The current U.S. health care landscape demands high cost-effectiveness without compromising standards of patient care. Behavioral health (BH) disorders co-occurring with general medical problems are well known to contribute to high health care cost and poor outcomes (
1). Multiple studies of collaborative integrated BH care approaches demonstrate improved economic and health care outcomes (
1). Patients requiring constant observation (CO) in general hospitals present economic burden for staffing needs (
2). However, studies fail to show a reduction in adverse events despite use of CO (
3,
4). With high prevalence of psychiatric comorbidity and the frequent use of CO of elderly medical-surgical patients with dementia and delirium, proactive engagement of BH specialists in quality improvement (QI) partnership with medical-surgical staff may offer general hospitals important improvement opportunity.
Project Evolution
With limited staffing resources, our newly formed psychiatry department was presented with the challenge of raising staff awareness of the BH needs of patients served by our 591-bed general hospital in the New York City metropolitan area. Even though our hospital does not have a designated psychiatric unit, 34% of all admitted medical-surgical patients have a psychiatric diagnosis listed in their medical records, which correlates with the national data (
5). However, only 1.36% of those patients had requests for psychiatric consultation by attending physicians. In seeking effective ways to gain acceptance by staff and administration, we found that our hospital spent $2.3 million on CO in year 2014 alone. Thus, from a QI perspective, patients under CO represented a “high cost, high volume, poor outcome” population. Because our hospital strives to be restraint free, reducing use of CO without increasing use of restraints was a legitimate challenge. Recognizing an improvement opportunity, we sought to offer psychiatric expertise in the behavioral and pharmacologic management of common CO scenarios. We therefore proposed a QI project aimed at reduction of CO utilization, with the goal of improving outcomes while reducing costs. Several meetings took place with hospital leadership and nursing administration to present facts about CO scenarios and potential benefits of proactive BH team involvement. The proposal was met with enthusiasm by nursing leadership, which was instrumental in initiating the QI intervention by developing a hospitalwide policy requiring psychiatric assessment within 24 regular business hours for all patients placed on CO. To assess the efficacy of the project, we involved hospital QI department and nursing leadership to partner in collecting baseline and ongoing data.
The next step was to use QI methodology to develop, test, and continually improve intervention strategies. Initial case reviews provided information about potential behavioral management and medication interventions that might mitigate the need for CO while improving overall outcomes. Although our primary objective was CO reduction, we wanted to test the hypothesis that early and proactive involvement of the BH team would result in other measurable improvements in quality.
