Health care and criminal justice systems are facing increasing challenges from the growing numbers of individuals experiencing behavioral health crises (defined here as a crisis related to mental illness or a substance use disorder) (
1,
2). Law enforcement agencies, emergency departments (EDs), and jails have become the de facto emergency response system for such individuals, yet these entities are not equipped to provide the care these individuals need.
Between 5% and 15% of all calls to 911 emergency services are for behavioral health emergencies and often result in a law enforcement response (
3). A quarter of police-involved shooting deaths are linked to mental illness, half of which occur in the person’s own home. More than 2 million people with serious mental illness are booked into jail each year, and the prevalence of behavioral health conditions in jails and prisons is three to four times that of the general population (
4,
5). Once in jail, people with mental illness are incarcerated twice as long as people without mental illness, and few receive needed treatment (
6–
8). Upon release, with Medicaid benefits interrupted and a criminal record, individuals are more likely to be unemployed, homeless, and rearrested (
6,
9–
11). Then the cycle continues. Even if more appropriate treatment options exist, civil commitment laws and behavioral health facility policies often require law enforcement to conduct mental health transports. A recent survey of U.S. law enforcement agencies estimated that the annual nationwide cost of transporting people with severe mental illness is $918 million. Law enforcement leaders have expressed dismay at the inhumanity of criminalization as a result of law enforcement’s role, along with concerns that the time spent on responding to and handling mental health emergencies may restrict law enforcement’s ability to uphold public safety (
12).
Racism and implicit bias magnify these problems for people of color. Black Americans are 2.6 times more likely to be killed by police than non-Hispanic Whites; when mental illness is taken into account, this difference is nearly 10-fold (
4). For people struggling with substance use disorders, disparate sentencing penalties (e.g., harsher sentences for crack vs. powdered cocaine) result in excessive imprisonment of Black Americans (
13). These long-standing inequities have been underscored by the continued high-profile killings of unarmed people of color by law enforcement. Of note, half of White Americans with mental illness receive the care they need, compared with only 31% of Blacks and Hispanics and 22% of Asians (
14). Reducing racial inequities in emergency response and access to care must be a central focus of any reform efforts.
Social justice movements have created momentum for alternative approaches such as replacing officers with clinical first responders. Law enforcement involvement is unlikely to be eliminated, however. Some situations may pose an unacceptable amount of safety risk to civilian clinicians, and some behavioral health emergencies may not become apparent until after officers are on scene. Solutions to these complex issues will require collaboration between law enforcement and the health care system to optimize responses for each situation, which could involve a law enforcement response, clinician response, or co-response with shared responsibility. For any response to be successful, the responders—whether law enforcement, clinicians, or both—require a behavioral health crisis system that can quickly accept individuals in crisis and provide the care they need, in the safest and least restrictive setting possible.
This policy article is intended as a guide for those who seek better ways to respond to individuals experiencing a behavioral health crisis, beginning with the moment a request for help is made and ending with the successful transition to an appropriate level of care. We describe best practices for crisis responses and outline the components of a comprehensive continuum of care that provides alternatives to law enforcement involvement, ED utilization, and hospital admission. We discuss the importance of addressing this complex issue with a systems-level approach rather than relying on stand-alone programs. Finally, we present policy considerations to assist communities in taking steps toward building an effective crisis response system.
Law Enforcement Responses
The law enforcement response to behavioral health emergencies has been under increasing scrutiny from both social justice movements and the courts. The Ninth Circuit Court of Appeals 2011 ruling in
Glenn v. Washington, which involved the death of a young man in crisis holding a knife, upheld an earlier ruling (
15), stating, “We have made it clear that the desire to quickly resolve a potentially dangerous situation is not the type of governmental interest . . . that justifies the use of force that may cause serious injury.” Instead, officers should be expected to proceed slowly and deescalate the situation. This decision became the basis for many law enforcement agencies to implement or expand Crisis Intervention Team (CIT) programs.
CIT and Training
The CIT model provides law enforcement with tools to recognize individuals experiencing a behavioral health crisis, deescalate the crisis, and divert the affected individual to treatment instead of jail. CIT began in the late 1980s in Memphis, in response to a police shooting of a Black man with mental illness (
16). Its centerpiece is a 40-hour training course that involves scenario-based exercises and participation of community stakeholders, including behavioral health clinicians, treatment agencies, people with lived experience of mental illness, families, and advocacy groups. More than 3,000 jurisdictions have implemented CIT programs across the United States and around the world (
17).
