The involvement of families in the mental health care of persons with severe mental illness is widely acknowledged to be critical to good clinical practice. Extensive treatment trials have shown that participation in family psychoeducation—a specific group of family involvement treatment models—decreases relapse rates (
1,
2,
3 ). Findings from these trials have effect sizes that are comparable with those observed in psychopharmacologic trials for schizophrenia (
4 ). Effective family psychoeducation models last at least nine months and provide illness education, support, problem-solving training, and crisis intervention services. Such robust findings have led to the inclusion of family psychoeducation in virtually every set of evidence-based practice recommendations and treatment guidelines for schizophrenia. The President's New Freedom Commission report (
5 ), the Surgeon General's report on mental health (
6 ), and the Institute of Medicine's report
Crossing the Quality Chasm (
7 ) all emphasize the need to offer families support and include family members in the process of care in order to improve outcomes and experiences for both consumers and families. Despite these imperatives, efforts to implement family psychoeducation in the United States have reached few families. Surveys and record reviews indicate that families in this country have minimal contact with their ill relative's mental health care providers.
To assess the state of the art regarding family psychoeducation and to come to a consensus on the necessary next steps to increase family involvement, the VA sponsored a conference, the Family Forum, a one-and-a-half-day event held in Linthicum, Maryland, on September 18–19, 2006. A national VA family work group was tasked with nominating individuals who were either experts in family interventions or providers implementing family interventions. Nominees were invited; those who could not attend were asked to nominate other individuals, and these candidates were then reviewed by the VA family work group. The final 40 attendees included academic leaders in family services research from both the VA and universities, administrators from VA Central Office who lead evidence-based implementation across the VA nationally, and frontline VA service providers whose medical centers had received Mental Health Enhancement Funds from the VA Office of Mental Health Services to implement family psychoeducation.
The forum's goals were to identify the challenges to implementing family psychoeducation and involving families in mental health care and to achieve consensus on how best to move forward with approaches that integrate new paradigms of delivering care (such as the recovery paradigm). The conference included breakout sessions and presentations on evidence-based family programs, comparisons of different types of family services and family psychoeducation, and assessment tools for both clinical and research endeavors. Issues raised during breakout groups were summarized and presented to the full group for discussion.
Minutes were taken throughout the meeting and consolidated into an outline for this article. Four main themes emerged: family psychoeducation models should be optimized by efforts to identify the factors mediating their success in order to maximize dissemination; leadership support, training for managers and clinicians in family psychoeducation models, and additional resources are necessary to successfully implement family psychoeducation; given that family psychoeducation is not appropriate, indicated, or acceptable for all families, additional complementary strategies are needed that include families in mental health care in order to increase the proportion of consumers and families who participate in services, while using relatively fewer per capita resources; and work is required to refine and validate assessment instruments that measure the full range of both consumer and family outcomes as well as the intervention process.
This article briefly summarizes the evidence and presents the consensus on each of these themes. A treatment heuristic borne out of the discussion at the forum is also presented. The article concludes with opportunities for the research and clinical communities to expand the proportion of families served.
Mediators of psychoeducation to maximize penetration
The Family Forum provided an opportunity to discuss randomized controlled trials that indicated the efficacy of family psychoeducation in reducing symptomatic relapse and hospitalization rates and in improving medication compliance in schizophrenia. Five published meta-analyses have confirmed these benefits (
8,
9,
10,
11,
12 ). However, forum participants identified serious practical difficulties in implementing family psychoeducation in nonresearch settings as well as unresolved research questions that limit our understanding of how to best structure the intervention to facilitate implementation.
Although family psychoeducation is ostensibly a specific model of family involvement, it may best be thought of as a collection of programs because it has been operationalized and implemented in various ways. A review of the empirically based family psychoeducation manuals reveals that although family psychoeducation interventions share many characteristics, there are considerable differences among them. The various programs share an emphasis on illness education, an empathic stance, formal or informal problem-solving training, and support for treatment adherence. However, they differ with respect to the proportion of time the consumer is present in the family sessions, the location of the intervention (home, clinic, or both), the degree of emphasis on formal skills training, the format (individual, group, or combination), the intensity of contact (weekly, biweekly, or monthly), and the length beyond nine months (up to three years).