Protocol Overview
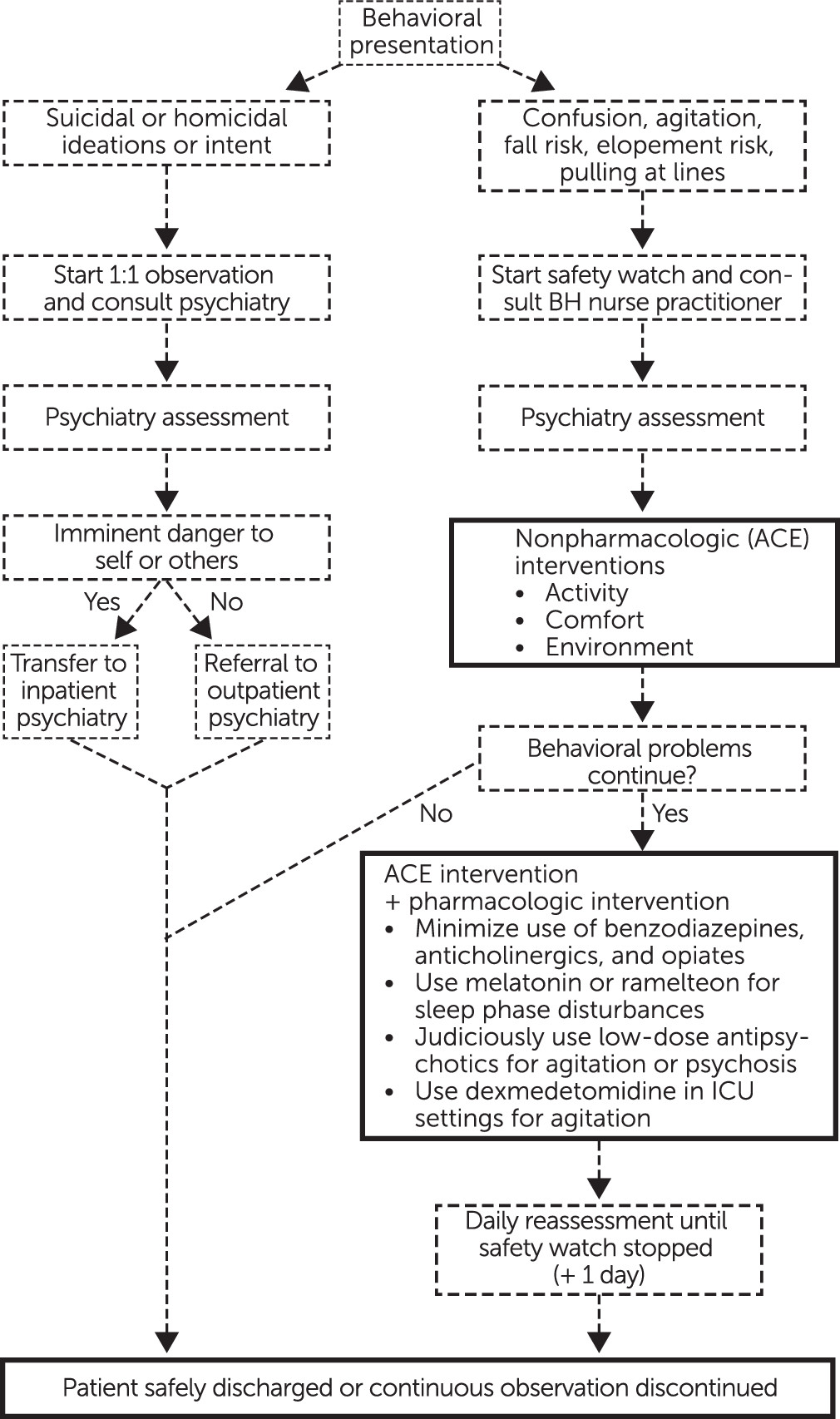
For this project, based on our clinical expertise and current standards of care, we developed a comprehensive evaluation and management algorithm (
Figure 1). Depending on the reason for CO, the attending physician orders one-to-one observation (1:1) or safety watch. In 1:1, one staff member directly observes the patient within arm’s length at all times. In safety watch, one staff member observes up to four patients in the same room. Typical CO scenarios include patients with suicidal ideation, altered cognition, or impaired judgment. Some 1:1 indications include risk of suicide or violence, whereas safety watch is used for agitated and cognitively impaired patients who may be pulling lines or catheters or are at risk of elopement or falls.
CO patients are referred for evaluation by the BH project team, consisting of a designated psychiatric nurse practitioner working in collaboration with a board-certified psychiatrist. A comprehensive initial psychiatric assessment with particular focus on safety, cognitive assessment, medical comorbidity, and current medications is conducted by the psychiatric nurse practitioner. Using a semistructured diagnostic interview adapted from the criteria listed in DSM-5, the clinician diagnoses and outlines a detailed treatment plan for each CO patient. Whenever possible, the team contacts the patient’s family to gather collateral information and discuss recommendations.
One result of this process was that early identification of the small number of patients requiring acute inpatient psychiatric hospitalization led to expedited transfers, which contributed to decreased CO and length of stay. Most patients, however, required improved treatment management on the medical-surgical unit.
We developed a multimodal approach designed to prevent and reduce delirium in the cognitively impaired elderly population who were at high risk of needing CO. An acronym “ACE intervention” was developed to emphasize measures relating to patients’ activity, comfort, and environment. [See figure in the online supplement.] This intervention included education of hospital staff, patients, and caregivers on delirium recognition and prevention. Frequent reorientation and redirection (such as encouraging the use of a call bell for assistance) were routinely recommended. Early ambulation and physical therapy were encouraged. Environmental recommendations included family presence, use of family photos, and familiar music. Whenever possible, patients were moved closer to nursing stations to improve access to staff. Sleep hygiene was emphasized by moving patients to beds next to windows, promoting daytime activity, and minimizing light and noise at night. When appropriate, early removal of lines, external tubes, and Foley catheters was recommended. Adequate pain management while minimizing and avoiding deliriogenic analgesics was recommended. Dietary needs and fluid intake were addressed to ensure adequate hydration and nutrition.
