As many as 21% of women will experience an episode of major depressive disorder in their lifetime, and up to 19% have significant depressive symptoms at some point during pregnancy (
1,
2 ). Unfortunately, depressive symptoms of pregnant women often go unrecognized and untreated (
3,
4 ) even though women are seen by medical providers on numerous occasions for prenatal care.
To address problems with detection and treatment of depression, many advocate screening in obstetrical settings (
5,
6 ). Despite the plausibility of this approach, studies from other general health care settings do not generally show that patient outcomes improve as a result of screening (
7,
8 ). In its summary, the U.S. Preventive Services Task Force recommended screening for depression only if further diagnostic and treatment procedures are in place to follow up on screening results (
9 ). To our knowledge, the one study that specifically addressed screening perinatal women for depression (
10,
11 ) found that it led to higher detection and treatment rates. Of note is that the women in this cohort had incomes and education levels that were above the national average, and procedures took place in a large multispecialty health care group that had resources for mental health care. It is not clear whether screening would be as effective in more diverse health care settings, including those that provide reproductive health services to less advantaged women, many of whom have public insurance or are uninsured.
Aside from the reduction of maternal morbidity, the detection of depressive symptoms of pregnant women may benefit their offspring. Several (
12,
13,
14 ) but not all (
15 ) researchers have found that high levels of depressive symptoms are associated with preterm or low-birth-weight delivery. Babies born preterm or of low birth weight have high rates of morbidity and mortality; therefore, reducing mothers' depressive symptoms may improve both maternal and fetal outcomes (
16 ). The goal of the federal Healthy Start depression initiative, funded by the Health Resources and Services Administration of the U.S. Department of Health and Human Services, is to reduce infant mortality by improving maternal and infant health outcomes. This program, which was started in 1991, stipulated screening for depression as part of its mandate during the funding period of 2001–2004 (
17 ). Grantees were also instructed to develop programs to educate clinicians, paraprofessionals, and the general public about depression during pregnancy and the postpartum period.
In this article, we present an evaluation of the New Haven Healthy Start (NHHS) depression initiative and assess whether it likely resulted in decreased rates of depressive symptoms among pregnant and postpartum women. Future reports will assess the influence of this program on birth outcomes. We addressed the following specific questions in our study: Did the severity of depressive symptoms among pregnant and postpartum women in participating clinics decrease in cohorts served after, compared with before, deployment of the NHHS depression initiative? Among women not already in treatment but with elevated rates of depressive symptoms, did the specific rates of depression recognition and treatment improve after versus before the deployment of the NHHS depression initiative? Did NHHS enrollees and nonenrollees differ on severity of depressive symptoms at follow-up? Was there a positive effect of the program on rates of detection, referral, and treatment?
Methods
New Haven Healthy Start procedures for participants
Women were eligible to participate in NHHS if they lived in the New Haven area, were pregnant or within six months of delivery, received health care at a publicly funded hospital or clinic, or were referred to the program through a community outreach worker. There were no age or language restrictions. All women who participated in the program provided written informed consent. Given the nature of women who seek services at this hospital and community clinics, this was a predominantly low-income group.
Women could enroll after they were approached by NHHS workers at health care appointments, if they responded to a program advertisement on television or in print, or if they were referred by a health care or social service provider.
Women enrolling in NHHS were administered a standardized risk assessment that included questions regarding general medical and obstetrical problems, the Primary Care Evaluation of Mental Disorders (PRIME-MD) Brief Patient Health Questionnaire (BHQ) (
18,
19 ) to determine whether an individual had a probable depressive disorder or panic disorder, the PTSD Symptom Scale (
20 ), a five-item modification of the Conflict Tactics Scale (
21,
22 ) to identify interpersonal violence, and questions regarding alcohol and illicit substances. Finally, women were asked if they desired help for an emotional problem or mental illness.