With the exception of individual versus group interventions, these variations in family psychoeducation have not been systematically studied, so guidelines for the clinician (and therefore guidelines for implementation and dissemination) are absent. With respect to whether the intervention is conducted individually or in groups, the data suggest that the results of the two are comparable (
13 ). The slight advantage of multiple-family groups over individual group interventions reported by McFarlane and colleagues (
1,
14 ) is found only when examining results from people who have completed treatment. Because there are considerable dropouts in multiple-family groups, intention-to-treat analyses are appropriate, and in these analyses the advantage of multiple-family groups is not as robust (
1,
14 ).
The specific mechanisms by which family psychoeducation generates its benefits are unclear. Because many family psychoeducation trials compare the intervention with customary care or waiting-list control groups (
2,
15 ), positive findings may result from the intervention or simply more frequent therapist contact. Furthermore, tests of hypothesized mediating variables have yielded contradictory findings. Consider the case of improved family problem solving, which was hypothesized by Falloon and colleagues (
16 ) to underlie the positive benefits of behavioral family therapy. Although the initial investigators reported significant improvements in problem solving (
16 ), a more fine-grained analysis (
17 ) found no significant improvement in communication or problem-solving skills associated with the more intensive, applied family treatment in the Treatment Strategies in Schizophrenia study (
13 ). In another case, an early study indicated that reduced negative reactions (such as expressed emotion) by family members could underlie the positive benefits of family therapy (
18 ), yet a later study found no effect of family therapy on relatives' negative reactions (
19 ). Only one of the recent meta-analyses showed support for family interventions in reducing negative reactions (
11 ).
Participation in an empirically validated family psychoeducation program clearly seems to confer a number of benefits that were not considered or measured by treatment originators yet may be integral to their positive impact. For example, participation in family psychoeducation typically permits easier access to the treatment team. Although such access is likely to promote better outcomes, it is rarely mentioned in study publications. Similarly, almost all of these programs include helping families to identify prodromes and develop a plan for rapid response. If such plans were implemented, they would probably lead to fewer acute exacerbations, yet use of specific relapse prevention plans has typically not been formally measured or linked with outcomes in family psychoeducation studies. Also, studies have indicated that education alone is not efficacious; instead, education in addition to support, problem-solving training, and crisis intervention are important components of efficacious family therapy (
20 ). Thus, although meta-analyses clearly indicate that participation in these programs can reduce relapse, we have limited knowledge of the critical elements in the interventions. More data on the mediators, or critical elements, would increase the likelihood of successful implementation of family psychoeducation and increase its acceptability among consumers, families, and providers.
In summary:
• How family psychoeducation programs achieve their effects is not clear.
• Identification of causal therapeutic mechanisms would provide direction for the development of effective, more flexible, modifications of family psychoeducation models.
Resources for successful implementation of psychoeducation
Theoretical and experiential literature has recently been published on the obstacles to implementation of family psychoeducation in routine practice. Forum participants identified barriers facing each stakeholder group (organization, provider, family, and consumer) and ways to address these barriers in order to serve the broadest population of consumers and their families. The group concluded that for family psychoeducation to be viable, three elements were essential: leadership support, training and ongoing supervision in family psychoeducation models, and adequate access to resources.
Leadership support
Forum participants' experience and the literature (
21 ) indicate that a top-down mandate from agency leadership to implement family psychoeducation will not lead to sustainable programs unless mechanisms for additional and continued supports are built in to such programs. Leadership must also initiate a process of explicit plans for rollout, adoption, and sustaining of family psychoeducation. Key stakeholders, clinic-level opinion leaders, and potential referral sources should be involved in the planning process from the outset (
22 ). Leadership representatives on various governing bodies (such as nursing, clinic, and hospital administrations) need to be consistent in emphasizing the importance and value of implementing family services so that human resources and frontline staff receive a clear message about expectations for family psychoeducation programs (
21 ). Development and circulation of position descriptions can be useful for familiarizing frontline staff with job skills, job tasks, and performance expectations associated with staff delivery of family psychoeducation. Position descriptions also assist in educating leadership about the skill sets necessary to conduct family psychoeducation and how these skills intersect with those of existing positions. Explicit incentives for adoption and competent delivery of family psychoeducation (such as provider pay-for-performance plans and agency performance measures) may be useful.
Systematic training and ongoing supervision
For programs to succeed, providers and managers must have the core knowledge, attitudes, and competencies needed for family psychoeducation. Ideally, family psychoeducation developers would train providers and managers in these competencies and provide ongoing supervision for them. Personal contact between the family psychoeducation developer and adopters builds commitment for use and should occur both during training and throughout program implementation. Training in the family psychoeducation models is necessary to combat the reluctance of some individual frontline staff to implement family psychoeducation.
