According to a 1994 report of the National Association of State Mental Health Program Directors (
2), 42 of 50 states are downsizing their state hospitals, and 12 states are actively closing them. Most of the closings are taking place in rural rather than urban settings, and, in many cases, accommodations are being made to divert new admissions to state hospital facilities in surrounding counties. To date, only Vermont, Massachusetts, and Pennsylvania have experimented with total state hospital closings, in which new admissions have stopped and substantial resources have been moved into community programs.
Similar results have been found in studies of discharged patients in England (
11,
12). However, full community integration of these patients has not occurred, and in many cases isolation and loneliness continue to be a common thread throughout the population (
13). In addition, although costs have generally been less for discharged patients living in the community (
14), this is not universal. In many cases, cost shifting, rather than cost saving, has occurred (
1,
4).
To date, no study has focused on an admission group who, in the past, would have used the state hospital intermittently for extended periods of time and, in a few cases, became long-term residents. These individuals are sometimes referred to as the “new long-stay” patients (
15–
17), although they do not necessarily represent new-onset cases. The closing of Philadelphia State Hospital in 1990 provided an opportunity to compare persons with serious mental illness who had been admitted to a state hospital before 1989 with individuals who were admitted to an extended acute care hospital bed after the state hospital closed. This study examines whether and to what extent residential alternatives and community-based inpatient services are cost-efficient substitutes for institutional care for the new population of seriously mentally ill individuals.
THE PHILADELPHIA STATE HOSPITAL CLOSURE
In 1990, the Commonwealth of Pennsylvania closed Philadelphia State Hospital, a 500-bed intermediate and long-term care facility that served 1.6 million Philadelphia residents (i.e., approximately 70% of the hospital's resident population had been institutionalized for over a year). The settlement of a legal action suit by family members of consumers resulted in an allocation of $50 million annually to the Philadelphia Office of Mental Health. These dollars were set aside to provide community accommodations and ambulatory services for the approximately 500 individuals in the discharged cohort, known as the “Class,” as well as the projected 250–300 patients per year requiring extended acute care after the state hospital closed (“divert” clients). A detailed description of the Philadelphia mental health service system after the hospital closure is found in a prior publication (
18).
Following the Philadelphia State Hospital closure, the state hospital functions were replaced by 1) 60 extended acute care beds in two community hospitals, 2) residential programs consisting of 100 long-term structured residential beds with 24-hour supervision, and 3) approximately 483 residential beds in more than 50 community residential rehabilitation facilities providing a range of maximum to moderate supervision and support services. In addition, funding from a collaborative Robert Wood Johnson grant and the U.S. Department of Housing and Urban Development was used to create supported living sites for over 200 persons with serious mental illness. In recent years, Philadelphia has added some 300 low-demand housing accommodations for homeless persons with serious mental illness, as well.
Patients were accepted for extended acute care beds as of January 1989, and, by 1993, admissions had climbed to 258 per year, comparable to the annual nonforensic admissions to Philadelphia State Hospital in the preclosure period. Extended acute care stays, in contrast to the former Philadelphia State Hospital stay, are reimbursable by Medicaid or Medicare funds, with Philadelphia State Hospital replacement funds used only for clients ineligible for these benefits. Residential admissions to community beds rose throughout this period as well, then began leveling off in 1993, when capacity was reached. The residential beds are privately operated and funded by the Philadelphia Office of Mental Health with Philadelphia State Hospital replacement dollars.
METHOD
Study Design
A pre-post study design was employed to compare the former Philadelphia State Hospital admission population with the postclosure divert group. Differences in general hospital, extended hospital, and residential stays, as well as ambulatory care, particularly intensive case management visits, were compared with respect to utilization and cost, both episodic and annual.
Study Subjects
The selection of study subjects was based on an admission to Philadelphia State Hospital between July 1986 and November 1988, or an admission to an extended acute care bed between January 1989 and July 1991, with the first admission in the pre- and poststudy period used as the “indexed” hospital event. All subjects had received acute care in community hospitals immediately before admission to extended care in both periods.
