Nonpharmacologic methods for alleviating depression have recently garnered renewed attention (
1,
2). ECT is the most effective nonpharmacologic treatment of depression (
3). Although the mechanisms of antidepressant action of ECT are unknown, recent data indicate that production of a generalized convulsion alone is not sufficient for treating depression; the effect of the ECT seizure on regional brain function is also important in determining therapeutic benefit (
4,
5). These data are consistent with evidence from functional neuroimaging studies that have implicated prefrontal, temporal, and limbic structures in depression (for review see reference 6).
Transcranial magnetic stimulation has been developed as a new tool to explore brain-behavior relationships noninvasively for potential therapeutic applications (
7). First developed by neurophysiologists and neurologists, transcranial magnetic stimulation involves placing a small but powerful electromagnet on the scalp, which causes cortical neurons just below the skull to depolarize in response to the electrical current generated in them by rapid oscillations in the magnetic field. This technology can map regional brain function (
8) and temporarily alleviate the bradykinesia of Parkinson's disease (
9). A single magnetic pulse, which typically generates a field of approximately 1.5 tesla 1–2 cm below the coil, will cause a cluster of neurons to discharge. Repetitive pulses (repetitive transcranial magnetic stimulation) can cause neurons to repeatedly discharge (
10). At high frequencies, these neurons may be unavailable for communication with other brain regions, in effect creating a temporary “functional deficit” (
11). For example, repetitive transcranial magnetic stimulation over temporal cortex blocks speech production (
12), stimulation over left dorsolateral prefrontal cortex impairs working memory (
13), and repetitive transcranial magnetic stimulation over the occipital cortex causes visual field defects (
14).
Several groups have begun investigating whether transcranial magnetic stimulation or repetitive transcranial magnetic stimulation might have antidepressant activity (
15–
19). Preliminary animal evidence suggests that repetitive transcranial magnetic stimulation is similar to electroconvulsive shock in animal models of depression (
20) and that it down-regulates beta receptors (
21) and produces changes in brain monoamine concentrations (
22). We initially employed repetitive transcranial magnetic stimulation over the left prefrontal cortex in six subjects with treatment-refractory depression in an open study and found modest group effects but robust individual responses in two of six patients (
18). This initial study was promising yet inconclusive because of its open design and small study group size. We designed and carried out the following placebo-controlled crossover study to test the hypothesis that daily left prefrontal repetitive transcranial magnetic stimulation has antidepressant effects.
METHOD
We enrolled 12 right-handed outpatients from the Washington, D.C., area (11 women) (mean age=41.8 years, SD=12.4). Subjects were recruited through local advertisements and were not paid. Structured interviews used for screening were the Schedule for Affective Disorders and Schizophrenia—Lifetime Version Modified for the Study of Anxiety Disorders (
23) and the Structured Clinical Interview for DSM-IV (
24). Subjects were also screened with a thorough general and neurological examination, a urine drug screen, an HIV test, and a magnetic resonance imaging (MRI) scan of the head. Patients with abnormalities on any of these measures, as well as patients with pacemakers or a history of seizures or major head trauma, were excluded. All subjects met DSM-IV criteria for current major depressive disorder; 11 subjects had recurrent unipolar depression, and one was diagnosed with bipolar II disorder. The mean score on the 21-item Hamilton Depression Rating Scale (
25) at entry was 28.5 (SD=4.2).
After complete description of the study to subjects, written informed consent was obtained through a protocol approved by the National Institute of Mental Health institutional review board. The antidepressant medication regimens of nine subjects were tapered. Three subjects had experienced a partial response to a 10-week, stable-dose antidepressant trial. The regimens (venlafaxine, 25 mg/day; venlafaxine, 200 mg/day; and nefazadone, 200 mg/day) were continued in order to not risk a worsening of depression, which would confound the interpretation of the effect of repetitive transcranial magnetic stimulation or sham treatment.