New Haven Healthy Start procedures for providers
Participants were deemed in need of mental health services if they screened positive for a mood or anxiety disorder, were subjected to interpersonal violence, endorsed hazardous substance use, or requested mental health services. An NHHS worker provided participants linkage to concrete services; in addition their assessment was faxed to a confidential helpline (MOMsline) for follow-up by a master's-level clinical social worker, who conducted a diagnostic assessment. On the basis of the assessment, each participant who screened positive was triaged to immediate care or to a treatment referral. All women who requested or required a treatment referral were given the names and numbers of at least two providers. In addition, the program offered weekly drop-in services that provided behavioral services, pharmacological services, or both to English- and Spanish-speaking participants. Participants were contacted again after one, three, and six months, and additional referrals were given, if necessary. [A diagram showing the recruitment and follow-up process is available as an online supplement to this article at
ps.psychiatryonline.org .]
During the project period, educational and training seminars were run for health care clinicians and NHHS care coordinators. Topics included general education on perinatal depression; technical assistance for using the helpline and NHHS referral procedures; behavioral health treatment options for pregnant and postpartum women; and assessment guidance for suicide, posttraumatic stress disorder (PTSD), and trauma.
Evaluation procedures
Because this was not a randomized study, we used two comparison groups to estimate the effects of the program. These groups shared characteristics of the women enrolled in NHHS and were drawn from the same reproductive health settings. The first comparison group included women who received reproductive health services before the NHHS depression initiative began. Because education of clinic workers and providers could contribute to a cohort effect, we also included a second comparison group composed of women not enrolled in the NHHS program. Reasons for not enrolling included lack of interest in participation from the potential enrollee and unavailability of an NHHS worker at the woman's health visit. Evaluation of all three cohorts—the pre-NHHS depression initiative cohort (group 1) and, postinitiative, the cohort enrolled in NHHS (group 2) and the cohort not enrolled in NHHS (group 3)—was conducted by an independent evaluation team.
The evaluation team assessed group 1 within the six-month period before the NHHS depression initiative began (November 2001). Assessment of groups 2 and 3 was concurrent (April 2002 to April 2005) and began after the NHHS depression initiative was implemented. Evaluators attempted to screen participants at least twice, with a three-month interval. Institutional review board approval was obtained at participating sites.
The independent evaluators were trained social workers with education ranging from bachelor's to master's degrees. They obtained written informed consent from participants and administered a structured questionnaire that asked questions about psychiatric history and current or past mental health treatment. The PRIME-MD was used to determine probable depressive or anxiety disorders (
23 ). The BHQ depression module from the PRIME-MD yields a dimensional measure of depression as well as a diagnostic indicator of probable depression. The PTSD Symptom Scale (
20 ) was used to identify probable PTSD. All questionnaires were administered before patients saw their health care providers. After their health care visit, participants were asked whether their provider had discussed or initiated a mental health treatment referral. Finally, participants' medical records were reviewed with a standardized abstraction form to identify clinician documentation of psychiatric illness or treatment.
Statistical analysis
Because women were not randomly assigned to any of the aforementioned groups, the observed covariates were not balanced across compared groups. To correct for this we used a propensity scoring method (
24 ). The propensity score is obtained as the conditional probability of being in the experimental group versus the comparison group and was divided into quintiles. Covariates in the propensity score adjustment included age, gestational week, parity (number of live births), race and ethnicity, past depression (yes or no), comorbid diagnosis (yes or no), site, baseline BHQ score, interpersonal violence (yes or no) and suicidal thoughts (yes or no). Our dependent variable was change in depressive symptoms according to the BHQ depression module (
18,
19 ).
Within each quintile (stratum), groups were compared for improvement according to the BHQ score. To assess whether changes likely resulted from a period effect (group 1, the pre-NHHS depression initiative cohort, versus groups 2 and 3, postinitiative) or participation in NHHS (group 2, which participated, versus group 3, which did not participate), we used linear mixed-effects models to estimate differences over time. The covariates in the final models included the group indicator, linear time in months, propensity score quintile, and the interaction term of group by time. In the model comparing group 1 with combined groups 2 and 3, if the indicator for the combined groups by time was negative and statistically significant ( α =.05), we concluded that women in the post-NHHS period had greater improvement in depressive symptoms than those in the pre-NHHS period. In the model comparing outcomes between groups 2 and 3, if the interaction term for group 2 by time was negative and statistically significant ( α =.05), then it indicated that women enrolled in the NHHS program had greater improvement in depressive symptoms than women not enrolled in NHHS. Because many women were asymptomatic and hence would neither be appropriate for nor benefit from an intervention, these analyses were repeated after inclusion of only those participants who were not in treatment and scored at least a 10 (indicating at least moderate severity of depressive symptoms) on the BHQ.