In order to avoid data-censoring problems created by unequal opportunities for service utilization, patients who had a continuous length of stay of 18 months (540 days) or more in any combination of hospital or residential accommodation were excluded from the analysis. This criterion was based on empirical findings that showed that 70% of patients admitted in both periods had a length of stay of less than 18 months, as well as on practical considerations of data availability, i.e., the postclosure population had fewer years of follow-up information. Forensic patients and individuals under 18 years of age were excluded as well.
Analysis
Two methods of analysis were used: an episode of care and an annual utilization per person. The episode of care concept was defined as a block of services received continuously in relation to a particular problem (
19). In this study it consisted of three contiguous events: an acute general hospital stay, followed by an “indexed” event in Philadelphia State Hospital or in an extended acute care unit, followed by a residential stay. (A contiguous event had to follow the previous event by no more than 1 day.) The assumption underlying the episode of care was that the combined number of general hospital stay, “indexed” extended hospital stay, and residential stay days, strung together in various combinations, represents an
equivalent period of care in both pre- and postclosure periods. Hence, the trade-off or substitution between various care components, as well as the total length of stay, can be compared.
In contrast, the annual length of stay analysis allowed for a longitudinal assessment of utilization, recidivism rates, and patterns of ambulatory care on the person or individual level. To calculate the annual utilization per group, the number of inpatient and residential bed days used 1 year before admission and 1 year after discharge from the “indexed” event were derived per person and aggregated to a group level. The days did not need to be contiguous, and the length of a particular stay was truncated if it extended on either side of the 12-month period. Ambulatory utilization was compared for the year after discharge from the indexed stay.
Differences in demographic characteristics were analyzed by using a chi-square test for categorical variables and analysis of variance for continuous variables. For the service utilization analyses that compared length of stay and number of visits between groups, the Wilcoxon rank-sum test for nonparametric statistical tests was used, since assumptions regarding equal variances and independence between mean and standard deviation did not always hold.
Cost
Inpatient and residential care costs in both periods were based on 1992 dollars. The episode of care cost was derived by using the average length of stay per bed type (i.e., general hospital, extended hospital, residential) multiplied by the average cost. The annual cost per person was derived from 2 years of service utilization data that included the indexed event and were then annualized. For purposes of comparison with other studies of discharged state hospital patients, the cost of care was also estimated for the year following discharge from the indexed event. The costs are those incurred by the State Medicaid Agency, Medicare, the State Mental Health Agency, and the County Office of Mental Health, which manages the ambulatory mental health budget.
Data Sources
Utilization and cost data were collected from eight administrative data files spanning a 9-year period between 1985 and 1993 (
20). Medicaid and Medicare claims records, as well as county- and state-funded data on inpatient treatment in community and state hospitals, residential placement, and all ambulatory services, were used to construct the study variables. Service utilization measures were constructed from claims records and address variables such as date of service, type and intensity of service, diagnosis, and provider of service. Unit cost information on all services was derived from claims and administrative data sources (Medicaid cost reports, county contracts, state cost reports); 1992 cost figures were used for comparison purposes. Data on boarding home use were not available in either period. However, the majority of study subjects were placed in state-funded residential settings.
RESULTS
Subject Characteristics
A total of 322 preclosure patients admitted to the state hospital and 163 postclosure patients admitted to extended acute care met the study criteria. Fewer subjects were identified in the postclosure period because extended acute care admissions were lower during the beginning phases of program implementation, since all extended acute care beds were not operational. Acute care general hospital admissions for schizophrenia and major depressive disorder increased during this period; this increase was likely caused by patients who were potential extended acute care admissions.