CIT encourages communities to adapt its model to their needs, allowing departments to develop their own curricula and tailor processes to work with local mental health systems. Although pragmatic, this approach creates research challenges (
18). Without a standard implementation or fidelity tool to measure variability across programs, comparative research is difficult, and the findings of the studies are often mixed or inconclusive. There is strong evidence that CIT training improves officers’ knowledge, attitudes about mental illness and treatment, and self-efficacy for interacting with someone who is suicidal or psychotic (
19). When comparing the behavior of CIT-trained versus untrained officers in the field, researchers found that CIT-trained officers are more likely to report verbal deescalation as the highest level of force used (
20), to use less force with resistant individuals (
21), and to refer or transport individuals to mental health treatment, but the effect of CIT-trained officer involvement on the frequency of arrests is mixed (
20,
22,
23). Similarly, system-level pre-post studies of CIT outcomes indicate increases in transports to mental health facilities (
24) but have yielded contradictory results in overall cost-effectiveness (
25,
26). Some of this variability may be related to officer selection. Newer research has compared officers who volunteered for CIT training with officers who were assigned to receive CIT training. Voluntarily trained CIT officers had better self-efficacy, deescalation skills, and referral decisions compared with CIT officers who had been assigned to training. Even when physical force was documented during an incident, voluntarily trained CIT officers were more likely than those assigned to training to refer individuals to treatment services and were less likely to make an arrest (
27). Another potential source of variation may be the availability of mental health crisis services available in a given community (
28).
The National Council for Mental Wellbeing (formerly the National Council for Behavioral Health) and CIT International recommend that 100% of a department’s uniformed patrol officers receive a basic 8-hour training session, such as Mental Health First Aid (MHFA) for public safety, and that the 40-hour CIT training be voluntarily undertaken by a subset of officers large enough to ensure 24/7 availability of trained officers to respond to calls for service (
29). Moreover, 911 services personnel should also receive training to help them dispatch CIT-trained officers when needed. This approach ensures both a basic level of competency among all officers and 24/7 availability of a specialized CIT response.
Although CIT is often thought of as a police training program, its creators continue to underscore that training is only one part of a more comprehensive approach. Once officers are trained to identify a person in crisis and divert that individual to treatment, their first question is often “divert to what?” Therefore, the full CIT model recommends a crisis system with quick and easy access and 24/7 availability (
30). In many communities, such services are often not available, and patients instead board in EDs while waiting for inpatient beds. Oftentimes the officer must wait with them, sometimes for hours, making jail the path of least resistance for officers.
Beyond CIT: Dedicated Specialty Teams
CIT-trained officers are often designated to handle behavioral health calls in addition to their regular duties, whereas dedicated specialty teams focus exclusively on behavioral health. Such teams may respond like regular CIT officers to mental health calls, but their specialization provides time and flexibility to discuss complex cases and collaborate with mental health partners on system improvement efforts. Examples include substance use deflection teams that connect people to treatment in lieu of arrest (
31), mental health case management teams that connect high-risk individuals to treatment or follow-up after a crisis (
32), and teams that reach out to homeless individuals (
33).
Behavioral Health Crisis Response
Crisis Call Centers and “Care Traffic Control”
Crisis call centers are often the first entry point to crisis services, providing 24/7 support via a range of modalities, such as suicide hotlines (staffed by trained professionals), warm lines (for emotional support and often staffed by peers), and text and chat functions. The National Suicide Prevention Lifeline (NSPL) is a nationwide network of >170 crisis call centers and is linked to the Veterans Crisis Line (
34). In some communities, crisis calls are accessed through nonemergency and information lines, such as 211 and 311 or other local crisis lines. As awareness of the utility of crisis lines increases, momentum has grown for a nationwide, easy-to-remember, 3-digit number for NSPL and other crisis lines. The Federal Communications Commission approved a new 988 number for implementation in July 2022 (
35).
Studies of NSPL call centers have found that callers have significantly decreased suicidality during the course of the call (
36), that one-third of callers are successfully connected with mental health referrals (
37), and that less than one-quarter of such calls result in law enforcement or emergency medical services (EMS) being sent without the caller’s assent (
38). Implementation of Applied Suicide Intervention Skills Training (ASIST) across the NSPL resulted in callers feeling less depressed, less suicidal, less overwhelmed, and more hopeful by the end of calls handled by ASIST-trained counselors (
39).
Crisis call centers are well situated to serve as a centralized hub for relaying information and coordinating the appropriate response. Such “care traffic control” functions include dispatching nearest mobile crisis teams, making outpatient appointments, and arranging bed placement. Some systems have crisis line clinicians embedded in 911 communications centers so that behavioral health calls can be diverted to the crisis line in lieu of a police response.
Mobile Crisis Teams (MCTs)
MCTs are typically one- or two-person teams composed of a combination of master’s-level clinicians, behavioral health technicians, or peers (
20). The CAHOOTS (Crisis Assistance Helping Out On The Streets) program in Eugene, Oregon, pairs a clinician with a nurse, paramedic, or emergency medical technician (
40). Some localities have established centralized dispatch for MCTs, often within crisis call centers, aided by technology such as GPS-enabled mobile apps for location tracking and transmission of clinical information.
