both private and publicly supported settings, the care consisted of medication management services (evaluation, prescription, and monitoring), psychoeducation, case management, and forms of supportive psychotherapy. Participants had the same opportunities for outpatient services regardless of whether they were randomly assigned to standard care or the RM condition.
Participants
Eligible patients were approached by study personnel during the early part of the index hospitalization after a review of their medical records and an administrative database . To be eligible, patients must have been at least 18 years old; must have experienced three or more psychiatric hospitalizations (or two admissions plus more than three psychiatric ED visits) during the 18-month period prior to the index hospitalization; must have a documented
DSM-IV (
22) diagnosis of schizophrenia, schizoaffective disorder, psychotic disorder not otherwise specified, bipolar disorder (type I, type II, or not otherwise specified), or major depressive disorder with or without psychotic features; and must have been willing to accept random assignment to standard care or the RM condition. Exclusion criteria were an inability to give signed, written consent; non-English speaker; and a primary
DSM-IV axis I diagnosis of substance abuse or dependence or an axis II diagnosis alone.
Population and Recruitment
Of the 4,371 individuals admitted to the adult wards of the Yale New Haven Psychiatric Hospital between November 1, 2006, and November 1, 2008, only 307 met the stringent eligibility criteria of this study. Of these 307 eligible individuals, 93 (30%) consented to enrollment and were randomly assigned to the RM condition (N=48, 52%) or standard care (N=45, 48%). Of the 93 enrolled participants, 15 withdrew from the study and two died after enrollment. For these analyses, the intent-to-treat sample (N=76) comprised all living individuals who did not withdraw consent during the study (N=39, RM; N=37, standard care). Because of significant attrition along the course of the study and because nearly 44% of those assigned to the RM condition did not engage in the treatment, we also present the findings from an analysis of 51 individuals who were considered treated. Participants in this analysis had completed at least a baseline interview and, for the RM condition, had at least one contact with the assigned mentor or clinician (N=22, RM; N=29, standard care). [A CONSORT chart of participation in the study groups is available as on online supplement.]
Evaluation
Participants were assessed immediately after discharge from their index hospitalization and at three and nine months postdischarge by study staff who were not involved in the intervention and who were not informed of the randomization status of the participants. Basic demographic information, diagnoses, and hospitalization data were obtained from administrative records. The baseline and follow-up interviews conducted by study staff contained a more detailed assessment of demographic information, along with measures of the following domains: alcohol and drug use (alcohol and drug use subscales of the Addiction Severity Index [ASI] [
23,
24]), psychiatric symptoms (Brief Psychiatric Rating Scale [BPRS] [
25,
26]), functional health and well-being (36-Item Short-Form Health Survey 1.0 [SF-36] [
24,
27,
28]), patient attitudes about their condition and future (Hope Scale [
29]), satisfaction with treatment (Mental Health Statistics Improvement Program [
30]), social functioning (modified Social Functioning Scale [
31]), and sense of community (Sense of Community Index [
32]).
Analysis
Between-group differences in demographic characteristics were examined via one-way analyses of variance and chi-square analyses by using SPSS, version 21 (
33). A series of regression equations with a linear mixed model (LMM) were conducted for each outcome variable, with the baseline value of the dependent variable included as a covariate in each model, along with baseline demographic variables that significantly differentiated the two groups. In addition to examining composite and subscale scores on each of the outcome measures, we conducted exploratory item-level analyses of items within the ASI and BPRS to identify any specific associations with the intervention. Main effects for treatment condition and time were included in the model, and a condition × time interaction term was added in separate models. Given the exploratory nature of our analyses, the relatively large number of tests required to examine item-level associations, and the lack of specific, prespecified hypotheses, we followed the recommendations of Bender and Lange (
34), who advise against adjusting p values for multiple comparisons. Thus any significant findings at p<.05 were viewed as exploratory, not confirmatory, results.
Life tables were used to provide estimates of median survival time (time between discharge and rehospitalization or end of study) and rates of survival (time to readmission) at 30, 90, 180, and 270 days after discharge from the index hospitalization. Cox regression was used to examine the degree to which assignment to the RM condition predicted length of community tenure between discharge from the index hospitalization and readmission (survival), above and beyond pre-enrollment hospitalization rates and days.