Both pre- and postclosure groups were predominantly African American (62% and 56%) (χ2=1.77, df=2, p=0.41), had a diagnosis of schizophrenia (86% and 88%) (χ2=0.39, df=1, p=0.53), and were between 37 (SD=12) and 40 years old (SD=12) (F=5.89, df=1,481, p=0.02). However, there was a significant difference in that a greater proportion of the postclosure group received income support through programs such as Supplemental Security Income (64% versus 75%) (χ2=6.88, df=1, p=0.009) and Social Security disability insurance (19% versus 28%) (χ2=5.82, df=1, p=0.02). Rather than reflecting a difference in disability levels between the preclosure and postclosure groups, the greater portion of the postclosure group meeting the Supplemental Security Income/Social Security disability insurance criteria after the state hospital closed is probably due to enhanced support provided to clients by intensive case managers in negotiating the eligibility process.
An analysis of admission patients who did not meet study criteria found significant differences for the preclosure group only in race and age. The excluded group had a higher proportion of African American subjects (62% versus 45%) (χ2=7.8, df=1, p=0.005) and was older (mean=43 years, SD=14, versus mean=37 years, SD=12) (F=16.5, df=1,402, p=0.001). These differences should not, however, affect the generalizability of the results.
Episode of Treatment
A subset of episodes experienced by the 322 patients in the preclosure cohort and the 163 in the postclosure cohort met the episode of treatment criterion. Thus, 218 preclosure admissions and 128 postclosure admissions had contiguous events constituting an episode of care. The smaller number of postclosure episodes, again, reflects lower admission rates for the extended acute care beds between 1989 and 1991.
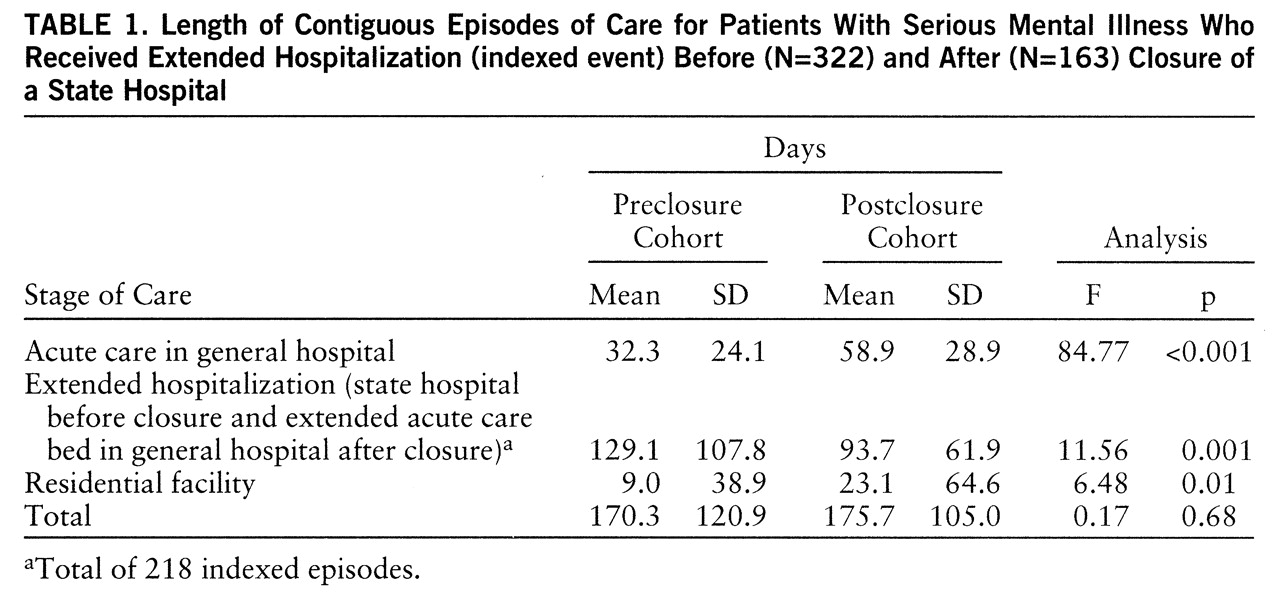
Table 1 shows the mean number of days for each component comprising the episode of care (general hospital-extended hospital-residential). A clear pattern of bed substitution emerged in the postclosure period, with acute care hospital days (general hospital) almost doubling, from 32 to nearly 59 days (Wilcoxon z=8.512, p<<0.001, N=346); the indexed stay decreasing significantly, from 129 to nearly 94 days (Wilcoxon z=–2.169, p=0.03, N=346); and residential days increasing significantly, from 9 to 23 days per group member (Wilcoxon z=2.507, p=0.01, N=346). Although there were significant differences between groups in the allocation of days among care components, the total number of days per episode was similar.