Providers' reluctance seems to be driven, in part, by limited skills in working with families, pessimism about the extent of family involvement in the lives of many individuals with severe mental illness, hopelessness about being able to modify long-standing negative consumer-family relationships, and limited knowledge about positive outcomes from such services. Providers are also troubled by not having enough time to implement and sustain the services, and providers report that managers have a lack of understanding of the time involved for successful implementation (
23 ). Passive approaches to addressing reluctance (for example, simple distribution of literature on efficacy studies) do not induce behavior change, lead to implementation success, or improve care (
24,
25 ). Training that is extended over several months and that uses multimodal methods (live demonstrations, videos, role plays, and testimonials from families, consumers, and successful family psychoeducation programs) has been found to be superior to training that includes only didactic methods (
3,
14,
18 ).
Adequate resources
Adequate resources are necessary for effective implementation. Family psychoeducation requires a front-loading of investment (providing adequate staffing, training, and supervision in family psychoeducation models; building a family-friendly agency; and advertising the program) that is expected to be recouped by improving outcomes. Agencies that are family friendly must be flexible if they are to meet the needs of their population of families. For example, such agencies might require evening and weekend hours and staff for those extended hours. They might also require resources to cover costs of providing family psychoeducation in the community and transporting community members to the agency.
In summary:
• Leadership needs to provide consistent and strong support for family psychoeducation while involving key stakeholders in implementation plans.
• Training should involve providers and managers, use multimodal methods, extend over several months, and involve contact with model developers.
• Resources are necessary for the up-front costs of implementing these programs and for maintenance of a family-friendly agency.
Complementary strategies to family psychoeducation
A critical issue that emerged from attempts to understand low rates of family psychoeducation use was the failure to consider family psychoeducation interventions in the context of the larger universe of family services for severe mental illness. In much the same manner that assertive community treatment is not appropriate, cost-effective, or acceptable to all consumers with severe mental illness, their families, or both, neither is family psychoeducation appropriate, cost-effective, or acceptable for all consumers and families. Some families may benefit from support but do not necessarily need an intensive intervention. Other families may not be receptive to long-term services but may undertake a briefer intervention.
Family Forum participants felt that, as the field focuses on implementation of family psychoeducation (currently the only evidence-based family involvement practice), we should not neglect the development and evaluation of other family-based strategies to support recovery. Interventions for families and consumers should be tailored to the needs of participants and will vary over time and circumstance. Further, successful development, implementation, and evaluation of an array of family-based services and interactions are very likely to increase and expand the appropriate utilization of family psychoeducation. The goal of adopting a treated-population perspective is to provide family services that are well matched to the consumer's service needs. This will permit the delivery of appropriate services to large numbers of consumers while using relatively fewer resources.
Efforts to advance a treated-population approach must address the needs of each key stakeholder, starting with the consumer. A subset of programs that address both consumer and family needs was discussed. The Family Member Provider Outreach intervention, which is a newly developed, two-phase manualized program, systematically engages the consumer in a discussion about family issues and concerns, encourages the expression of ambivalence, educates about options, and provides consumers with skills to talk with family members. Results from a pilot study of the Family Member Provider Outreach program indicate that this may be a promising approach to increase rates of family involvement in treatment, including but not limited to family psychoeducation.
Consideration of the treated-population approach also requires exploration of the relative's perspective. Family members typically benefit from access to the treatment team, a menu of options for education and support, and skill building. Naturally, they want to meet these needs as easily as possible. E-mail holds promise for connecting relatives with the treatment team efficiently, provided that security of information can be established and that families have access to a computer. Internet-based support and educational programs also address barriers to access often cited by families, especially in rural areas. Programs such as Support and Family Education (
26 ) provide open educational and support groups for families that allow attendance at the family member's convenience and may provide a bridge to family psychoeducation.
Other options beyond family psychoeducation are community-based services such as the National Alliance on Mental Illness' Family-to-Family education program or the Journey of Hope family education course. These models are not clinical services but are offered by unpaid peer volunteers. They cannot substitute for family psychoeducation or other strategies that mental health providers use to link with families, but their potential to reduce families' subjective illness burden and to increase coping and knowledge of mental illness merits attention.