Unless specifically indicated, we routinely discouraged or minimized the use of benzodiazepines, opiates, and anticholinergic medications for patients at risk of delirium. When the ACE intervention was not enough to reduce behavioral disturbance, we used low-dose antipsychotics judiciously and briefly. [See table in the online supplement.] Whenever necessary, the BH team served as liaison between the family and health care team to assist with efficient flow of care and appropriate discharge planning.
This protocol was implemented daily with all patients who had received at least 12 business hours of CO, except weekends and holidays, when the nurse practitioner was not available. On-call psychiatrist consultants were available for emergent consultations during those times. All patients were followed until at least one business day after CO was discontinued. Data on length of stay, CO cost, complications (falls, elopements, or inadvertent extubations), and 30-day readmissions were collected over a six-month QI study period to evaluate the impact of our protocol. During this period, 491 patients were seen by the BH team and underwent the protocol. Data were compared with aggregate data for all patients receiving CO during the previous year to measure improvement over baseline in the plan-do-study-act QI change cycle.
Results
This project had a significant positive economic impact on our institution; the average monthly costs of CO were reduced by 33%, with an associated 15% reduction in length of stay, from seven days to six days. Savings were over $750,000 per year.
There were two patient falls in the study period, versus 63 in the comparison period; zero inadvertent extubations in the study period, versus 10 in the comparison period; and one elopement during the study period, versus three in the comparison period. In the control period, 20 of 553 patients (4%) were readmitted within 30 days, versus 10 of 491 patients (2%) during the study period. Because the baseline data were aggregated (with no information about individual patients), we did not calculate statistical differences. Nonetheless, the findings were viewed positively by hospital administration and medical and nursing leadership.
The CO population had a high prevalence of delirium (N= 305, 62%) and dementia (N=259, 53%), so that in addition to the ACE protocol, the reduction of deliriogenic medications may partly explain the demonstrated positive impact. Benzodiazepines were reduced for 25% (32 of 130 patients) and discontinued for 53% (69 of 130 patients) on these medications. Prescribed opiates were reduced for 34% (39 of 116) and discontinued for 49% (57 of 116 patients on opiates), and anticholinergics were discontinued for 92% (11 of 12 patients prescribed). We also found through the QI process that if patients with delirium were treated nightly with ramelteon, they were less likely to need antipsychotics for agitation (60% [N=36 of 60] versus 86% [N=56 of 65]).
Improvement Opportunities
Because of limitations in our initial efforts, improvement opportunities remain. The protocol was not implemented over weekends and holidays, and additional benefits may have been lost. This project did not examine the effect of the protocol on patient and staff experience and satisfaction. Future QI efforts for this population may address these opportunities. Finally, having an inpatient psychiatric or a medical-psychiatric unit in the hospital might further improve the quality and flow of specialized care.
Conclusions
A formal QI project using early and proactive involvement of a designated BH team to manage care of patients requiring CO demonstrated a “return on investment” through significant improvement in hospital economics and quality of care. This project was supported by routine QI infrastructure and consistent education and communication with leadership, staff, patients, and families. Success of this QI project required institutional buy-in and close collaboration with the nursing department and hospital administration. This collaboration, along with the measurable impact on cost and quality metrics, helped facilitate the acceptance, growth, and successful integration of our recently formed BH team with the rest of the hospital community. Medical and nursing staff expressed increased trust in our ability to partner with them to help medically fragile patients by using pharmacologic and nonpharmacologic interventions. Since implementation, we have become allies with medical practitioners in addressing broader issues such as delirium, substance use disorders, agitation, and polypharmacy. We are now engaged in multiple collaborative efforts and have a robust presence in hospital academic and clinical endeavors. We believe that this QI approach can address the gap between medical and psychiatric aspects of care for a range of high-risk populations and be replicated in any general hospital.
Acknowledgments
The authors acknowledge the support and guidance of the leadership at NYU Winthrop Hospital: John Collins, chief executive officer; Valerie T. Terzano, R.N., chief nursing officer; Donna Caccavale, M.B.A., R.N.; Eve Dorfman, M.A., R.N.; Lee Moldowsky, M.S.N., R.N., and Monica Santoro, M.S., R.N.