Annual Length of Stay
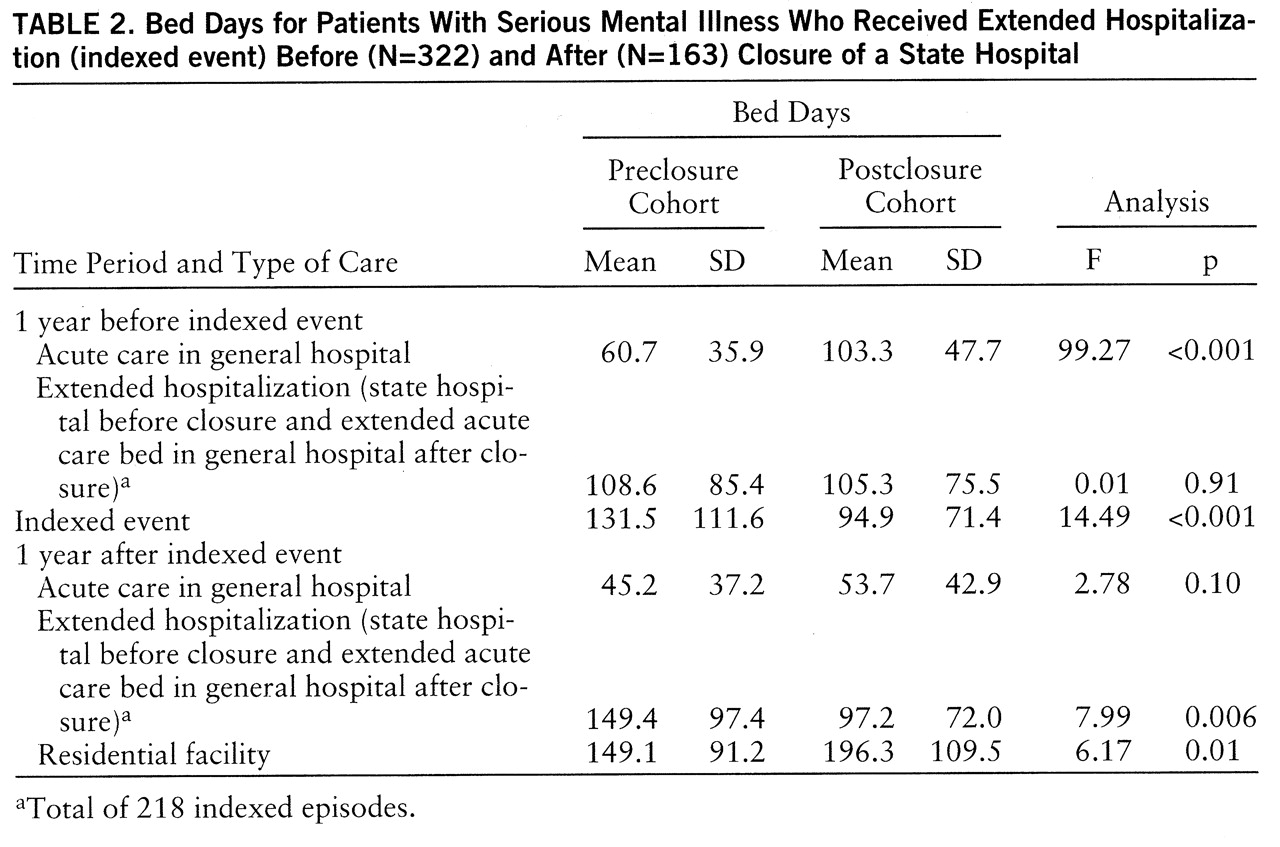
Table 2 shows the service utilization patterns of both groups 1 year before and 1 year after their indexed event. The number of general hospital days increased significantly from before the indexed event to the postclosure period (from nearly 61 to 103 days; Wilcoxon z=8.822, p<<0.001, N=388). Although the number of general hospital days after discharge was not statistically significant (Wilcoxon z=1.543, p=0.12, N=250), the general hospital admission rate in the postclosure period, upon examination, was significantly higher than the preclosure rate (47% versus 63%) (χ
2=11.25, df=1, p=0.001).