The family services heuristic
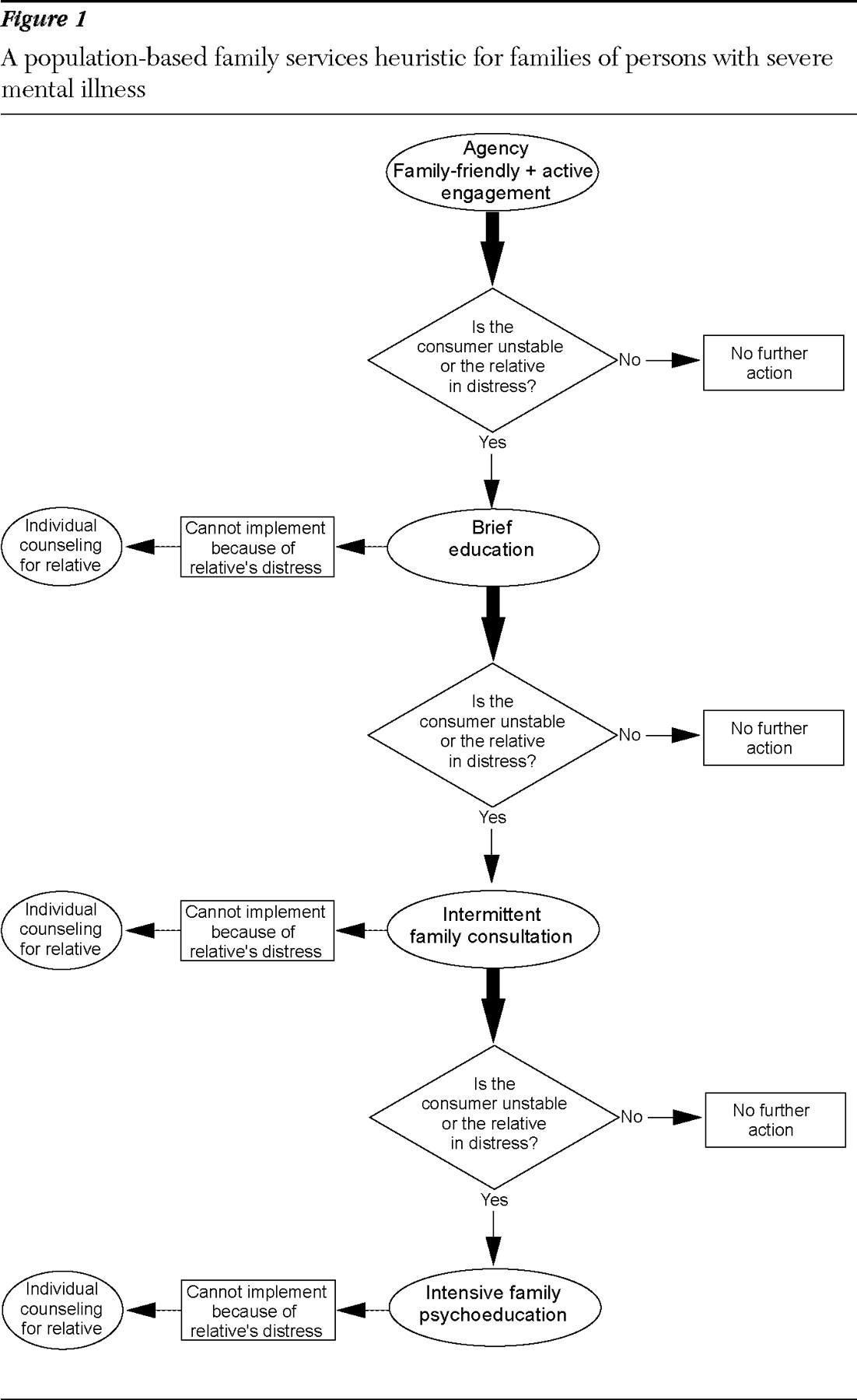
Family Forum participants discussed the potential of the heuristic shown in
Figure 1 to assist clinicians and agencies in implementing a more population-based approach to family services for severe mental illness. The heuristic provides the foundation for this approach by suggesting that interventions be adjusted to accommodate family and consumer needs and circumstances. This heuristic is to be utilized by an agency with consumer services in addition to family services.