Magnetic stimulation was performed by using a high-speed magnetic stimulator (Cadwell, Inc., Kennewick, Wash.). On the initial visit, the motor threshold of the right abductor pollicis brevis muscle (the thumb) for the subjects was determined by using the method of limits as previously described (
11,
26). For the remainder of the study, the subjects then received stimulation at 80% of this level. Each weekday the subjects received 20 2-second, 20-Hz stimulations over 20 minutes (800 pulses per session, 10 sessions per treatment phase, total of 20 sessions overall per subject). Stimulation occurred over the left dorsolateral prefrontal cortex, which was defined for each person as the site 5 cm anterior and in a parasagittal plane from the point of maximum stimulation of the right abductor pollicis brevis muscle. We used a figure 8-shaped water-cooled coil, with the extensions of the coil perpendicular to a line running from the site to the subject's nose.
Sham stimulation occurred in exactly the same manner as active repetitive transcranial magnetic stimulation, except that the angle of the coil, rather than being tangential to the skull, was at 45 degrees off of the skull. This produces a similar sensation in the scalp but appears not to stimulate the brain, since such angled stimulation when applied over motor cortex is ineffective in producing a motor evoked potential and does not produce changes in [
18F]fluorodeoxyglucose positron emission tomography (
27).
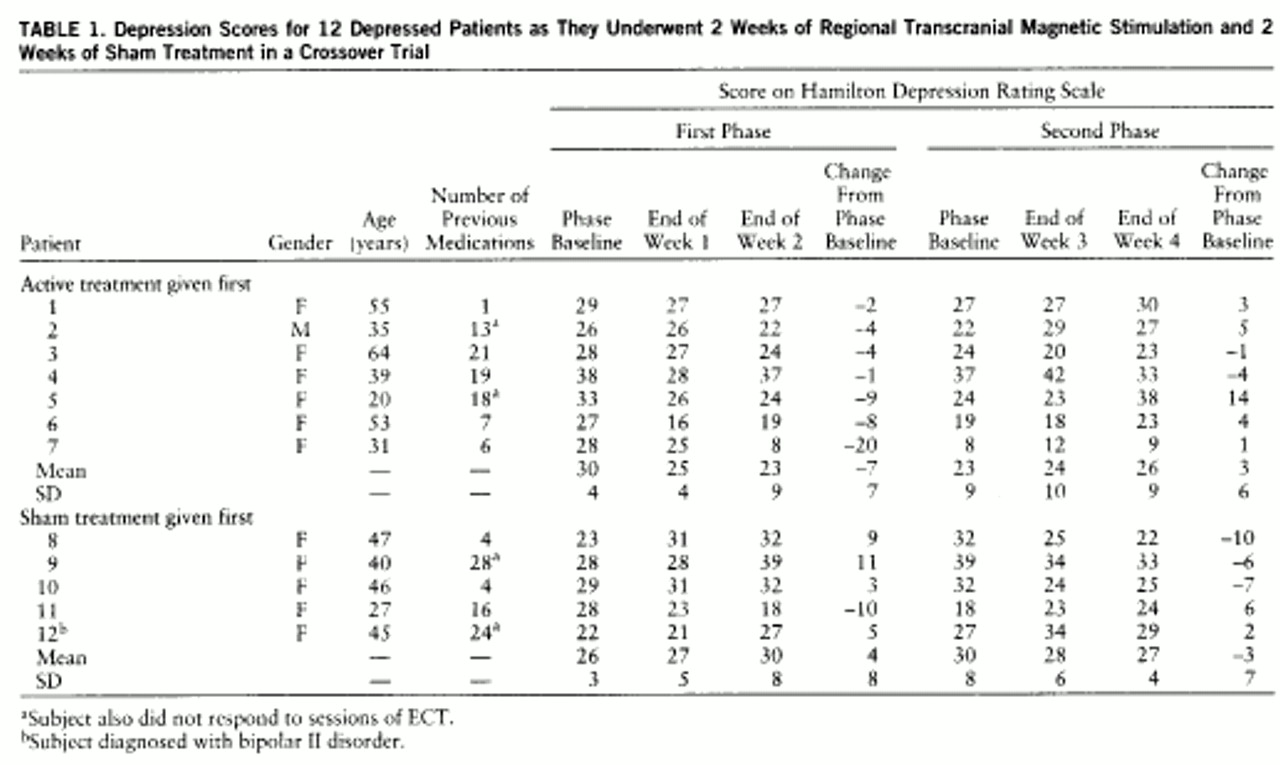
Patients were selected at random to initially receive either placebo or active daily repetitive transcranial magnetic stimulation. Seven patients with a mean Hamilton depression scale score of 30.0 (SD=4.1) initially received active repetitive transcranial magnetic stimulation; five patients with a mean Hamilton depression scale score of 26.4 (SD=3.7) initially received the sham procedure. Subjects were serially rated (at phase baseline and at the end of each week) with the 21-item Hamilton depression scale by trained investigators who were blind to the treatment phase. Hamilton depression scale scores were analyzed as change from the relevant phase baseline (active, sham) by using repeated measures analysis of variance (ANOVA) with order (sham-active versus active-sham) as a between-subjects term and treatment (sham versus active conditions) and time (weeks 1 and 2) as within-subject factors.