Although no significant difference was observed between groups in the number of extended hospital days before the indexed event, extended hospital days were significantly fewer in the postclosure period following the indexed discharge (97 versus 149 days) (Wilcoxon z=–2.829, p=0.005, N=485). This suggests that the shorter indexed stays found in the postclosure period resulted in higher readmissions to extended care (16% versus 24%) (χ2=3.93, df=1, p=0.05). Finally, residential days increased significantly in the postclosure group following discharge from the indexed event (Wilcoxon z=–2.223, p=0.03, N=116).
Ambulatory Treatment Patterns
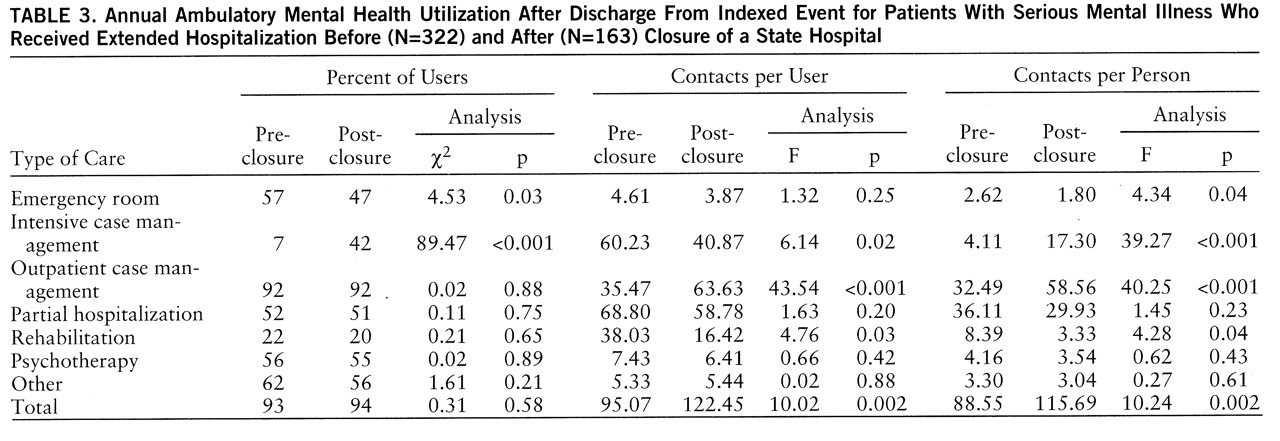
A comparison of ambulatory mental health utilization following the indexed event is shown in
table 3. The percent of individuals using intensive case management services was significantly greater after the state hospital closed; however, far fewer individuals used emergency rooms after the indexed event. Nevertheless, for those individuals who used emergency room services, the number of visits remained similar in both periods (mean=4.6 visits, SD=4.9, versus mean=3.9, SD=4.1).