Family-friendly agencies. Agencies should strive to be family friendly and actively engage consumers and their families in treatment planning through assertive outreach (top of
Figure 1 ). A family-friendly agency has a deep understanding of and respect for what it means to have a loved one with a severe mental illness and a staff with the knowledge and skills to work with families. Family-friendly agencies have active procedures to promote a comfortable and nonjudgmental exchange with families and forge collaborations with community groups such as their local chapter of the Alliance on Mental Illness. Readily available informational brochures and occasional open family education forums facilitate this type of environment.
Brief education. The components of the first level of the heuristic may be sufficient to address the concerns of many consumers and family members without the need for any other intervention. However, any indication that the consumer is unstable or that the relative is experiencing distress should trigger referral to the second level of intervention: brief education. Markers of a consumer's need for referral include persistently high symptom levels, hospitalization, lack of active participation in treatment, or lack of progress on recovery goals. Markers of family need, which are mostly reflective of distress, include frequent calls to the clinic, complaints about the consumer, or reports of sadness, progressive withdrawal, or self-sacrificing behavior. In the presence of any of these markers, the family can be referred to an educational program in either the clinic or the community. Although participation in such programs typically does not affect consumer outcomes (
27,
28 ), it can increase caregiving satisfaction and reduce caregiving-related information needs (
29 ), obviating the need for more intensive intervention.
Intermittent family consultation. Even after involvement with a family-friendly agency, active consumer and family engagement, and brief education, if consumer or family markers for more intensive intervention still exist, referrals for intermittent family consultation are indicated. Rather than the minimum nine-month commitment required for effective family psychoeducation, intermittent family consultation typically involves between one and five sessions during which the consumer and relative work to resolve specific issues. Sessions are typically held in the clinic, build on the educational material covered previously, and address focused issues (such as where the consumer will live or an exacerbation of symptoms). The goal is issue resolution rather than skills training. Several models of family consultation have been described in the literature (
30 ). One advantage of family consultation is that it can be provided numerous times as a low-intensity intervention. For many consumers and relatives, the ongoing availability of such support on an as-needed basis will be sufficient.
Intensive family psychoeducation. When consumer or family needs persist despite participation in the family services mentioned above, referral should be made to more intensive, evidence-based family psychoeducation programs. These programs involve more formal skills training, especially around problem solving. They are labor intensive and dictate completion of out-of-session assignments and regular attendance. For those who expend the effort, the benefits can be invaluable.
It is possible that at any stage of intervention (brief education, consultation, or family psychoeducation) clinicians may become aware that the relative has little capacity to participate in education or skills programs with the consumer because of the urgency of his or her own concerns. Relatives may be confronting various stressors (for example, illness or job loss) that may have nothing to do with the consumer. Strain from serving in multiple roles and from difficult living circumstances (such as poverty or divorce) can all take their toll. In those situations, the relative should be referred for individual counseling, either concurrent with the family intervention or as a replacement for the family intervention for a specified period. It is also possible that at any stage the family may refuse participation. In that situation, family involvement could be revisited in the future or an alternate relative could be invited for involvement at the current time. In addition, if desired by the consumer, the family refusal could be addressed in discussions with ongoing treatment providers.
The sufficiency principle
The family services heuristic presented in
Figure 1 can be framed as a multilevel intervention that is based on the principle of sufficiency. Because consumers and their families have a range of needs and varying abilities to take advantage of family-based services, it is important to develop a range of services that permit delivery of the least intensive, most sufficient intervention. There are excellent models for this approach to intervention, notably the Triple P—Positive Parenting Program for childhood and adolescent behavioral problems (
31 ). Triple P is analogous to family psychoeducation in having begun as a complex, intensive intervention, well supported by empirical studies. The originators of Triple P, however, proceeded to develop a family of Triple P interventions, varying in intensity from a population-level, media-based information campaign, through targeted interventions focused on minor parenting concerns, up to a highly intensive enhanced version of the original program. Careful empirical evaluation of each version of Triple P has provided evidence for the effectiveness of the overall program (
32 ). A similar process of development and evaluation is now needed for the less intensive family interventions for consumers with severe mental illness (
Figure 1 ).
In summary:
• Efforts to implement family psychoeducation must be complemented by consideration of the larger universe of family services for severe psychiatric illnesses.
• A heuristic for working with families of persons with severe mental illness provides a match of interventions at varying levels of intensity, adjusted to family and consumer needs and circumstances.
• Careful empirical study is needed in the development of these less intensive family interventions to ensure that the needs of consumers and their family members are met with the most efficient and effective methods.