In order to explore whether diagnosis, referral, or treatment differed among groups, we compared rates with the chi square statistic, without propensity score adjustment. These comparisons were restricted to women who had a BHQ score of at least 10 and were not already in receipt of mental health care.
Results
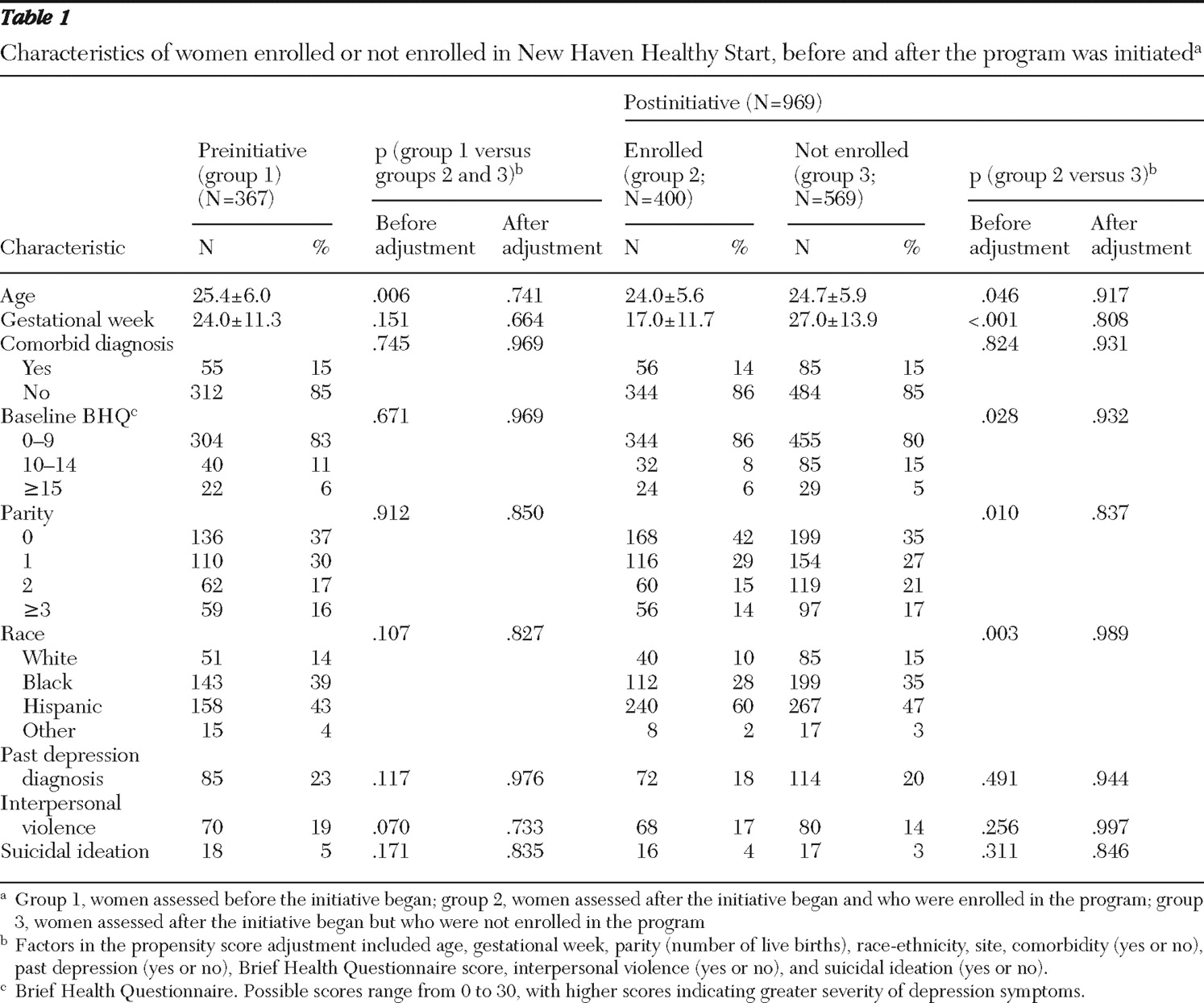
The women's baseline characteristics and depression outcomes are presented in
Table 1 . The 367 women in group 1 (preinitiative) were significantly older and had a trend toward a greater frequency of interpersonal violence than the combined groups 2 and 3 (400 and 569 women, respectively). Unadjusted comparisons between groups 2 and 3 indicated significant differences in age, parity, gestational week, race and ethnicity, and baseline BHQ score. Differences between these groups were no longer significant after propensity score adjustment.
