In patients manifesting suicidal behavior, indications of reduced central serotonergic function have been found across boundaries of specific psychiatric disorders (
1–
3). This suggests that agents enhancing serotonergic transmission, like selective serotonin reuptake inhibitors (SSRIs), may be effective in the treatment of suicidal behavior. Some studies reported a more rapid improvement of suicidal ideation in patients with major depression with SSRIs than with other antidepressants (
4,
5). In contrast, patients have been described who experienced intense suicidal ideation (
6–
9) or sudden urges to harm themselves (
10) after starting or increasing the dose of the SSRI fluoxetine. Nevertheless, analyses of pooled, double-blind drug studies in patients with major depression indicated less emergence of substantial suicidal ideation with SSRIs than with tricyclics or placebo (
11–
13). The SSRI fluoxetine appeared to be superior to placebo in the reduction of suicidality in obsessive-compulsive disorder (
14), anxiety disorders (
15), and bulimia nervosa (
16) but not in recurrent brief depression (
17).
Recurrent suicide threats are among the characteristics of borderline personality disorder (DSM-III-R and DSM-IV). Several small open trials with 5 to 80 mg/day of fluoxetine (
18–
21) and 50 to 200 mg/day of sertraline (
22) demonstrated improvement in suicidality, self-injury, and impulsive aggression in patients with borderline personality disorder. In a double-blind, placebo-controlled study, a decrease in anger was shown with 20 to 60 mg/day of fluoxetine (
23).
In conclusion, several reports suggest the efficacy of SSRIs in treating suicidal and aggressive behavior. However, this effect may vary between different patient subgroups. The aim of the present study was to assess the efficacy of the SSRI paroxetine in the treatment of patients with a high risk of recurrent suicide attempts. Because the number of previous suicide attempts (
24,
25) and presence of a personality disorder—particularly a cluster B personality disorder (
25–
28)—are predictors of repetition of suicidal behavior, the impact of these variables has been taken into account.
METHOD
Subjects were recruited from 298 consecutively treated outpatients in the emergency departments of the University Hospital of Leiden and the University Hospital of Rotterdam who had attempted suicide, who had a history of at least one previous suicide attempt, and who were 18 years old or older. No screening assessment could be established with 37 of the patients, and 54 refused to join the study. Patients were excluded if they had a major affective disorder or were using antidepressants (N=49), if they had a psychotic disorder or were using antipsychotics (N=24), if they had an organic mental disorder (N=5), if they were dependent on alcohol or any other substance (N=27), if they were using other prohibited medication (N=1), if they had a serious physical disease (N=4), or if they were unable to cooperate (N=6). DSM-III-R axis I diagnoses were assigned on the basis of a comprehensive psychiatric examination and structured interview by one of the authors (R.J.V. or J.P.T.).
Of the 91 patients who entered the study, six had a current diagnosis of dysthymia, four were suffering from an anxiety disorder, eight had a dissociative disorder, 40 had a diagnosis of alcohol abuse, 19 had an adjustment disorder, 23 had depressive disorder not otherwise specified, and 15 were not given a diagnosis; 23 patients had more than one diagnosis. Five patients had a past history of a major depressive episode. Twenty-eight patients had a history of five or more suicide attempts, including the index attempt. According to the definition by Kreitman and Casey (
29), the patients who had attempted suicide five or more times are called “major repeaters,” and those who had attempted suicide one to four times are called “minor repeaters.” DSM-III-R axis II criteria were assessed by using the Personality Diagnostic Questionnaire—Revised (
30). All but seven patients met the criteria for one or more DSM-III-R personality disorders (cluster A, N=65; cluster B, N=74; cluster C, N=60).
After a placebo washout period of 2–4 weeks, the patients were randomly assigned to one of two treatment groups receiving either paroxetine or placebo. Patients in the paroxetine group received 20 mg/day of paroxetine for 1 week followed by a fixed dose of 40 mg/day of paroxetine for up to 52 weeks. Patients in the placebo group received matching placebo. In addition to study medication, supportive psychotherapy was offered on a weekly to fortnightly basis.