MCTs meet patients where they are—at home, in the ED, or on the street—eliminating the need to transport them to a more restrictive environment (
41–
43). Studies of MCTs have reported reduction of psychiatric hospitalization and ED use (
44–
46), but additional studies describing clinical best practices in MCTs are needed.
Co-Responder Teams
A variety of co-responder models are emerging in which police officers respond to crisis calls with a clinician, peer, or other social services staff (
47). Teams may ride and respond together, arrive separately, or involve the clinician via phone or video. There is no consensus on which model is most effective, and programs should be adapted to the local context.
Qualitative research indicates that most people in crisis prefer MCT or co-responder teams to police-only teams (
48). In particular, they value responders with mental health knowledge and verbal deescalation skills and a compassionate, empowering, and noncriminalizing approach (
49). Studies of other outcomes have been mixed (
18). A review of police and mental health co-responder programs concluded that these programs decreased arrests and reduced the amount of time officers spent handling mental health calls, but evidence was limited for other impacts of the co-responder model (
50). Furthermore, many programs are limited in hours of operation or geographical area served. In particular, programs experience difficulty when community mental health resources are lacking.
Specialized Crisis Facilities
Crisis facilities vary in scope, capability, and populations served, but all are intended to provide a safe and therapeutic alternative to hospital EDs, inpatient psychiatric facilities, or jail. Receiving crisis facilities accept any individual, regardless of behavioral acuity, including those who may be suicidal, violent, or intoxicated. These facilities are typically staffed with an interdisciplinary team of psychiatric providers, nurses, social workers, behavioral health technicians, and peers, and they may be freestanding or adjacent to an ED or hospital (
51). The CIT model outlines facility attributes critical for law enforcement, including 24/7 availability, faster drop-off times than jail, and a “no wrong door” policy of never turning officers away (
30). Clinical care should follow applicable evidence-based practice standards, such as the Suicide Assessment Five-Step Evaluation and Triage (SAFE-T) (
52) and Project BETA: Best practices in Evaluation and Treatment of Agitation (
53) frameworks. Facility-based crisis care is associated with reduced hospitalization rates, boarding of psychiatric patients in EDs, and arrests (
54–
56). Other terms for these programs include 23-hour observation, psychiatric emergency services, or EmPATH (Emergency Psychiatric Assessment, Treatment, and Healing) units.
“Living rooms,” detoxification centers, and sobering centers provide 24/7 alternatives for less acute needs and often accept police drop-offs for patients who meet their admission criteria. These facilities are typically unlocked and serve patients who arrive voluntarily, are nonviolent, and motivated for receiving help (
57). Living rooms offer a home-like environment with couches and artwork and are staffed predominantly by peer specialists, with limited coverage by a psychiatrist or other provider. They are especially helpful if psychosocial stressors are the main precipitants of the crisis. Detoxification centers provide medically supervised detoxification services, whereas sobering centers employ primarily psychosocial and peer support.
Crisis clinics and mental health urgent care centers offer same-day or walk-in access for outpatient assessment, crisis counseling, medication management, care coordination, and bridge services until the person is connected to appropriate outpatient care. Crisis residential, crisis respite, and peer respite facilities offer longer-term (days to weeks) stabilization in a residential setting. They are often used as step-down care after inpatient or acute crisis care. Some programs may accept low-acuity patients from law enforcement.
Postcrisis Care
A variety of models have been developed to facilitate a successful transition to community-based care. These models range from predischarge interventions such as psychoeducation and structured discharge planning, to postdischarge interventions such as follow-up phone calls and case management, to transitional interventions that engage with clients before discharge and continue for some time after discharge. These services can be provided by nurses, social workers, case managers, or peers. Small study sizes and the wide variability in program elements, intensity, and duration make comparative research among different models difficult, and effects on readmission rates are often mixed or inconclusive (
58). Earlier appointments (within 3 days) are associated with higher attendance and longer time in the community without ED use (
59). Several studies have focused specifically on suicide-related outcomes, revealing promising evidence that follow-up calls and “caring contacts” (e.g., letters, postcards, text messages, and phone calls) decrease repeat suicide attempts (
60,
61) and are cost-effective (
62,
63).