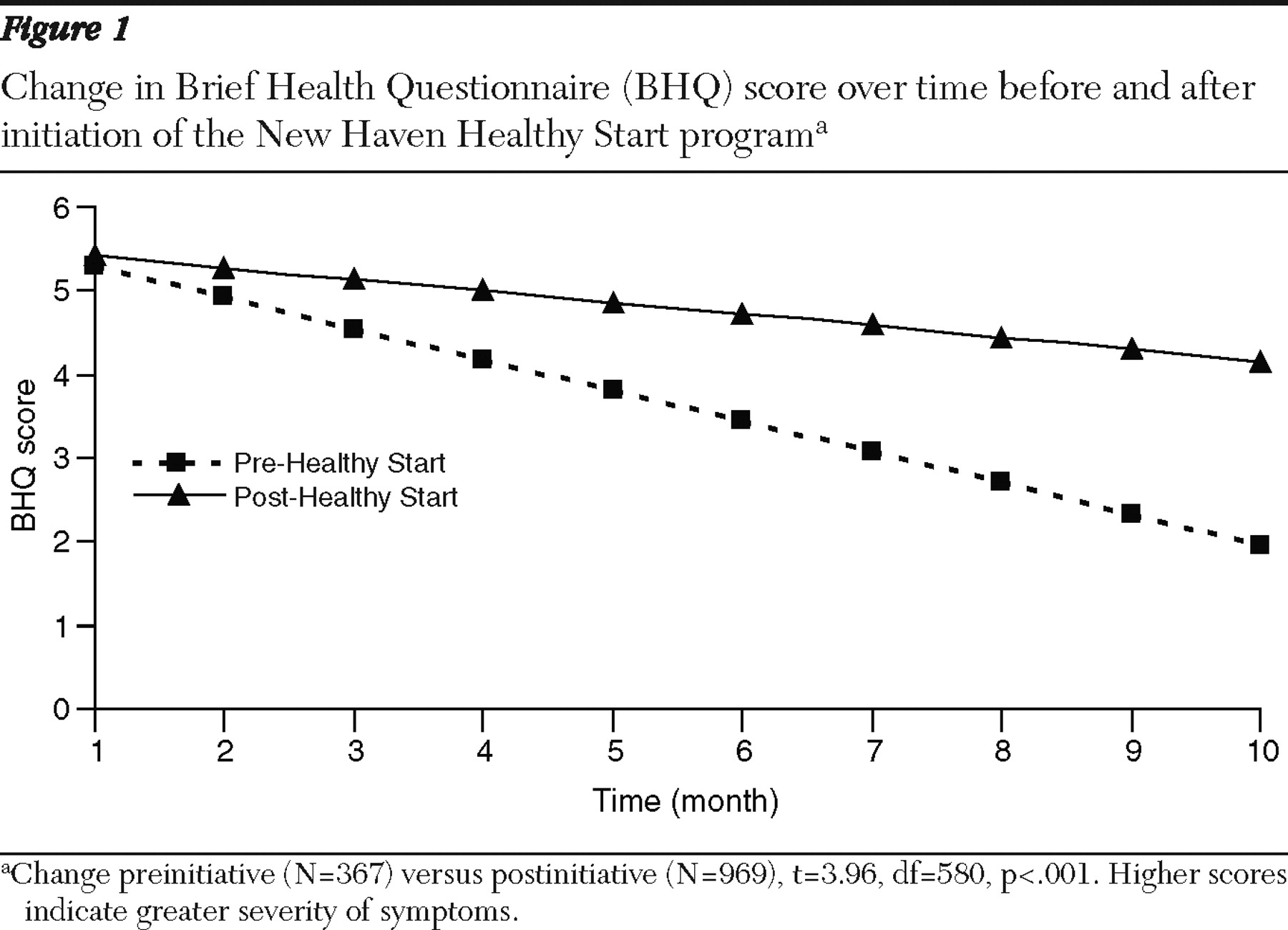
There was improvement over time when all groups were combined (decrease in BHQ score of .17±.02 points; t=–8.23, df=1,016, p<.001). However, the improvement was largely in group 1 (see
Figure 1 ). The monthly difference in BHQ scores in combined groups 2 and 3 was slightly but significantly more positive (BHQ difference=.23±.06; t=3.96, df=580, p<.001) than in group 1, indicating that there was no greater improvement in depressive symptoms after implementation of NHHS. In the analysis of women with a score of at least 10 at baseline, both the pre- and post-NHHS cohorts improved over time by 1.00±.08 points on the BHQ (t=-11.88, df=140, p=.01).
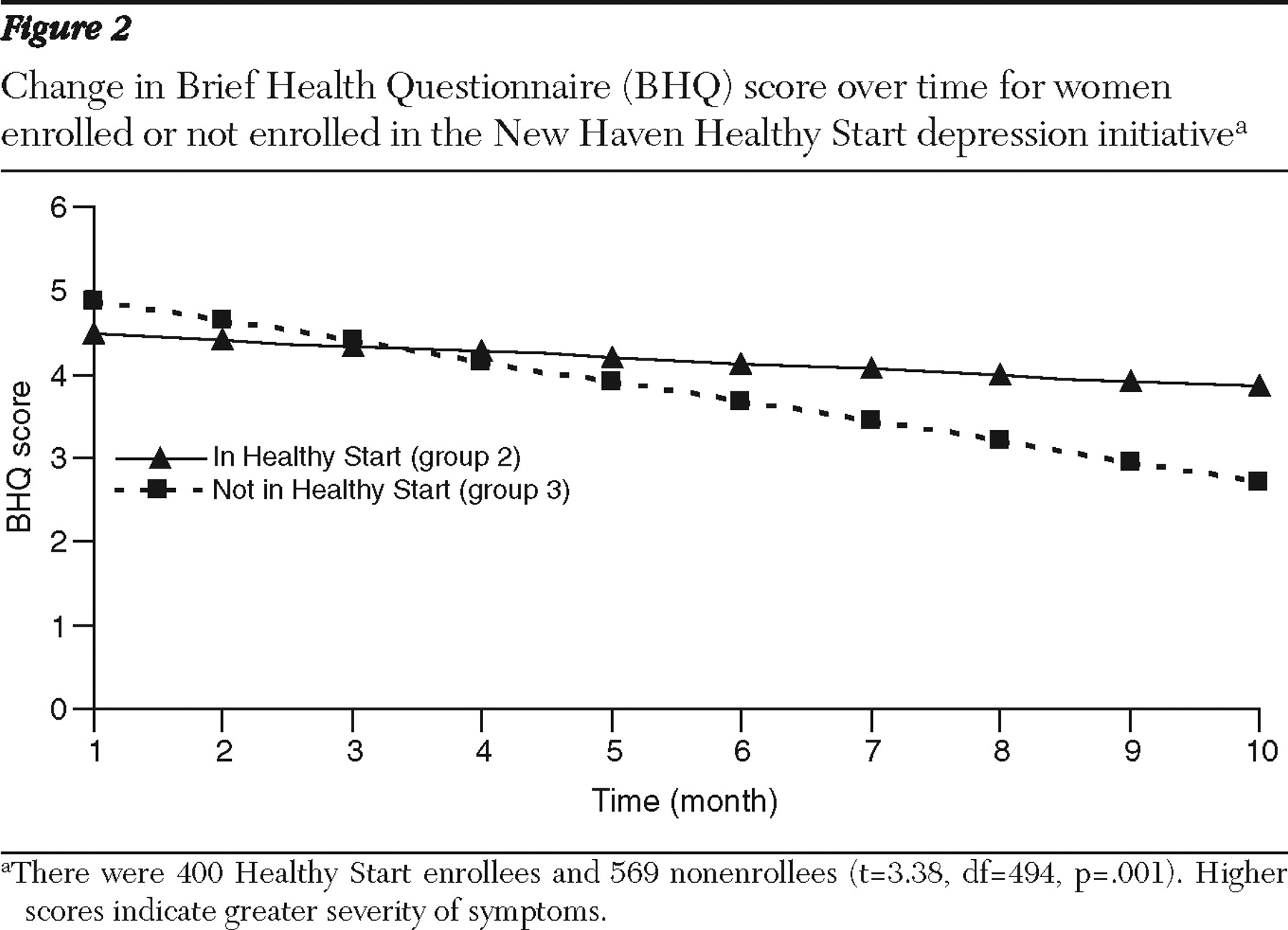
Effect of NHHS participation on depression outcome
Women in the combined postinitiative group (groups 2 and 3) had small but significant improvement in BHQ scores over time (change of .14±.02 points; t=-6.10, df=722, p<.01) (data available on request). However, group 2 (enrolled in NHHS) showed significantly less improvement than did group 3 (