Only benzodiazepines were allowed as concomitant psychotropic medication, with the restriction that the dose remain stable throughout the study. Benzodiazepines were used by 28 patients in the placebo group and 24 patients in the paroxetine group.
Recurrence of suicidal behavior and safety factors such as adverse events and vital signs were assessed at baseline, after weeks 2, 4, 6, 8, 10, and 12 of treatment, and at monthly intervals thereafter until 52 weeks. As secondary outcome measures, changes from baseline in some suicidality-related measures (depressive mood, hopelessness, and anger) were used. Depressive mood was assessed by using the total score on the Beck Depression Inventory (
31), hopelessness was assessed by using the Beck Hopelessness Scale (
32), and anger was measured by using the state scale of Spielberger's State-Trait Anger Expression Inventory (
33).
At each visit, medication compliance was assessed by capsule count. Furthermore, platelet serotonin content was measured at baseline and after 2, 8, 20, 32, and 52 weeks. Platelet serotonin decreases significantly when an SSRI is administered and could serve as an indicator for compliance in the paroxetine group (
34). Platelet serotonin content was determined as described previously (
34).
Efficacy was analyzed on an intention-to-treat basis; all available observations were used without the last point carried forward or estimating missing values. We also analyzed efficacy excluding the noncompliant visits. The time from baseline to first recurrence of a suicide attempt was considered to be the primary endpoint. The treatment effect with regard to this endpoint was analyzed by using the log-rank test and Cox's regression model. The effect of treatment on change in depressive mood, hopelessness, and anger compared with baseline was analyzed by using repeated measures analysis of variance for treatment group with visit number and baseline scores as covariables. Between-group differences in the incidence of adverse events were assessed by using Fisher's exact test. Two-tailed probabilities with an alpha level of 0.05 were applied throughout.
The study was approved by the ethical committees of the Leiden and Rotterdam university hospitals. After a complete description of the study, written informed consent was obtained from all subjects.
RESULTS
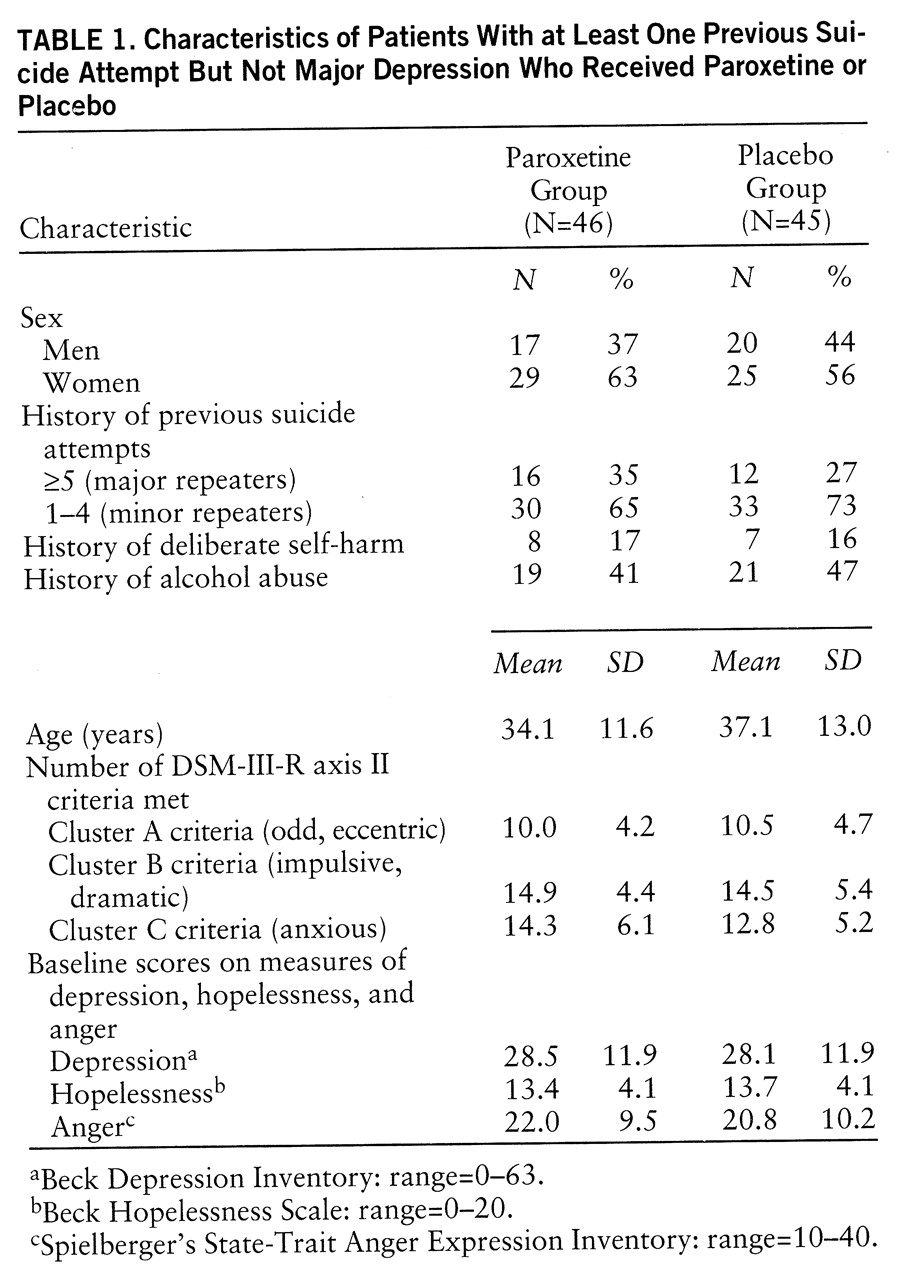
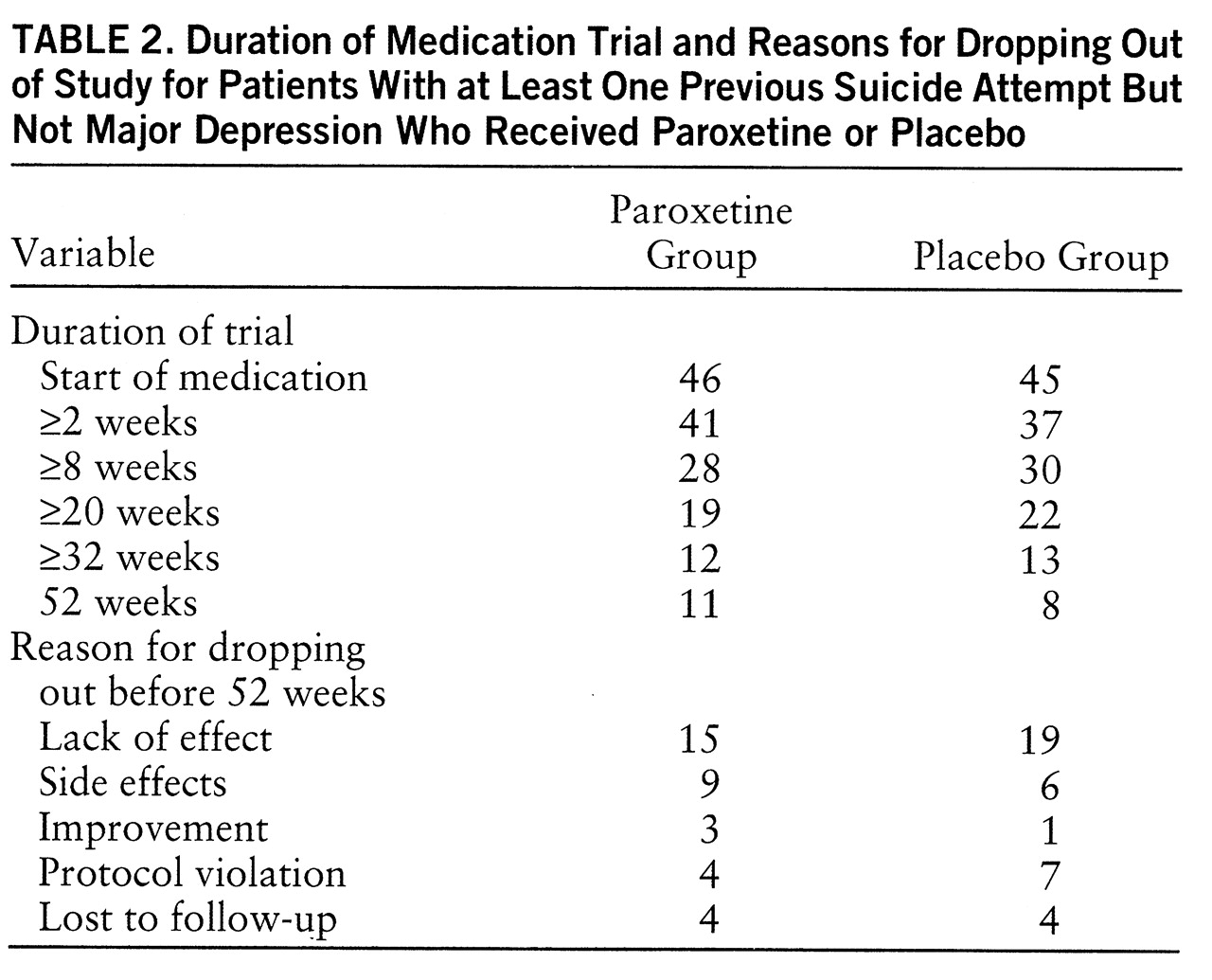
Of the 91 patients, 46 were randomly assigned to receive paroxetine and 45 to receive placebo. Random assignment produced comparable groups (