Systems Thinking
Crisis Services Versus Crisis Systems
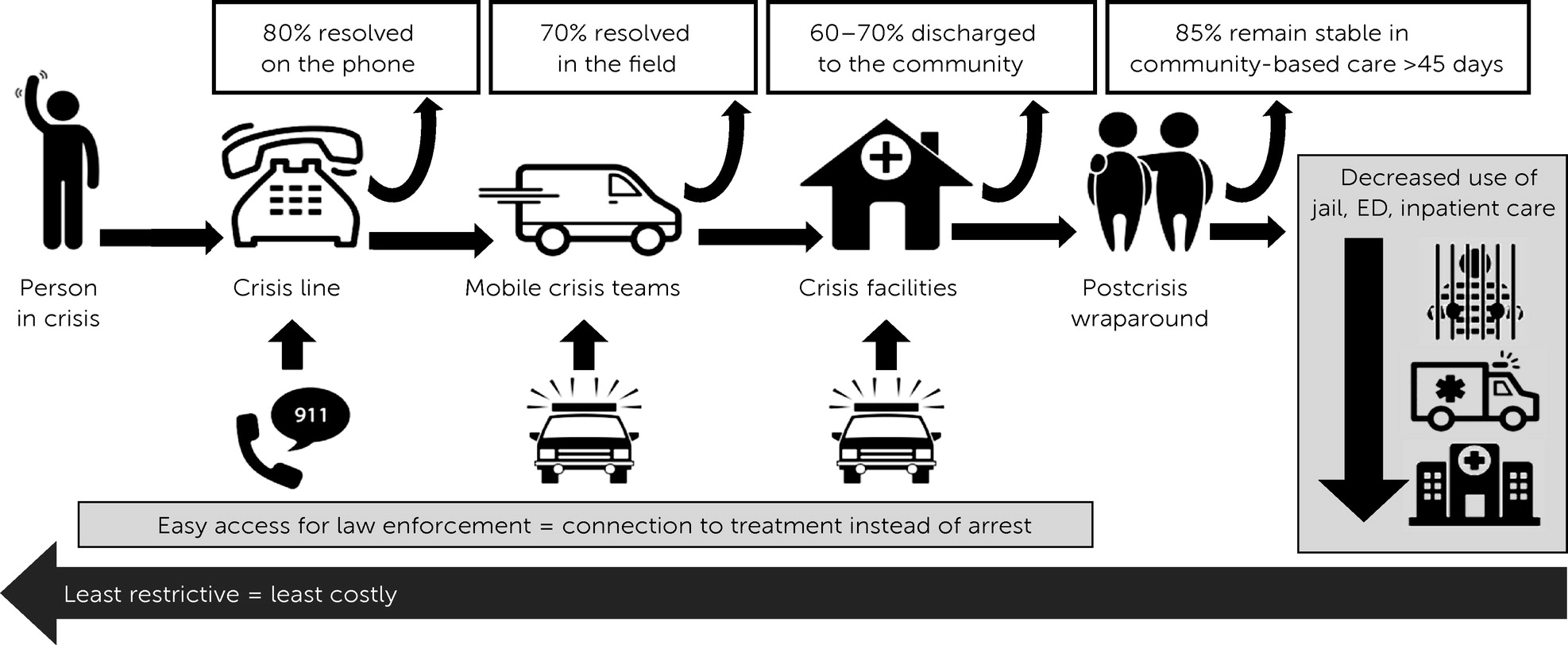
Although each of the individual programs described above may improve outcomes, their impact is multiplied when an array of programs and services work together as a coordinated system to achieve common goals. This approach is illustrated in
Figure 1, depicting the crisis system in Tucson, Arizona (
64). In this model, health care and law enforcement stakeholders agree on a common goal of preventing avoidable jail, ED, or hospital use by providing care in the least restrictive setting that can safely meet the needs of an individual in crisis. Because less restrictive settings tend to be less costly, clinical and financial goals are aligned as well. A Regional Behavioral Health Authority (RBHA) contracts with provider agencies to create an array of services organized along a continuum of intensity, restrictiveness, and cost. At all points along the continuum, easy access for law enforcement (e.g., 911 colocation, co-responder teams, and no-wrong-door policies) facilitates connection to treatment instead of arrest. To further incentivize coordination, some contracts confer a “preferred customer” status to law enforcement so that, for example, response time targets for MCTs are faster for calls that involve law enforcement.
Governance and accountability are key to ensuring that crisis services operate as an organized and coordinated system. In the Arizona model, the RBHA serves as the “accountable entity” via its role as the single payer and regulator for the crisis system, accountable to the state for both fiscal and clinical outcomes and financed via braided funding from a variety of sources (e.g., Medicaid, Substance Abuse and Mental Health Services Administration [SAMHSA] block grants, and state and local funds).
Several frameworks describe crisis services from a systems perspective. The Crisis Now Model (
57) and SAMHSA’s Best Practice Toolkit (
65) describe essential services for a crisis continuum of care: call centers, mobile crisis teams, and stabilization facilities. The National Council for Mental Wellbeing’s Roadmap to the Ideal Crisis System (
66) provides a blueprint for building the services, financing, and governance structures needed for a coordinated crisis system. The sequential intercept model (SIM) describes the typical pathway through the criminal justice system for a person with behavioral health needs and identifies opportunities for the health care system to intervene, with intercepts 0 and 1 focused on crisis care (
67). SIM mapping can be a useful exercise to engage stakeholders in system planning (
68).