RESULTS
All subjects enrolled completed the study with no unexpected side effects (
table 1). Four subjects reported the occurrence of mild headaches, from immediately after to 3 hours after active treatment, that were relieved by acetaminophen. No subjects reported problems with memory or attention. There were no seizures (a possible adverse effect of repetitive transcranial magnetic stimulation).
One subject who initially received sham treatment significantly worsened over the first 10 days of the sham stimulation, stopped going to work, and became actively suicidal. She was deemed capable of providing continued informed consent, and she chose to advance to the next phase (active). She clinically improved over the next 2 weeks and was no longer actively suicidal, although she only returned to her entry level of depression.
A repeated measures ANOVA of changes in Hamilton depression scale scores from relevant phase baseline, with order (sham-active versus active-sham) as a between-subjects term and treatment (sham versus active conditions) and time (weeks 1 and 2) as within-subject factors, found no significant effect for order (F=1.2, df=1,10, p<0.30) or time (F=0.25, df=1,10, p<0.60). During the active phase, mean Hamilton scores decreased by 5.25 points, and during the placebo phase they increased by 3.33 points. This treatment effect was statistically significant (F=6.02, df=1,10, p<0.03).
DISCUSSION
This study confirms the hypothesis that daily left prefrontal repetitive transcranial magnetic stimulation (20 Hz at 80% motor threshold) for 10 days over 2 weeks has an antidepressant effect in a group of mainly unipolar depressed outpatients. We have also demonstrated that repetitive transcranial magnetic stimulation can be safely used in outpatient studies of depression.
Although our findings were statistically significant, there were numerous limitations to this study. It was only designed to test whether repetitive transcranial magnetic stimulation in this population, at these stimulation parameters, and for a limited duration of treatment, would have more robust antidepressant effects than sham treatment. Our study was not a naturalistic “clinical” trial that occurred over 4–6 weeks such as those seen in most antidepressant and ECT studies. However, when several patients from this study openly received additional repetitive transcranial magnetic stimulation at the same parameters after completion of the blind study, further clinical improvement was noted. It also should be noted that, although patients and raters were blind, the physician who administered the repetitive transcranial magnetic stimulation was not, which leaves open the possibility of biasing the results. Future studies may consider the use of a head-holder or other measures to minimize interaction between subjects and clinicians who know the treatment phase of the patient.
The site of stimulation was functionally defined for each person on the basis of the location of motor cortex in that subject. It is likely that we have stimulated slightly different regions of the prefrontal cortex. Future studies might consider the use of MRI-guided stimulation to control for differences in brain morphology and skull size and thickness (
28), as well as explorations of other measures. Finally, this study was largely composed of women, and although we are not aware of a differential response by gender, such a phenomenon is possible and thereby limits the ability to generalize from these results.