In contrast, the average annual number of intensive case management contacts per user was significantly smaller for the postclosure group (Wilcoxon z=2.142, p=0.03, N=91). This suggests that although intensive case management services were being used more widely throughout the mental health system, the intensity of use per person had been reduced. What is clear is that both the pre- and postclosure groups appear to have had a similarly high proportion of individuals making contact with the ambulatory system following discharge from an extended acute care stay (93% versus 94%). However, the average number of ambulatory contacts per user was significantly higher in the postclosure period (Wilcoxon z=3.676, p<<0.001, N=454). Despite this increase in outpatient care, acute care hospital days increased, suggesting that ambulatory care may not be a substitute for hospitalization in this population.
Cost Comparison
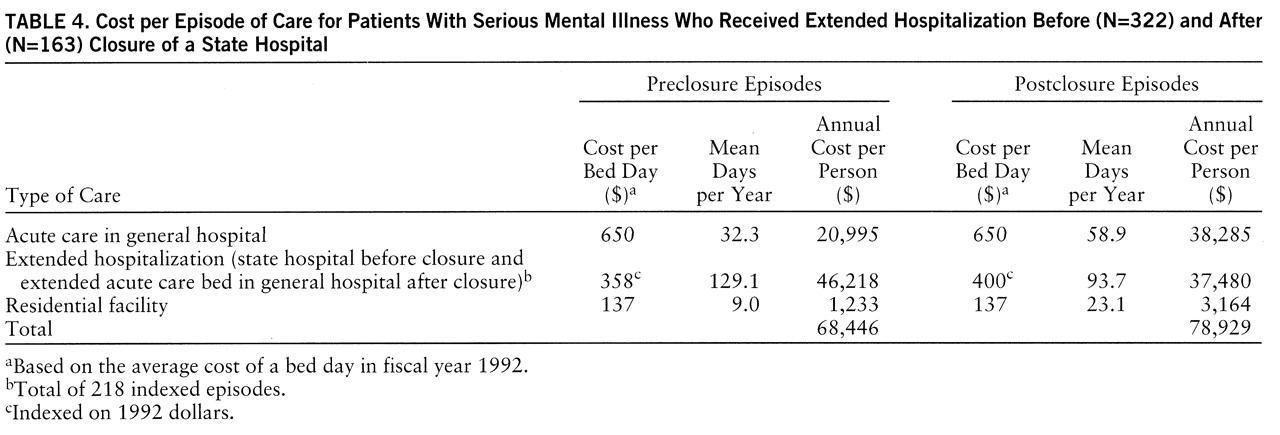
Table 4 shows the episode of care cost to be higher in the postclosure period than in the preclosure period ($78,929 per individual, versus $68,446), when indexed on 1992 dollars. The cost increase was due primarily to the increased use of general hospital acute care days, which are the most expensive care component.
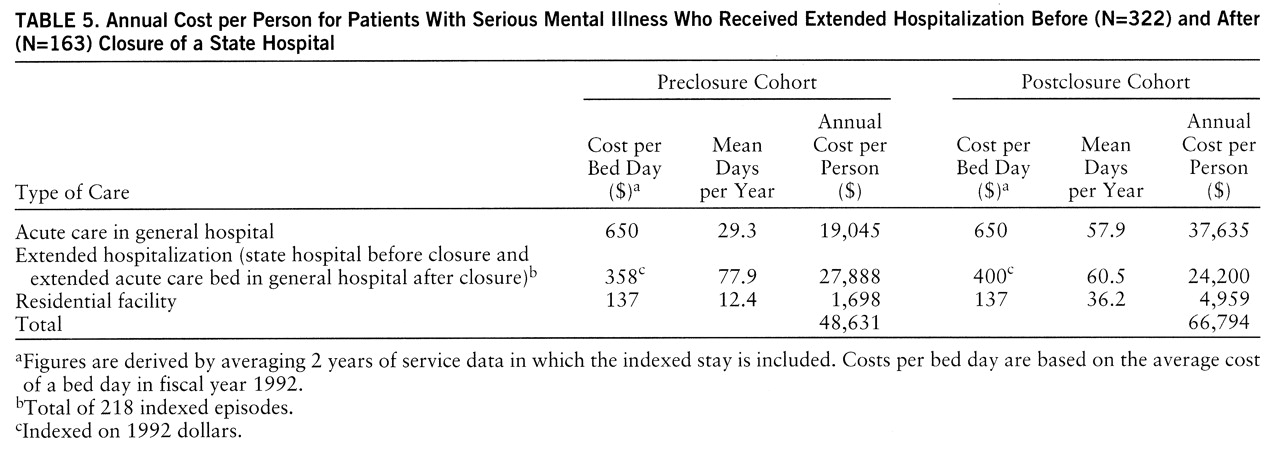
Table 5 presents a similar picture in that the annual cost per person, based on a 2-year service utilization history incorporating the indexed event, was $48,631 per person for the preclosure group compared to $66,794 per person for the postclosure group. Despite a trade-off between residential and extended hospital days in the postclosure period, the increased use of expensive general hospital beds before and after the indexed event drove the total annual cost up significantly.