Measurement issues
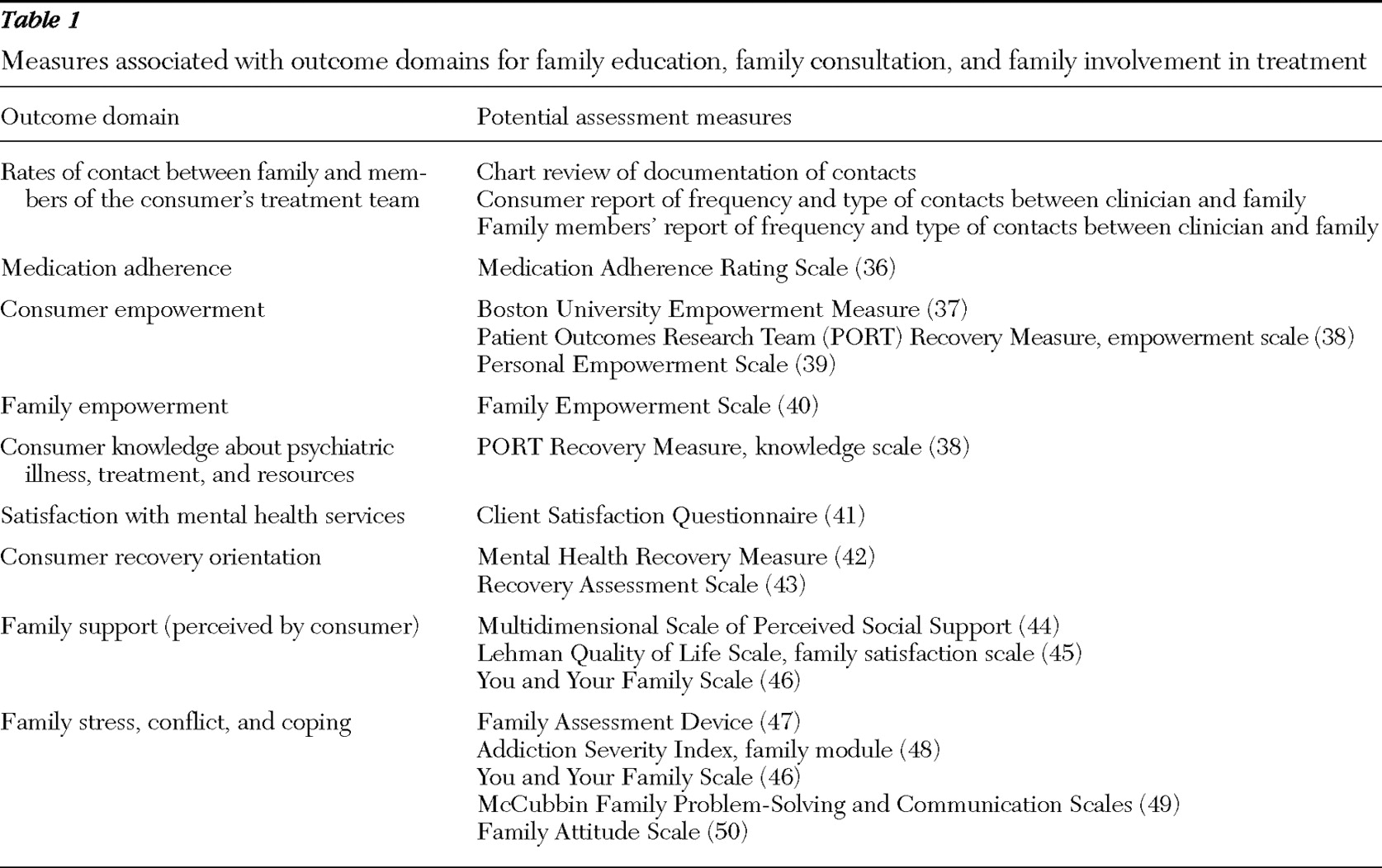
It is important to identify the expected outcomes of family involvement in care within each of the two broad program categories (less intensive family education and consultation and family psychoeducation). Published studies suggest that participation in general forms of family education, consultation, and involvement in treatment is associated with better adherence to treatment and to medications (
33,
34 ) and increased feelings of empowerment and hope and greater perceived illness knowledge by consumers (
35 ). Forum participants hypothesized that involvement in such programs could also be expected to result in greater rates of ongoing contact between family and the consumer's treatment team; increased empowerment for family members; increased knowledge about psychiatric illness, treatment, and resources for family members; increased satisfaction with the mental health services provided for consumers and their family members; an improved subjective recovery trajectory (such as perceived control and well-being) of the consumer participating in family-based services; enhanced perceptions of family support by consumers participating in family services; and improved coping and reduced stress and conflict among all involved family members. It is important to acknowledge that the measurement of many of these constructs (empowerment, knowledge, and recovery, for example) is a developing area of scientific inquiry.