Comprehensive Law Enforcement Approaches
Like crisis systems, public safety agencies benefit from a broad organizational approach that goes beyond the implementation of a single program or training. The International Association of Chiefs of Police created its “One Mind” campaign to encourage this type of systems thinking. The campaign challenges law enforcement leaders to begin implementing a crisis system by committing to three core elements: partnership with community mental health agencies, model policies to guide interactions with individuals experiencing a behavioral health crisis, and training programs built on MHFA and CIT (
69).
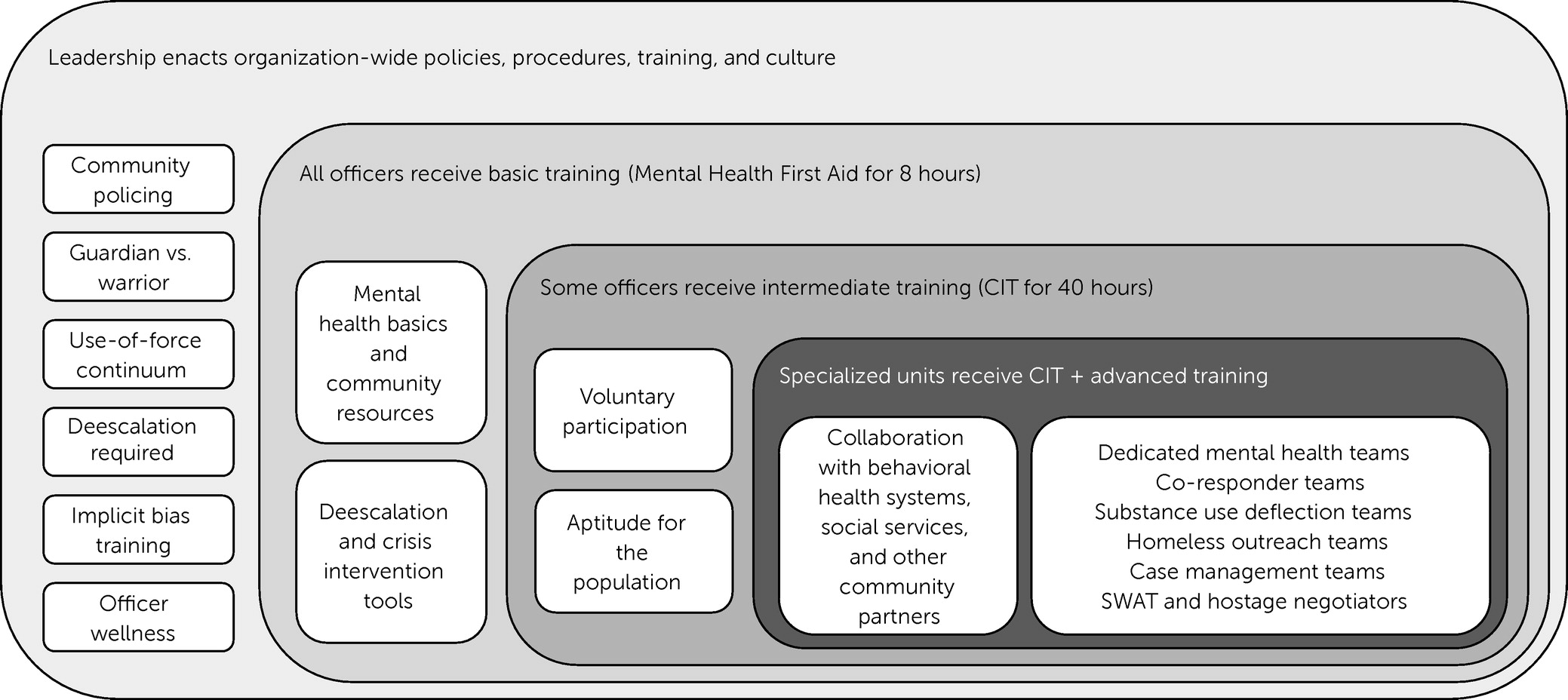
Figure 2 illustrates how these elements fit together to create a systematic approach across the Tucson Police Department for helping individuals in crisis (
64). Organizational leadership provides a foundation by creating the culture and operational procedures needed to support safe and compassionate interactions with people in crisis. MHFA training provides a basic level of competency to all police officers, and those with the aptitude and interest are incentivized to pursue CIT training. Specialized teams receive further training, such as motivational interviewing and trauma-informed care, and work to develop partnerships with behavioral health and other community partners. As they continue to gain knowledge and experience, members of these specialized teams also serve as subject matter experts to the rest of the organization.
The Police–Mental Health Collaboration (PMHC) Framework, authored by the Council of State Governments Justice Center, also encourages law enforcement agencies to take a comprehensive approach to responding to people with behavioral health needs (
70). This framework guides law enforcement executives on how to partner with behavioral health and social service providers to implement data-driven, agency-wide responses (
47). The U.S. Department of Justice Bureau of Justice Assistance’s Law Enforcement–Mental Health Learning Sites are model agencies across the country that have implemented these types of sophisticated innovations. The sites employ many of the programs described in this article, tailored to work for their individual communities. They also provide free technical assistance and host site visits for jurisdictions looking to implement PMHCs (
70).