table 1). The groups were also comparable with respect to dropout rate and reasons for dropping out (
table 2).
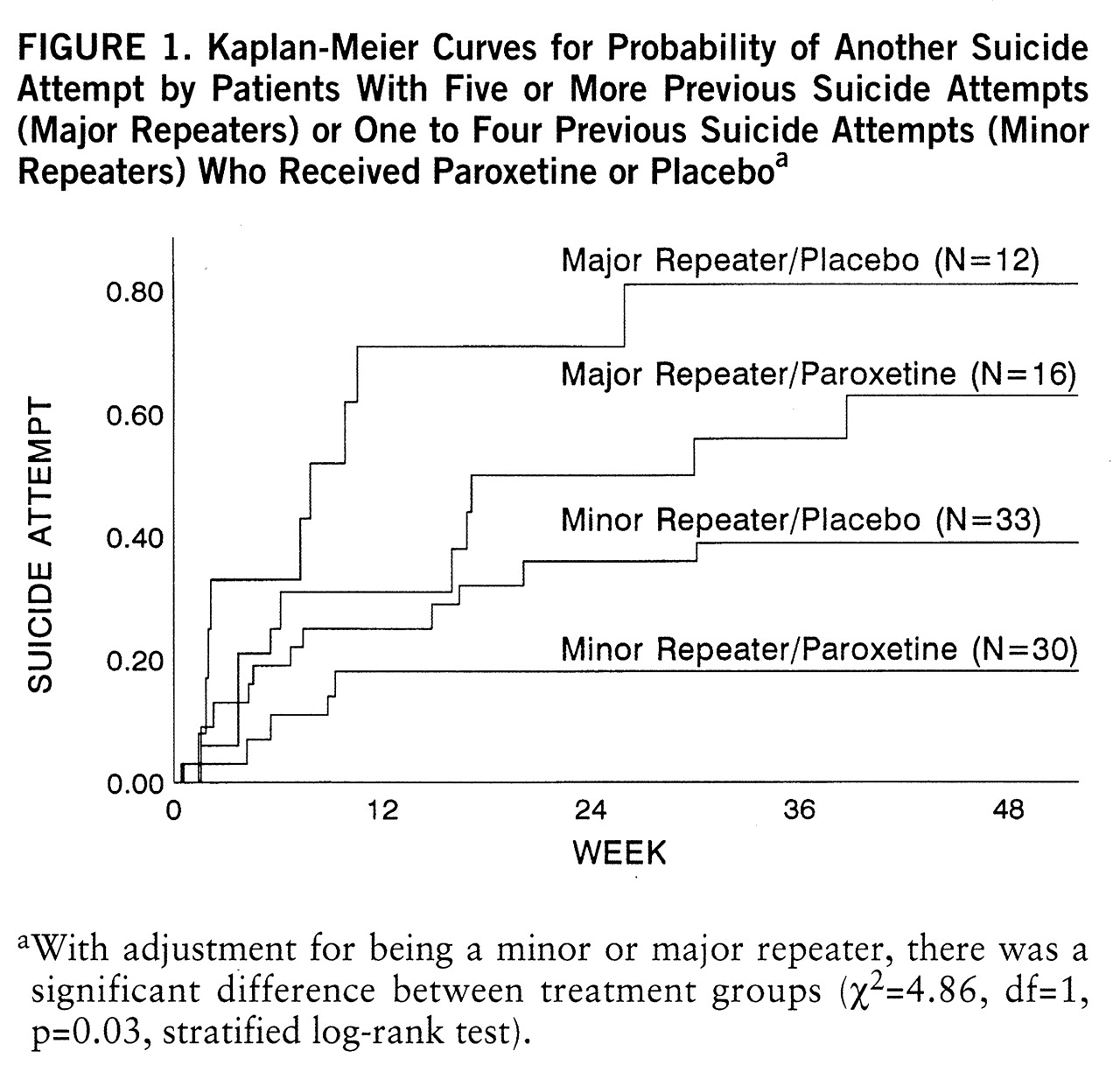
Fifteen patients (33%) in the paroxetine group and 21 patients (47%) in the placebo group made another suicide attempt (χ
2=2.42, df=1, p=0.12, log-rank test). The number of previous suicide attempts (i.e., being a minor or major repeater) was manifestly associated with the risk of another suicide attempt (χ
2=12.40, df=1, p<0.001, log-rank test). With adjustment for this important predictive characteristic, paroxetine proved to reduce the recurrence of suicidal behavior significantly (
figure 1). As shown in
figure 1, within the minor repeater group, recurrence of suicidal behavior occurred in five (17%) of 30 patients receiving paroxetine, compared with 12 (36%) of 33 patients receiving placebo. One minor repeater receiving placebo committed suicide. Within the major repeater group, 10 (63%) of 16 patients receiving paroxetine, compared with nine (75%) of 12 receiving placebo, attempted suicide again.
