Immunological mechanisms may be involved in the pathophysiology of schizophrenia (
1,
2). One reasonable approach to testing this hypothesis is the measurement of cytokines and their soluble receptors in body fluids, because 1) increased levels of these immune system mediators are established markers of infection and inflammation (
3,
4) and 2) cytokines, such as interleukin-2, interleukin-6, and tumor necrosis factor—alpha (TNF-α), are important mediators of interactions between the CNS and the immune system (
5).
Antipsychotic drugs such as chlorpromazine affect cytokine secretion in animals (
6,
7). Clozapine consistently increases the plasma levels of TNF-α, soluble TNF receptor p55, soluble TNF receptor p75, and soluble interleukin-2 receptor in schizophrenic patients (
8). The effects of antipsychotic drugs on cytokine secretion are important because 1) pharmacological treatment might confound studies investigating disease-related alterations of immune function in schizophrenia; 2) recognition of drug-induced changes in cytokine secretion might help in the understanding of side effects mediated by the immune system, such as clozapine-induced fever and agranulocytosis (
8); and 3) cytokines might mediate effects of antipsychotic drugs on the CNS. TNF-α, for example, is an important mediator of the influence of endotoxin, the major cell-membrane constituent of gram-negative bacteria, on sleep (
9,
10). Similarities between the effects of endotoxin (
9) and those of clozapine (
11,
12) on night sleep suggest that the influence of clozapine on TNF-α release is involved in the drug's effects on sleep-wake behavior.
Neither short-term (
13) nor long-term (
14,
15) haloperidol treatment affects plasma levels of soluble interleukin-2 receptor. We extended the database of our preliminary report (
15) and present here the time course of rectal temperature, white blood cell counts, and plasma levels of various cytokines and soluble cytokine receptors in psychiatric patients during 6 weeks of treatment with haloperidol.
METHOD
Ten inpatients (two women, eight men; mean age=32 years, SD=14, range=19–61) were included. They all received haloperidol because of psychotic symptoms due to schizophrenia (N=8) or major depression (N=2) diagnosed according to DSM-III-R. The diagnoses were arrived at by thorough clinical interviews conducted by clinicians trained to apply DSM-III-R criteria. No patient suffered from a comorbid axis I diagnosis. After complete description of the study, all patients gave informed written consent to participate in the investigation, which had been approved by an independent ethics committee. Thorough baseline investigations, described in detail earlier (
8), did not indicate chronic or acute inflammation or infection, autoimmunological disorders, or endocrine diseases. No patient had a history of alcohol or substance abuse. No patient had been treated with haloperidol, clozapine, or phenothiazines during the last 6 months. No patient received additional antipsychotic medication during this study. Seven patients received the anticholinergic biperiden (2–4 mg/day) to control extrapyramidal side effects. The depressive patients received amitriptyline or paroxetine in addition to haloperidol.