Cost Savings Across Systems
Results from numerous studies have indicated that crisis services such as mobile teams and facility-based crisis stabilization reduce costs arising from ED or psychiatric inpatient use (
44,
71,
72). Within the justice system, law enforcement approaches such as CIT, co-responders, and dedicated teams reduce costs related to jail bookings and special weapons and tactics team deployments (
73,
74). But the true power of a collaborative approach becomes apparent when its impact across silos is considered. For example, an analysis of the crisis system in Maricopa County, Arizona, which includes many of the elements described in this article, estimated that a $100 million investment in crisis care resulted in savings of $260 million in psychiatric inpatient spending, $37 million in ED costs, 45 years of psychiatric ED boarding hours, and 37 full-time equivalents of police officer time and salary (
75). The CrisisNow.com website includes a “crisis resource need calculator” that allows users to model services, costs, and savings for their local communities on the basis of the Arizona model (
76).
Policy Implications
Stakeholder Engagement and Collaboration
Strong partnerships are critical to generating the enthusiasm for designing, funding, and implementing crisis systems and to ensuring that these systems function effectively on an ongoing basis. Potential stakeholders include state and local governmental agencies, payers, law enforcement, 911 services, behavioral health providers, social services agencies, and advocacy groups (
77). It is imperative that these processes actively engage and incorporate input from individuals with lived experience of a behavioral health crisis. Strategic inclusion of elected officials or other influential community leaders may effectively garner support.
How to begin crisis system implementation largely depends on the dynamics within each local community. Momentum may be driven by county leadership seeking to reduce the jail population, law enforcement agencies strained by mental health transports, or community leaders galvanized by a tragic outcome involving a person in behavioral health crisis. Collaborative groups can be built on existing organizational infrastructure (e.g., a county task force or CIT steering committee) or created de novo. For communities just beginning to organize, data collection can be a good first step, because data help engage stakeholders and build the business case for investing in crisis services. Most localities already have at least some components of a crisis system, and system-mapping exercises (e.g., SIM mapping) could both ensure a better understanding of the existing context and engage additional stakeholders. The Stepping Up Initiative—a joint effort of the American Psychiatric Association, the National Association of Counties, and the Council of State Governments—challenges counties across the United States to sign a resolution pledging to reduce the prevalence of mental illness in jails and includes a framework for engaging stakeholders, setting goals, and learning from the >500 counties that have made the pledge thus far (
78).
Successful collaborations are iterative and longitudinal and may begin with small, simple improvements that require no additional resources (e.g., setting up a process for partners to better communicate with one another). By building on the successes of these “easy wins,” partners can progress to more sophisticated solutions. Eventually, the collaborative is no longer building a crisis system but rather monitoring and improving the system they built.
The inclusion of people with lived experience of crisis systems and people of color in these types of collaborative bodies is essential to ensuring that the crisis systems deliver care to those who are most in need. People who have directly experienced the crisis system or witnessed how the system works for their family and community can provide their perspectives on interacting with a truly recovery-oriented, trauma-informed, and culturally responsive system. Crucially, however, systems must advance beyond strategies that tokenize or marginalize these perspectives in their planning and oversight processes. The balance of power in collaborative groups will often favor privileged people who are working in government or in larger service provider agencies. Therefore, it can be helpful to shift that power by including multiple representatives of color and those with lived experience in collaborative groups. Treating these representatives as experts and compensating them for their time can also ensure that people who are serving outside of their professional capacity will have the support necessary to meaningfully participate in the group.
Financing
Crisis financing models vary widely by state and often draw on multiple funding sources. Individual services can be billed to Medicaid and other health insurance, but additional funding sources are needed to support the infrastructure costs of 24/7 on-demand access to care (
79). State general funds, local funds, and federal block grants are often used for this purpose, and for the first time, the SAMHSA Mental Health Block Grant (MHBG) contains a set-aside for crisis care in the 2021 budget (
80). The upcoming 988 services implementation has been an impetus for states to bolster crisis infrastructure via federal planning grants, telecommunications fees, and new appropriations of state funds for crisis services. The American Rescue Plan Act of 2021 further incentivizes states to leverage Medicaid by providing an 85% federal match for bundled payments to MCT (
81). Medicaid 1115, 1915(b), or 1915(c) waivers offer states a powerful tool to combine multiple funding streams, maximizing efficiency and accessibility by pooling resources to create a common safety-net crisis infrastructure that can serve anyone in need, regardless of payer (
82). Emerging financing models, such as value-based payments, provide additional mechanisms to invest in crisis and other social services (
83,
84). In communities with robust crisis systems, co-responders funded by the behavioral health system can be allocated to assist law enforcement officers without additional cost to law enforcement agencies.