Results
Demographic Characteristics
Participants were, on average, 40 years old and were equally divided by gender. The sample was mainly white (N=45, 59%) and black (N=20, 26%) and was largely non-Hispanic (N=60, 79%). Seventy-five percent of the sample was diagnosed as having a psychotic disorder (N=57) and 25% (N=19) as having a mood disorder. There were no between-group differences at baseline in demographic characteristics of the intent-to-treat sample; however, RM participants in the treated sample reported significantly higher levels of education compared with those in standard care.
Table 1 presents complete demographic characteristics at baseline of the intent-to-treat sample.
The 22 RM participants who met with their mentor at least once had 13.0±11.3 visits on average (range 1–61 visits), spending an average of 24.9±18.8 total hours with the RM (range 2–61 hours). An examination of the baseline characteristics that distinguished participants who met with their RM versus those who did not revealed several significant differences. Compared with participants who did not meet with their mentor at all (N=12), individuals who met with their mentor at least once were more likely to be white (χ2=4.58, df=1, p=.03), less likely to be living in a private residence (χ2=5.77, df=1, p=.02), completed more years of formal education (F=7.28, df=1 and 28, p=.01), and reported fewer general medical problems (F=6.10, df=1 and 27, p=.02), less alcohol use (F=4.08, df=1 and 29, p=.05), fewer psychiatric symptoms (F=11.93, df=1 and 30, p=.002), greater satisfaction with services (F=9.34, df=1 and 30, p=.01), and a greater sense of community (F=5.44, df=1 and 30, p=.03).
Among individuals across both conditions who completed a baseline interview (N=63), those who did not have a follow-up interview (N=17, 27%) had fewer hospitalizations in the 18 months prior to baseline compared with those who had a follow-up interview (N=46, 73%) (3.24±.83 versus 4.09±1.41; F=5.45, df=1 and 61, p=.02). They also reported earning, on average, about $300 less in income per month (F=6.08, df=1 and 57, p=.017), were more likely to have children (χ2=6.14, df=1, p=.01), reported more alcohol use (F=8.85, df=1 and 55, p=.004) and more drug use (F=7.55, df=1 and 57, p=.008), and were less likely to have a sense that community members help each other with needs (F=4.04, df=1 and 50, p=.05).
Outcome Variables
In the intent-to-treat sample, after the analyses controlled for baseline values of the dependent variable, a significant main effect was found on the ASI alcohol subscale, with RM participants reporting significantly lower scores at nine months compared with standard care participants (
Table 2), indicating less severe problems in that domain. Interaction effects suggested that participants assigned to the mentor condition had a greater decrease in drug use (ASI-drug subscale, days of drug use, days with drug problems, and feeling troubled by drug problems) compared with standard care participants, who reported an increase in drug use from baseline to the nine-month follow-up. On the BPRS items, participants in the RM group demonstrated greater improvements over time in physical health, hygiene/self-care, unusual behavior, and excitement compared with those in standard care. There were no significant main effects or interactions observed between the groups in functional health, hope, service satisfaction, or sense of community.
Similar to results for the intent-to-treat sample, the analysis of treated participants, also included in
Table 2, revealed that participants who met with their RM at least once had significant improvements over time on BPRS items related to physical health and hygiene/self-care, compared with participants receiving standard care alone. Like those in the intent-to-treat sample, RM participants in the treated sample also showed significantly greater improvement than the standard care participants on the ASI item about feeling troubled by drug problems. RM participants who met with their RM also demonstrated significantly greater improvements in social functioning over time than participants in the standard care condition. There were no significant differences between the RM and standard care groups for the ASI-alcohol subscale, ASI-drug subscale, other ASI or BPRS items, or measures of functional health, hope, service satisfaction, or sense of community.