The impact of personality disorder on recurrence of suicidal behavior was studied for the three DSM-III-R clusters separately. Median splits were used according to the number of criteria met in clusters A, B, and C, respectively. Using Cox's regression model, we found what appeared to be a significant interaction between drug and number of cluster B criteria (χ2=4.96, df=1, p=0.03, Wald test), indicating that paroxetine was significantly more effective in patients meeting fewer than 15 criteria than in patients meeting 15 or more criteria. Forty-six patients met fewer than 15 cluster B criteria; 22 of these patients received paroxetine, and 24 received placebo. The suicide attempt recurrence rate among the patients receiving paroxetine (14% [N=3]) was significantly lower than the rate among the 24 patients receiving placebo (50% [N=12]) (χ2=7.03, df=1, p=0.008, log-rank test). Among the 45 patients who met 15 or more cluster B criteria, the recurrence rates of 50% (N=12) in the 24 patients receiving paroxetine and 43% (N=9) in the 21 patients receiving placebo did not differ significantly. There appeared to be a manifest association between being a major repeater and meeting cluster B criteria in that only four (9%) of the 46 patients with fewer than 15 cluster B criteria were major repeaters, compared with 24 (53%) of the 45 with 15 or more cluster B criteria (χ2=21.28, df=1, p<0.001).