In contrast, Medicare and most private health plans provide little or no coverage for crisis services, and care for their members often is financed by the aforementioned safety-net mechanisms. These payers must be held accountable to providing parity coverage for behavioral health emergency care. The Centers for Medicare and Medicaid Services Emergency Triage, Treat, and Transport demonstration program provides parity Medicare reimbursement for EMS to transport patients to “alternative” destinations other than the ED, including crisis facilities (
85). Models like this are a step in the right direction.
Regulations and Accreditation Standards
Because most crisis services are funded and regulated at the state or local level, they vary widely in program definitions, licensure, accessibility, and quality. Furthermore, the lack of standard definitions and nomenclature hinders the billing of crisis services to private payers (
79). For these reasons, the Interdepartmental Serious Mental Illness Coordinating Committee recommended the development of national standards in its first report to Congress (
86). In the meantime, accreditation exists and should be incentivized for some individual crisis programs via organizations such as the American Academy of Suicidology, Commission on Accreditation of Rehabilitation Facilities (commonly known as CARF) International, and the Joint Commission; reimbursement can be sought through widely accepted standard-of-care frameworks such as the Level of Care Utilization System for Psychiatric and Addiction Services Standards (commonly known as LOCUS) and the American Society for Addiction Medicine (commonly known as ASAM) Treatment Criteria for Addictive, Substance Related and Co-Occurring Conditions (
87).
Standardizing practice across the nearly 18,000 law enforcement agencies has been even more challenging. Although best practice standards have been proposed through various initiatives, reform and accountability are realized only after a Department of Justice consent decree is enacted. However, support has grown for police reform legislation that includes accreditation standards and incentives for law enforcement agencies to adopt more progressive practices.
Civil Commitment and Mental Health Transports
Although many people in crisis voluntarily seek care, some lack the capacity to make rational decisions. In these situations, state civil commitment statutes define the role of law enforcement in detaining and transporting individuals involuntarily for psychiatric evaluation (
88). State statutes vary widely in terms of criteria, duration, and use of civil commitments; however, comparative research of these statutes is difficult because of inconsistent data collection across jurisdictions (
89,
90). In some states, only law enforcement—not clinicians or family—can initiate the civil commitment process. Others require that the individual’s risk for harm to self or other be “imminent” and thus forces families to wait for the individual to decompensate, creating the conditions for a volatile and risky encounter with law enforcement.
Many statutes require law enforcement to perform involuntary transports to treatment facilities, and some behavioral health treatment agencies require police transport even if the individual wants to go voluntarily, creating the potential for further trauma and harm. A recent survey of law enforcement agencies estimated that 65% of transported patients did not pose a risk for harm to others and could be transported by another entity (
12). Many of these laws were written decades ago and should be updated to support earlier interventions and alternative transportation options, with law enforcement used only as a last resort when no other means is available to protect the safety of the individual or those providing the transport.
Data Sharing and Quality Improvement
At the individual level, data sharing can help law enforcement agencies and behavioral health providers coordinate care. For example, knowing that someone is receiving behavioral health services can help officers choose the right intervention. Conversely, law enforcement often has information about past interactions and psychosocial factors that can aid clinicians in their assessment. HIPAA is often seen as a barrier to data sharing but does allow sharing in emergencies. Data can also be shared via business associate agreements or by obtaining a patient’s consent. When protocols are developed, it is important that agencies and other entities reach consensus regarding applicable state and federal laws and seek input from stakeholders with lived experience so that concerns about privacy and other potential negative consequences of data sharing can be addressed.
At the system level, data are a powerful tool for quality improvement and will be increasingly tied to financing as alternative payment models evolve (
91). However, very few quality measurement standards exist for crisis services. Some standard measures are used by crisis call centers (
92), and a measure set for crisis facilities has been proposed (
93). Reporting through SAMHSA's Uniform Reporting System may be expanded to include crisis metrics as a condition of the new MHBG crisis services set-aside (
84). In the meantime, communities can choose metrics that guide their system toward common goals. For example, as shown in
Figure 1, the various system components report the percentage of patients stabilized without the need for a higher level of care. Each of these measures is one facet of the overarching goal of crisis stabilization in the least restrictive setting possible.
Data can also be used to address health system disparities and support racial equity in policing. Analyzing outcomes by race, gender, socioeconomic status, and other demographic characteristics can reveal inequities in key metrics, including decisions about disposition and referrals, use of coercive practices, diagnoses, and access to high-quality care. Disparities in key law enforcement outcomes such as use of force, arrest, and connection to care can reveal implicit bias in policing (
70). Openly and transparently sharing such data with the public is an important step toward gaining trust and implementing policies to address these problems.
Disparities, Inequities, and Racism
The treatment of a community’s most vulnerable members plays an important role in building trust; thus, improving responses to behavioral health emergencies is critical to reform efforts. As communities across the country have declared racism a public health crisis (
94) and as social movements such as Black Lives Matter have motivated jurisdictions to examine law enforcement’s role, addressing racism in the crisis system is a challenge that many communities are now poised to tackle.