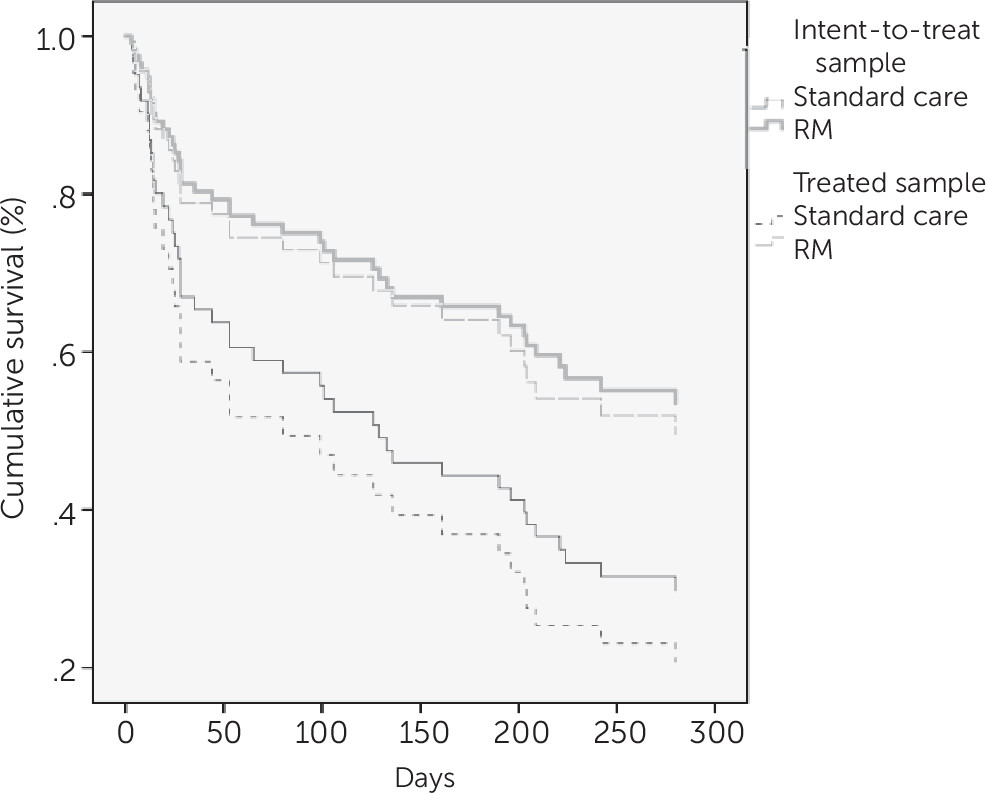
The survival analysis demonstrated that individuals in the RM condition had a median length of time to rehospitalization of 270 days, compared with 135 days for individuals in standard care (
Table 3 and
Figure 1). Within the first 30 days of discharge from the index hospitalization, only 15% of participants who were randomly assigned to RM experienced a psychiatric hospital readmission, compared with 38% of those who were randomly assigned to standard care. Ninety days after the index hospitalization discharge, 26% of those assigned to the RM condition had experienced a psychiatric hospital readmission, compared with 43% of standard care participants. By the nine-month follow-up, 48% of individuals assigned to the RM condition had experienced a psychiatric hospital readmission, compared with 66% of the standard care participants.
When controlling for pre-enrollment admissions and hospitalization days, the survival analysis showed that assignment to the RM condition significantly predicted the likelihood of remaining out of the hospital for a longer period (χ
2=4.59, p=.03) (
Figure 1). The survival rates at each follow-up and the timing of first readmission were similar for the treated analytic sample (χ
2=4.94, p=.03).
Discussion
This study provides evidence in support of theories and emerging research that peers may play uniquely beneficial roles in connecting with individuals who may be difficult to engage or less responsive to traditional outpatient care. Using both intent-to-treat and treated samples, we observed significant improvements in drug use, symptoms, and community tenure for individuals who were randomly assigned to an RM condition compared with those in standard care. Of greatest clinical and statistical significance is the dramatic reduction in rates of hospitalization in the months following the index hospitalization among the participants in the RM condition compared with participants in standard care (
Table 3 and
Figure 1). Standard care participants were readmitted to the hospital at nearly three times the rate of RM participants at three months, and RM participants remained out of the hospital nearly twice as long as standard care participants (median days to hospitalization=270 and 135, respectively). These findings, in conjunction with the self-reported improvements in functioning, health, and drug problems, although exploratory in nature, suggest that by promoting interactions with a peer during the critical posthospital period, the RM program is a promising intervention and worthy of further exploration through additional confirmatory studies.