Figure 2 ). The monthly BHQ score was .16±.05 points higher (t=3.38, df=494, p=.001) each month in group 2 compared with group 3, indicating no benefit of NHHS participation. In the analysis of women with a score of at least 10 at baseline, the combined groups improved over time by .92±.09 points on the BHQ (t=-9.91, df=106, p<.001), but there was no significant difference between groups.
Rates of depression diagnosis, referral, and treatment
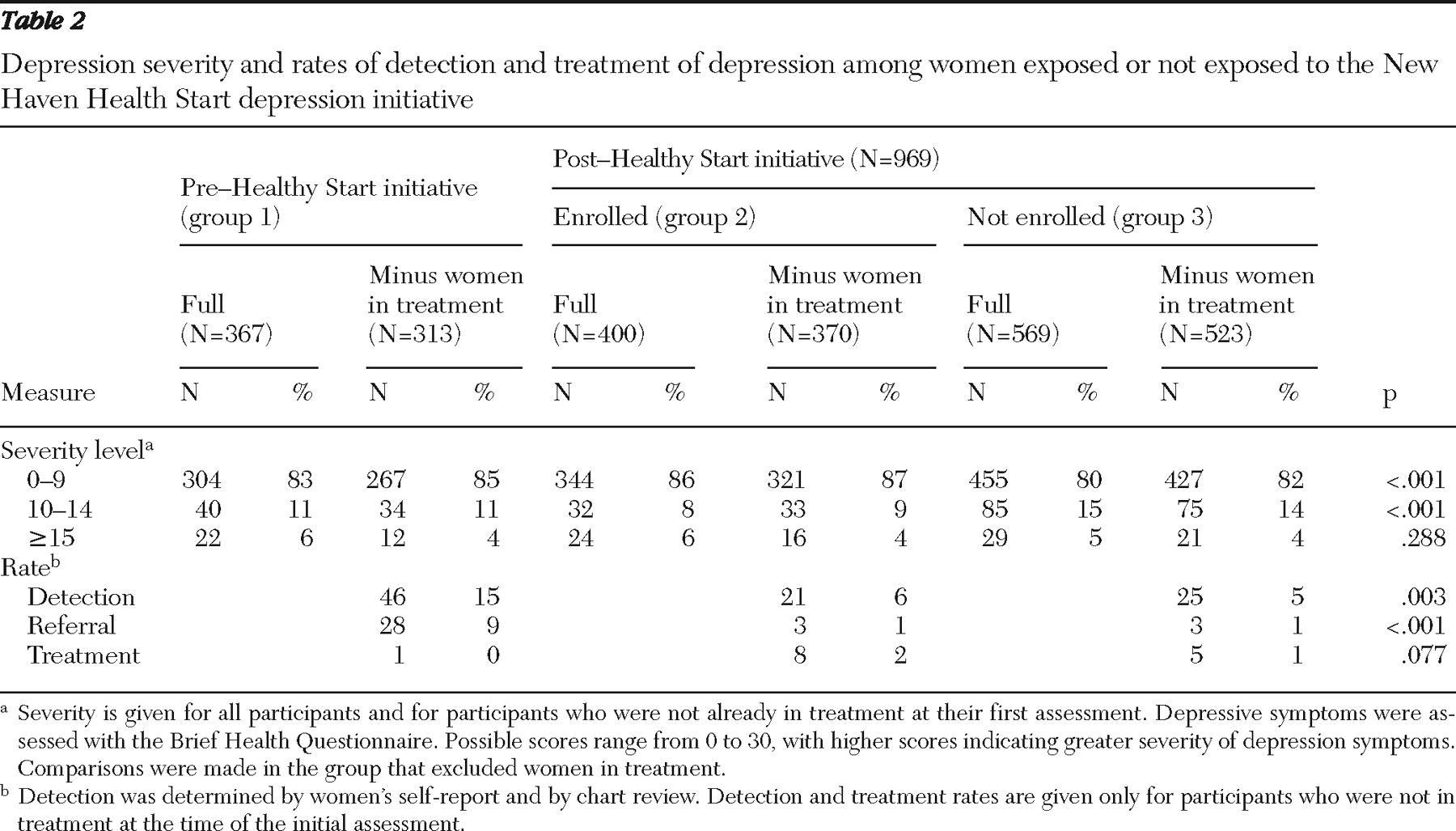
The severity of illness and rates of detection, clinician referral, and treatment for the three groups are presented in
Table 2 . Of those not in treatment 15%, 13%, and 18% from groups 1, 2 and 3, respectively, had BHQ scores that were at least 10. Rates of detection (
χ =11.76, df=2, p=.003) and referral (
χ =36.76, df=2, p<.001) by the obstetrical provider to mental health services differed significantly between the three groups, with the highest rates in group 1. Treatment rates did not differ significantly.
Discussion
This study found no evidence to support independent depression screening and referral among perinatal women in publicly funded clinics. In the first set of analyses, we examined whether a program