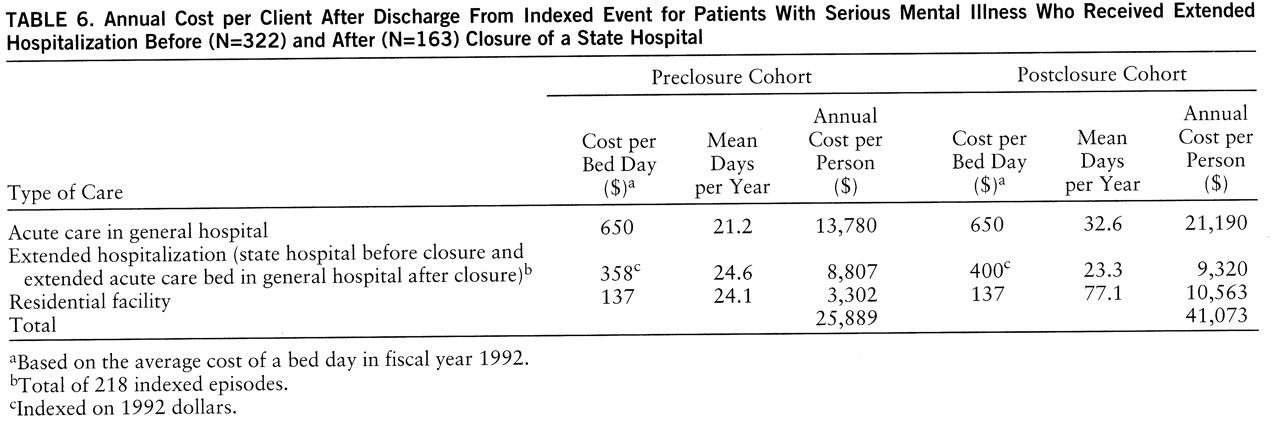
An alternative way of examining costs is to construct the use of services 1 year following discharge from the indexed event. This method has been used to determine the cost of caring for a “discharged” cohort and is considered a cost substitute for long-term hospitalization.
Table 6 shows that the cost per person in the year following the indexed discharge was higher than that in the postclosure period, with expenditures averaging $41,073 per person compared to $25,889 for the former state hospital patient. The increased use of general hospital days remained higher, both before and after the indexed event.
DISCUSSION
The major finding of this study is that the direct cost of treating individuals who require extended hospitalization (i.e., divert group) in an unbundled state hospital system was greater after the state hospital closed. Despite the decreased number of extended care days and the increased supply of residential care slots, individuals having acute care episodes that required hospitalization had higher episode and annual costs in the postclosure period. The data suggest that the increased costs were due primarily to the increased use of acute care general hospital days that were the consequence of patients queuing up in general hospitals while waiting for a transfer to an intermediate care unit.