We must, however, consider the condition of those who did not connect with their assigned mentor or who were not available for follow-up interviews. There may have been prerecruitment traits among these two groups (not detected in this research) affecting willingness or ability to participate in the RM opportunity. Our evidence suggests that individuals who were available for follow-up after the baseline assessment averaged more hospitalizations in the 18 months prior to baseline, had more income, had less alcohol and drug use, and reported a greater sense of community at baseline compared with those lost to follow-up. Moreover, of those assigned to the RM condition, participants who met with their mentor were more likely to be white and living in a nonprivate residence, were more educated, and felt a greater sense of membership in their communities. They also appeared to be less symptomatic and had fewer problems with alcohol than participants who did not meet with their mentor.
Because 50% of those who did not participate in the intervention also did not have a follow-up interview, we do not know if the reasons for nonengagement had anything to do with the intervention, the symptomatic and social profiles of the individuals, or both. Those who did not participate may be a unique subgroup of recurrently admitted patients that for one reason or another does not connect with available resources and that may require a more assertive, specialized engagement approach. Our clinical experience suggests that this is so.
It is important to acknowledge the technical limitations of this study that may preclude generalization to other settings. In addition to being limited to only one setting, the study had a small number of participants (N=93), and those who participated represent a small proportion of eligible participants (N=307). These factors opened the results to idiosyncratic influences and dramatic changes in direction, whether because of the passage of time or the influence of other unrecognized processes. Adults with severe mental illness who experience multiple psychiatric hospitalizations within an 18-month period make up a small proportion of individuals admitted to psychiatric inpatient units, yet they may be among the most costly and difficult to treat. In this study, only roughly 7% of patients admitted to the adult wards of a psychiatric hospital over a two-year period met our criteria for recurrent psychiatric hospitalization. Given that 58% of the eligible patients admitted to the inpatient unit were discharged before we had the chance to approach them about the study and given the high level of interest in participation among those approached (75% of those approached chose to enroll in the study), there is a critical need to determine ways to connect with these high-risk patients earlier in the hospitalization process, perhaps even upon admission.
Second, our study offers no quantitative information about the operant feature of the program’s apparent effectiveness. Persons with serious mental illness may benefit simply from spending more time with an interested person. On the other hand, spending time with mentors with lived experience of recovery may provide specific rewards that are superior in effectiveness to the benefits of other relationships. Our qualitative study (
19) suggests that RMs may bring specific factors to their interactions with their mentees that may be considered as falling under the construct of accurate empathy and engagement. These factors would allow them to share a unique understanding of the challenges facing their clients and demonstrate a special sensitivity to the dilemmas of those who are re-experiencing difficulties, worsened by loneliness and low self-esteem. In addition, RMs may be particularly able to communicate this empathy. Future research that can standardize and assess the degree to which peer staff demonstrate these aspects of care in their relationships will be able to shed additional light on these issues.
Finally, we must emphasize that the results should be viewed as exploratory in nature, given that corrections were not made to account for the increased familywise error rates (probability of making at least one type 1 error) associated with conducting multiple tests. Correcting for familywise error rates in such exploratory analyses is often difficult or impossible because the number of tests is typically large and there are no clear, prespecified hypotheses (
33). Thus as we interpret these findings cautiously, we also believe they point to potential areas for further exploration in confirmatory studies.
Conclusions
The suggestive findings from this randomized but small-scale study warrant further testing with larger and more representative samples. To the degree that they are useful, though, they suggest that peer support services that build explicitly and directly on a peer’s lived experiences of mental illness and recovery may offer more than simply adjunctive, nonspecific support. In fact, these services may be a particularly effective, highly specific means of engaging reluctant persons in distress in supportive relationships that serve to decrease substance use and increase community tenure.