Table 1 summarizes the existing measures suggested for assessing the major outcome domains (
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50 ).
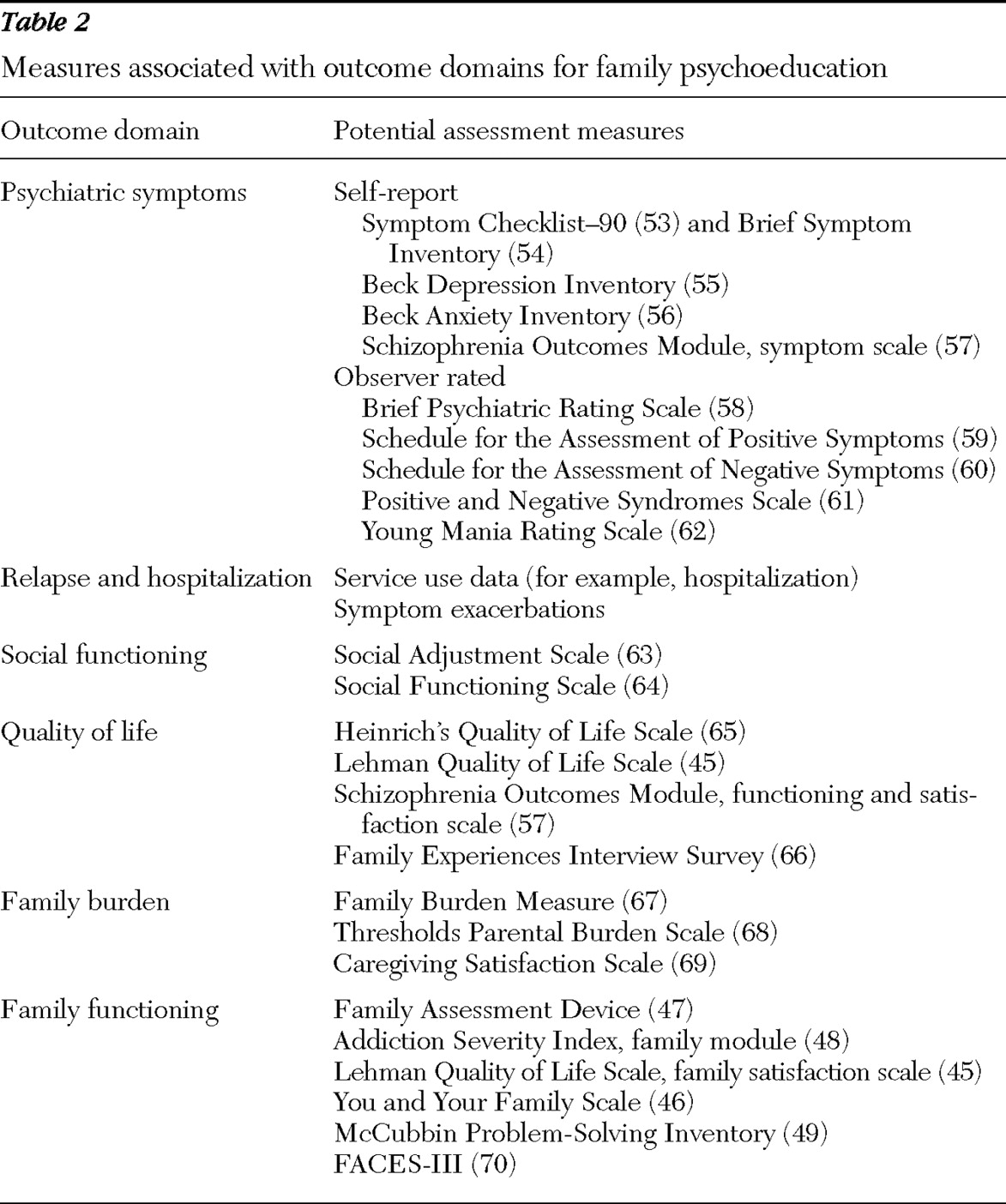
With regard to sustained participation in family psychoeducation, the existing literature on outcomes is more extensive, with a large body of randomized trials indicating that participation in family psychoeducation results in improved psychiatric symptoms (
2 ), reduced frequency of relapses and hospitalizations (
9 ), enhanced social functioning and quality of life, reduced family burden (
51 ), and improved family functioning (
52 ).