that included provider education, community awareness, and direct systematic depression screening by an individual who was not the health care provider diminished the rates of depressive symptoms among pregnant and postpartum women. In contrast to our expectations, the rates of depression diminished significantly less after, than before, the program was initiated. Although this difference was significant, the differential of .23 point on the BHQ between the two groups is not likely of clinical significance. Moreover, outcomes for the group in greatest need, those with a BHQ score of at least 10, did not differ significantly. In the second set of analyses, we examined whether actual participation in the NHHS program led to decreased depressive symptoms. Neither overall participants in the NHHS program nor those who were most symptomatic and enrolled in NHHS had significantly greater improvement in depressive symptoms compared with women who were not enrolled in NHHS.
Our third set of analyses showed that detection and clinician referral to specialty mental health care was lower after than before initiation of the NHHS program. Although the NHHS depression initiative sought to strengthen the therapeutic role of the obstetrical provider in intervening on depression, the addition of NHHS workers on site may have been viewed by health care providers as replacing their need to detect symptoms and refer women. This may have resulted in a more fragmented system in which busy providers felt that detection and treatment referral for mental health issues was addressed by support staff. This theory is congruent with work demonstrating that the addition of mental health workers on site may reduce detection, referral, and treatment by primary care providers because of providers' abdication of these responsibilities to the mental health specialists (
25,
26 ). The fragmented process of detection and care may be why our results differ markedly from those of Georgiopoulos and colleagues (
10 ), who found benefits for screening postpartum women. In their study, many women were treated for depressive symptoms on site by an obstetrical provider. Nearly one-half were prescribed an antidepressant, which may be more acceptable among postpartum women than pregnant women.