Despite these limitations, this placebo-controlled study demonstrated an antidepressant effect of left prefrontal active repetitive transcranial magnetic stimulation versus sham treatment. This builds on previous open studies with transcranial magnetic stimulation (
15–
17) and repetitive transcranial magnetic stimulation (
18) in patients with treatment-refractory depression. In a recently published double-blind study that was carried out while this study was ongoing, Pascual-Leone and colleagues (
19) demonstrated, with slightly “stronger” stimuli (20 10-second, 10-Hz stimulations at 90% motor threshold or a total of 2000 stimuli per day), that daily left but not right prefrontal repetitive transcranial magnetic stimulation had antidepressant properties in 11 of 17 severely depressed patients.
These treatment studies follow in the path of new information gleaned from functional neuroimaging studies, which have most often implicated the prefrontal and temporal cortex as dysfunctional in depression, with normal function returning after clinical recovery (
4,
29). In contrast, in nondepressed healthy volunteers, studies of the acute effect of repetitive transcranial magnetic stimulation on mood have found that left prefrontal repetitive transcranial magnetic stimulation causes subtle increases in self-rated sadness, while right prefrontal stimulation resulted in greater happiness (
30–
32). This lateralized effect on mood was also seen in a repetitive transcranial magnetic stimulation study in nondepressed patients with obsessive-compulsive disorder, which demonstrated that right prefrontal repetitive transcranial magnetic stimulation decreased compulsive urges and also improved mood (
33).
This reversal in hemispheric effects of repetitive transcranial magnetic stimulation on mood in studies of nondepressed comparison subjects and clinically depressed patients is intriguing (
34). It has been hypothesized that the prefrontal cortex acts in a regulatory manner on underlying limbic structures, which directly determine mood and may be different in depressed patients and in healthy subjects (
6,
35–
38). These data suggest the possibility that depression involves not only a relative prefrontal hypofunction but a qualitative change in relative hemispheric modulation of mood.
The mechanisms that underlie the antidepressant effect of repetitive transcranial magnetic stimulation are unknown. It appears that repetitive transcranial magnetic stimulation does not induce “silent” focal seizures, since previous studies in healthy subjects at these parameters showed no change in serum prolactin (
31) or in surface EEG activity recorded before and after stimulation (
26). We also reason that because of the known rapid drop-off in magnetic field intensity as a function of distance from the coil, we are only directly stimulating neurons immediately beneath the coil at the surface of the cortex (
28,
39). Previous studies have demonstrated that repetitive transcranial magnetic stimulation at similar parameters over the prefrontal cortex results in increases in serum thyroid-stimulating hormone, which suggests the possibility of increases in thyrotropin-releasing hormone and an indirect effect of repetitive transcranial magnetic stimulation on hypothalamo-pituitary structures (
31). Functional neuroimaging studies and somatosensory evoked responses have demonstrated that prefrontal repetitive transcranial magnetic stimulation has effects at brain regions remote from the site of stimulation, presumably through transsynaptic signaling (
18,
27,
40). Of note, a recent SPECT study in healthy adults that used left prefrontal repetitive transcranial magnetic stimulation at parameters identical to those in this study demonstrated that compared to baseline, there was reduced blood flow at the coil site and in the anterior cingulate during stimulation, with increases in brainstem activity (
40). Future studies that combine neuroimaging with regional stimulation will likely be very helpful in clarifying neurobiological effects of repetitive transcranial magnetic stimulation (
41).
CONCLUSIONS
Daily left prefrontal repetitive transcranial magnetic stimulation over a 2-week period had an antidepressant effect in outpatient depressed patients that was superior to sham stimulation. Further studies appear warranted to examine which of the many variables used in this study are crucial to this antidepressant effect (location, intensity, frequency, train length, intertrain interval, dosing schedule, and length of treatment) and which, if any, can be optimized to induce more robust effects. Until this effect is further replicated and these technical and methodological issues are clarified, it is unclear what role repetitive transcranial magnetic stimulation might have in the clinical management of depression. Regardless of its potential clinical role in the treatment of depression, further repetitive transcranial magnetic stimulation work will likely provide important information about the neuroanatomical structures and pathophysiological mechanisms that are important in mood regulation.