There are several caveats, however, that must be noted in interpreting these results. First, this study was implemented during a period when the full components of the new unbundled system were not completely in place. Between 1992 and 1995, acute care hospital days declined for patients referred to extended acute care beds. Nevertheless, length of stay before an extended acute care admission still averaged 22 days higher than it was during the preclosure period, even with the full complement of beds. In addition, length of stay for the indexed extended hospital admission decreased during this period, as well, from 90 to 85 days, but, as anticipated, residential stays continued to increase and new admissions to residential units declined as capacity was reached.
An important factor that may have led to the increased use of acute care general hospital days was a finance incentive, whereby acute care beds in general hospitals, unlike former state hospital beds, were eligible for Medicaid and Medicare reimbursement. As a consequence, the Philadelphia Office of Mental Health used the state hospital replacement dollars to develop residential and ambulatory programs for persons with serious mental illness, while allowing the cost of extended acute care beds to be paid for by Medicaid. The rationale for this behavior no longer exists today because in July 1997 the city assumed the behavioral health care risk for the entire Medicaid population and now must pay for acute care general hospital days as part of its capitated rate agreement with the State (
21).
Another caveat in interpreting these findings is that the cost calculations focus only on direct inpatient treatment and residential care. The cost of ambulatory care is absent, as are indirect costs not related to treatment, i.e., social costs. Data are also lacking on the use of nontraditional services such as clubhouses, drop-in centers, and other informal programs. Notwithstanding the importance of ambulatory care and nontraditional services, other studies have found that the total cost differences are small when nonhospital care is excluded, since hospital and residential services explain 80% or more of total costs (
22,
23). Our study findings also show that with respect to ambulatory costs, the only appreciable increase in ambulatory care for this population during the postclosure period was in case management services (
table 3). Although case management is costly, the decrease in emergency room and rehabilitative care services in the postclosure period likely offset the case management expenses. Future studies, however, should explore indirect costs to ascertain the total economic costs of a system change such as this.
Another limitation that should be noted was the lack of a control group, which meant that we could not account for changes in the type of admissions or referrals for extended care. Despite the fact that study criteria required all subjects to be admitted to a community hospital before an extended care referral, and all subjects had to have prior treatment histories of inpatient and emergency room use, it is still possible that subjects in the postclosure period were different from those in the preclosure period.
Furthermore, caution must be applied in using these results to characterize closures in general, since the results of our study are limited to an admissions population that made up approximately 30% of the former Philadelphia State Hospital population in any 1 year. In the past, approximately one-quarter of the new admissions each year became long-stay patients. Future analysis is needed to determine whether the “new” long-stay population will be costlier over long periods when compared to the prior state hospital era. A more comprehensive cost analysis of the entire state hospital population, including the discharged long-stay patients living in the community today, is forthcoming.
Despite these precautions in interpreting this study, there is, as of 1995, no empirical evidence to show that hospital admissions for persons with schizophrenia and major affective disorders are decreasing despite a wealth of community programs. Anecdotal evidence suggests that more highly structured residential accommodations are needed to alleviate the queue in the general hospital and extended acute care units. However, unless discharge criteria for residential stays are developed, or new residential programs opened, a crisis may occur in future years. A preliminary bed simulation model, using Philadelphia State Hospital data, projected that if residential accommodations remained stable, extended acute care beds should be increased from 60 to 85 beds in order to optimize total system costs. The model, which is based on admission rates, length of stay, and cost per bed day, is being refined and tested on more recent data (
24).
Although new configurations may optimize costs over the next few years, it is impossible to project the experience of the current seriously mentally ill population, who may incur more psychiatric and substance abuse hospitalizations living in the community because of shorter inpatient treatment periods and a less structured, more vulnerable environment. On the other hand, reduction in long-term institutionalization may prevent the condition of dependence known as social breakdown syndrome, noted by Gruenberg (
25) many years ago. This might ultimately lead to greater independence and less chronicity over time for future populations. Continued monitoring of the community system of care is clearly needed.