Our results are in accord with the meta-analysis by Gilbody and colleagues (
8 ), who found that depression screening changed neither levels of depressive symptoms nor the use of depression treatment in unselected populations. Our intervention had additional components that included general education of the community and practitioners and a system in place to offer care to those who screened positive for depressive symptoms. The U.S. Preventive Services Task Force (
9 ) suggested that screening is more likely to diminish the burden of depression if there are procedures in place to care for patients with depressive symptoms. Even the availability of treatment resources did not enhance the effectiveness of depression screening. However, we did not have the kind of rigorous on-site depression treatment that has promoted successful treatment of depression in other primary care settings (
27,
28,
29 ).
Our inability to show that the NHHS program improved depression may have been hampered by issues unique to our patient cohort. First, providers may be reluctant to initiate—and pregnant patients may be less likely to accept—treatment on site because this usually indicates pharmacological treatment. Referrals to specialty mental health care meant that patients needed additional motivation to schedule and follow up with appointments or attend appointments off-site during drop-in hours.
Second, there were substantial differences in the groups at baseline. Although propensity score adjustment should have equalized possible confounding factors, there may have been residual confounding or other differences related to improvement in depressive symptoms for which there was not adequate adjustment.
Third, the lack of effect of the NHHS initiative also may have been due to a relatively low rate of treatment need. A score of 10–15 points on the BHQ indicates only a mild degree of depression and was found in 13%–18% of women in these groups. In this cohort of underprivileged women, we may have identified women who were in distress because of a host of psychosocial issues, including unstable housing, scarcity of food, and concerns about neighborhood violence and crime. A more clinically meaningful score of >15 was endorsed by 5%–6% of women in each group, but some of those women were already in treatment. Thus, even though our cohort was large, the actual small numbers of women who needed treatment may have limited power of the analyses to detect differences.
Other investigators have found that despite thoughtful procedures and enthusiastic community interest, community-based interventions frequently do not show demonstrable clinical benefits (
30 ). Reasons for this include failure to measure behavioral change for a sufficient period, weak interventions, or difficulties in providing the intervention to those who need it the most (
30 ). The NHHS depression initiative provided robust treatment resources (flexible appointment times and multiple referrals). However, a stronger focus on treatment engagement or on-site treatment resources may have been needed.
Finally, it may be that women in the greatest need of treatment had already been identified. This is not likely, however, because our previous work has shown that only about one-quarter of women with a mood or anxiety disorder, including 12% with suicidal ideation, were detected by a prenatal care provider in these publicly funded prenatal care settings (
3 ).
Conclusions
In summary, systematic screening and treatment referral did not reduce the overall rates of depressive symptoms of perinatal women. Given these findings, the mandatory inclusion of these procedures in the Healthy Start program must be questioned. It may be that on-site treatment resources, if made available, or an intervention that focuses on engagement would improve results, but this hypothesis would require further evaluation. Other research conducted by our group with a low-income population of perinatal women demonstrated that women were more than four times more likely to attend a behavioral health treatment visit if the provider was located at the same site as their obstetrical provider. Future work should consider conjoint care by providing mental health services on site in reproductive health care settings.
Acknowledgments and disclosures
This study was supported by grant 5-R0-HD045735 from the National Institute of Child Health and Human Development, grants MH-01908-04 and T32-MH014235 from the National Institute of Mental Health (NIMH), and grant 1H78MC00028-01 from the Health Resources and Services Administration of the Department of Health and Human Services.
Dr. Yonkers received an investigator-initiated research grant from Eli Lilly and Company. She received medication from Pfizer to conduct an NIMH trial and received royalties from Up to Date. The other authors report no competing interests.