Table 2 summarizes measures to assess these outcome domains (
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70 ). Although initial family psychoeducation studies focused on measuring more clinically oriented outcomes (such as symptoms and relapses), forum participants agreed that the evaluation of family psychoeducation and family involvement in care should be broadened to incorporate a range of outcomes more directly relevant to recovery, such as empowerment, recovery orientation, community functioning, and consumer quality of life (see
Table 1 ).
Additional work is needed to better understand the impact of family interventions on family members by assessing constructs such as family members' level of burden and family functioning.
In summary:
• Outcomes that may be achieved through general forms of family education, consultation, and involvement in treatment will likely differ from those achievable through family psychoeducation.
• Given the considerable efforts under way to implement and conduct further research on family interventions for consumers with severe mental illness, there is a pressing need for experts in measurement to develop appropriate measures of the impact of family programs.
Discussion and conclusions
Providing optimal care to the population of individuals with severe mental illness requires provision of services to families. The failure to achieve even minimal family involvement in care, let alone the more intensive involvement required by family psychoeducation, raises concerns. This article outlines critical issues that must be addressed by the field if we are to expand the proportion of families served. In the simplest terms: we need to offer family psychoeducation to more families, and we need to develop an evidence base for complementary family services.
Implementing family psychoeducation is a challenge, and to maximize its offering we need to know the critical aspects, or mediators, of family psychoeducation models. If research could provide answers to these questions, and if the answers drove the refinement of interventions toward the greatest clinical flexibility, then wider implementation could be achieved. Key unaddressed issues in family psychoeducation implementation include the question of how (and whether) individual and group family interventions should be combined. Also, can groups be open, with rolling admission, or must they be closed to new participants once the group begins?
It is clear that successful implementation requires adequate resources to get the services up and running, to support the providers, and to provide appropriate referrals. Giving family psychoeducation its best chance at affecting a larger population requires considerable front-loading of investment and agencies or institutions that consider family services to be a top priority and a necessity in good clinical care. This is a challenge to agency administrators and clinical supervisors, as well as to funding agencies and institutions to provide this support.
Ideally, future family services research would fully disaggregate family psychoeducation manuals in order to randomly assign and study family psychoeducation elements (for example, group 1 gets family psychoeducation part A, group 2 gets family psychoeducation parts A and B, and group 3 gets family psychoeducation part B). Unfortunately, such studies would require a relatively large sample to be adequately powered and might be prohibitively expensive. However, there are investigations that could be informative. For example, studies that implement family psychoeducation could include a systematic qualitative analysis of the elements via interviews or focus groups with consumers and providers in order to elucidate critical elements of the family psychoeducation program. Future studies could also be hypothesis-driven theoretical studies of mediators in order to identify how family psychoeducation creates its effects. Either methodology could lead to the development of modified family psychoeducation models that incorporate the critical (presumably causative) components and permit flexibility with the remaining program components in order to further the penetration of family psychoeducation in the population.
There is an opportunity to improve family services by adopting a population-based approach that more fully addresses the needs of a range of consumers and families. A treatment heuristic such as the one presented in this article would facilitate the assignment of consumers and families to the least intensive intervention sufficient for their current needs and in doing so may optimize use of family psychoeducation while expanding complementary services. As complementary services to family psychoeducation are expanded and utilized, careful empirical study will be necessary.
Finally, there is a critical need to further develop and validate assessment instruments that will measure the intervention process and consumer and family outcomes. Measure development and validation will be necessary to properly assess the critical aspects of family psychoeducation and thereby optimize the models. Measure development is also critical for efficacy evaluations of complementary family services implemented. Measures will also be needed to access the efficiency and impact of the tiered treatment heuristic proposed.
A considerable list of challenges faces the family services research, academic, and administrative communities, but the time is ripe to expand the involvement of families in the care of individuals with severe mental illness.
Acknowledgments and disclosures
The authors report no competing interests.