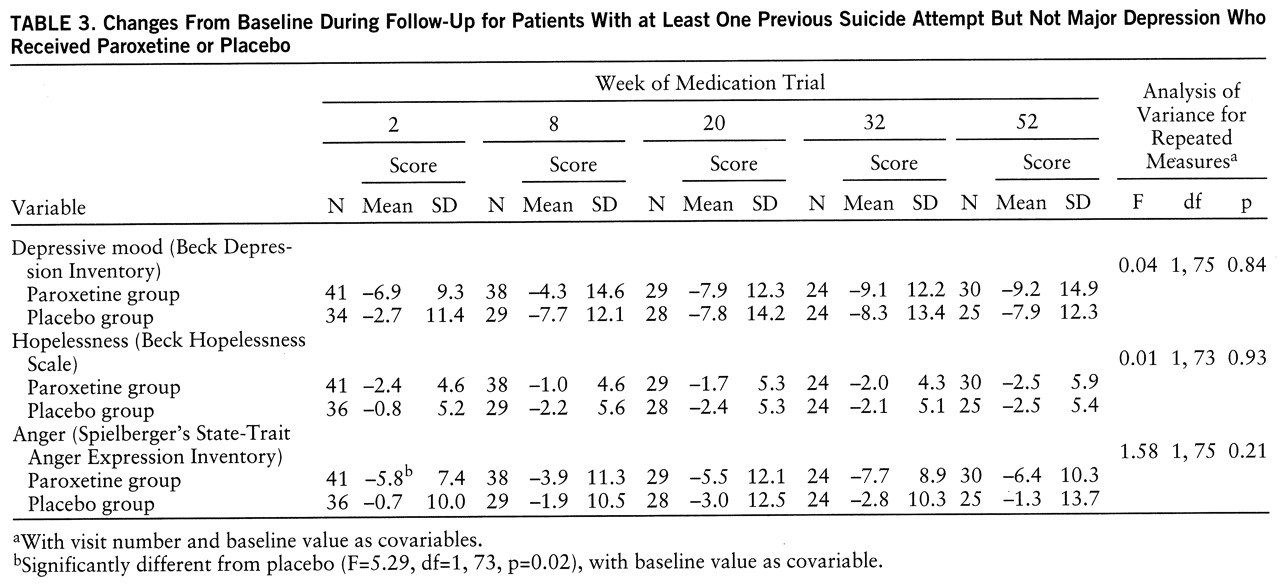
To explore the effect of paroxetine on depressive mood, hopelessness, and anger, we examined the data for the 77 patients for whom these measures were assessed after 2 weeks of using trial medication. Overall, there was no significant treatment effect for any of these variables, although anger decreased significantly more in the paroxetine group than in the placebo group after 2 weeks and remained lower, but not significantly, for the rest of the trial period (
table 3).
With respect to compliance, analysis of capsule counts at each visit revealed no statistically significant differences between treatments. Levels of platelet serotonin were not substantially decreased at week 2 in five patients, indicating doubtful compliance, and showed a manifest increase following a previous definite decrease in four other patients—at week 8 (N=2) and week 52 (N=2). Efficacy analyses restricted to the visits with undoubted use of trial medication yielded essentially the same results as the intention-to-treat analyses.
Adverse events that occurred significantly more often with paroxetine (N=46) than with placebo (N=45) were delayed orgasm (N=9 versus N=0) (p=0.003, Fisher's exact test), diarrhea (N=10 versus N=1) (p=0.007, Fish~er's exact test), and tremor (N=8 versus N=1) (p=0.03, Fisher's exact test). Substantial ecchymoses occurred in two patients taking paroxetine.
DISCUSSION
Paroxetine appeared to be effective in the prevention of recurrent suicide attempts. This effect was observed in minor repeaters and—amounting to the same—in the subgroup of patients not too severely compromised by cluster B personality traits. Paroxetine failed to show a significant effect on depressive mood, hopelessness, or anger. However, our data suggest that paroxetine may have some temporary effect in reducing anger. This effect appeared in the first 2 weeks of treatment, which is in accordance with reports by others on the effects of SSRIs in borderline patients (
18,
19,
21,
22) and a mixed group of patients experiencing intense anger (
35).
To our knowledge, this is the first double-blind, placebo-controlled study of the effect of an SSRI on recurrent suicidal behavior in a clinically relevant group of patients without major depression. A strength of the study is the follow-up of 1 year. Limitations consist in the use of solely subjective self-rating scales for depressive symptoms and anger and the use of a self-report questionnaire to assess axis II diagnoses. Given the observed importance of personality pathology, a structured interview schedule would have been preferable.
Further research is indicated to replicate our findings and to further characterize the patients who may benefit from treatment by an SSRI. However, our results provide support for the hypothesis that agents enhancing serotonergic function have an effect on suicidal behavior.