Make an explicit commitment to racial equity.
As communities are declaring racism a public health crisis, crisis providers, payers, and law enforcement departments can explicitly commit to racial justice in their agency’s mission or other foundational documents. This explicit commitment, coupled with earnest adherence to it by the agencies’ leaderships, can help support the adoption of policies aimed at improving racial equity. The Center for Policing Equity notes that this commitment should also include policies that directly address discrimination and implement disciplinary action, including dismissal, of officers who have engaged in discriminatory behavior (
95).
Conduct racial equity impact assessments.
Jurisdictions should engage in explicit self-reflective processes that center racial equity as a goal and seek to identify policy and practice improvements that can help achieve equity. Resources such as the Racial Equity Toolkit from the Government Alliance on Racial Equity (
96) can help structure this process. Assessments should include data on race and ethnicity to enable stratified analyses of any disparities in policy outcomes among individuals differing in race-ethnicity (
97). Asking questions about who might benefit from or be harmed by a policy can help identify potentially racist policies or practices. For example, many observers have noted the potential for harm and criminalization from well-intentioned policies that send law enforcement to follow up with people after a drug overdose. A racial equity assessment before implementation can illuminate the potential to increase disparities or cause trauma and harm (
98).
Support training of crisis system actors.
Many communities have taken steps to ensure that their health care workforce understands how race, racial bias, and structural racism can affect crisis system outcomes. Traditionally, this approach has taken the form of training in cultural competency—the ability to understand the needs, values, and behaviors of people from different cultures and to apply that understanding to improve care. The evidence base for this approach is mixed, with more support for positive impact on knowledge and skills of medical professionals than on clinical care or health outcomes (
99).
In recent years, researchers have argued that the concept of cultural competency is insufficient to produce system change or improve clinical care (
100) and advocate instead for training that increases a clinician’s ability to be structurally competent and culturally humble. Structural competency is an understanding of how social, economic, and political structures (e.g., inequitable access to good-quality housing and living in neighborhoods with disproportionate incarceration rates) influence health outcomes (
100), and cultural humility is the state of being open and curious about other cultures while continually examining the impact of one’s own culture and biases (
101) on one’s interactions with others. These concepts may not only help medical professional address interpersonal bias but also encourage advocacy for policy reforms that address social determinants of health inequities such as structural racism (
102).
Similarly, law enforcement agencies have increasingly adopted implicit bias training. Its goal is to make police officers aware of their own unconscious racial biases (e.g., association of Black people with criminality) and their potential impact on behavior (e.g., use of force and decision to stop a motorist). Studies of the effectiveness of implicit bias training have yielded mixed evidence, with more support for the idea that such training can increase officers’ understanding of their own biases and their impact on behavior and less evidence indicating that training actually changes behavior (
103).
Invest in community-led and -operated crisis supports and “health-first” responses.
Crisis services should be tailored such that they add value to the community they serve. For example, crisis provider organizations located in and led by people from communities of color may reduce barriers to accessing care, such as a mistrust of health care systems. Such investments can also serve as a source of economic support for communities of color that have a history of economic disinvestment and higher rates of poverty, which can worsen health outcomes. Tools such as the Self-Assessment for Modification of Anti-Racism Tool developed by the American Association for Community Psychiatry can help crisis care providers adopt clinical best practices for antiracist mental health care whose goals include increased awareness of racial discrimination, racial profiling, microaggressions, and racism; assessments adapted to the real needs of Black individuals; a person-centered approach to medications; and a treatment approach that addresses the needs and issues arising from racism experienced by Black individuals (
104,
105).
Communities of color are increasingly advocating for health-first or health-only crisis responses similar to CAHOOTS and other MCT models. When governments listen to and act on these calls, they acknowledge the capacity of communities to articulate what they need to improve the health of their own residents. As these programs spread, it is imperative to examine the outcomes of health care (e.g., ED use and connection to ongoing care) and criminal justice (e.g., rate of law enforcement involvement as backup and use of force) by race and other key demographic characteristics to ensure that these initiatives are having an equitable impact.
Conclusions
Both health care systems and law enforcement agencies must adopt systems approaches to serving individuals in crisis that strive toward a common goal of connecting people to care in the least restrictive setting, while minimizing law enforcement involvement and ensuring the safety of the individual in crisis, care providers, and the public. Stakeholders will need to collaborate closely to ensure adequate planning, financing, accountability, data collection, and oversight, including ongoing assessment of racial bias and health inequities. Successful solutions have the potential to improve health outcomes for individuals in crisis, increase public safety by reducing demand on police, build community trust, and reduce costs across health care and criminal justice systems. With growing support for meaningful change in these complex systems, every effort should be made to seize the moment and improve the accessibility, quality, and equity of behavioral health crisis care in our communities.