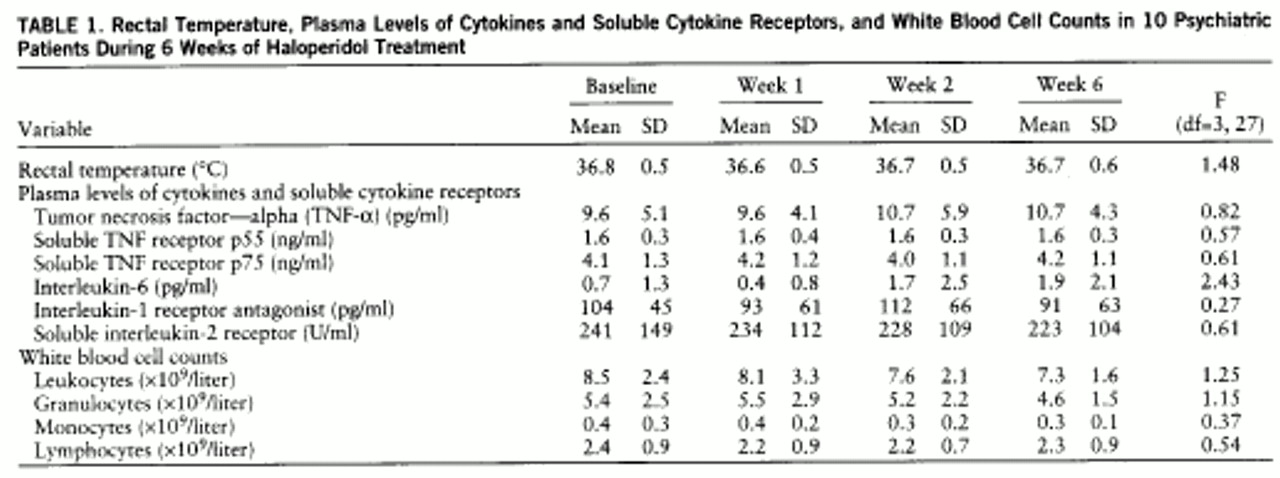
Evaluation of the target response variables was done between 8:00 and 9:00 a.m. on the first day, before haloperidol treatment began, and 1, 2, and 6 weeks after initiation of treatment. The measures included rectal temperature, white blood cell counts, and plasma levels of interleukin-6, TNF-α, soluble TNF receptor p55, soluble TNF receptor p75 (Medgenix Diagnostics, Brussels), interleukin-1 receptor antagonist (R&D systems, Minneapolis), and soluble interleukin-2 receptor (Biermann Diagnostics, Bad Nauheim, Germany). The intra- and interassay coefficients of variation were below 5% and 8%, respectively (for more methodological details see reference 8). Statistical analysis was performed by analysis of variance (ANOVA) with repeated measures followed by Bonferroni-corrected tests with contrasts, when a significant main time effect was found. As a nominal level of significance an alpha level of 0.05 was accepted. Means and standard deviations are reported.
RESULTS
The mean doses of haloperidol were 7.0 mg/day (SD=3.4), 6.9 mg/day (SD=3.4), and 5.0 mg/day (SD=3.1) at the end of the 1st, 2nd, and 6th weeks of treatment, respectively. The ANOVA for repeated measures indicated a significant decrease of dose across time (F=6.03, df=2,18, p<0.05). However, post hoc tests failed to confirm a significant difference between specific time points at the corrected level of significance. Haloperidol treatment had no significant influence on the target variables (
table 1). Excluding the two depressive patients from the data analysis had no effect on the results of the statistical tests (data not shown).
DISCUSSION
This study demonstrates that haloperidol treatment for 6 weeks has no effect on rectal temperature, white blood cell counts, and the plasma levels of various cytokines and soluble cytokine receptors. These findings extend reports showing that short-term (
13) and long-term (
14,
15) haloperidol treatment does not affect the plasma level of soluble interleukin-2 receptor. Although these results do not exclude effects of haloperidol on other aspects of immunity, they allow three conclusions. First, haloperidol at a medium dose is unlikely to confound studies investigating disease-associated alterations of the systemic levels of interleukin-6, interleukin-1 receptor antagonist, TNF-α, soluble TNF receptor p55, soluble TNF receptor p75, and soluble interleukin-2 receptor in schizophrenia. Second, although particular aspects of behavior, such as smoking (
16) and motor activity (
17), are known to affect the plasma levels of the cytokines and soluble cytokine receptors investigated in the present study, it is unlikely that these immune system variables are affected by hospitalization per se. Third, cytokines that are known to profoundly affect CNS function (
5), such as interleukin-6 and TNF-α, are unlikely to mediate the psychotropic effects of haloperidol.
To our knowledge the immunomodulatory effects of biperiden have not been investigated, and so we cannot definitely exclude the possibility that the administration of this drug to seven of the 10 patients in this study exerted effects on cytokine secretion opposite to those of haloperidol. Therefore, an investigation of patients without anticholinergic treatment would be desirable. However, because of the high frequency and the disabling nature of haloperidol's extrapyramidal side effects, such a study would be difficult to perform.