In a previous study (
1), we reported that 13 (65%) of 20 Bosnian refugees were diagnosed with posttraumatic stress disorder (PTSD) just after being resettled in the United States; this rate of PTSD is consistent with rates reported in other traumatized refugee groups (
2,
3). Few empirical data exist on how PTSD in traumatized refugees changes over time (
4). Prospective studies of PTSD have been done with survivors of disaster and combat (
5,
6). However, no studies have addressed the longitudinal course of PTSD in traumatized refugees during the early phase of resettlement. This phase is characterized by psychological stressors associated with recent (or continued) traumatization, social isolation, language difficulties, unemployment, and family instability, but it is also characterized by psychological gains through adjustment and recovery in these same realms.
Our goal in this paper is to describe 1) the characteristics of PTSD symptoms in Bosnian refugees at resettlement in the United States and at 1-year follow-up and 2) possible factors affecting the PTSD symptom profile among refugees.
METHOD
The subjects were 34 Bosnian refugees who were originally evaluated soon after their resettlement in Connecticut. Sixteen were females and 18 were males; they ranged in age from 13 to 59 years. All had previously lived in Bosnia and were ethnic Muslims. They were referred to our group by refugee resettlement organizations in Connecticut. For the follow-up study, the original participants were contacted by letter or telephone. All gave written informed consent to participate in this project.
The procedures for the initial study have been described elsewhere (
1). Assessments included the PTSD Symptoms Scale (
7), the Communal Traumatic Experiences Inventory (
1), the Global Assessment of Functioning (DSM-IV), and the SCL-90-R (
8).
All refugees had the opportunity to participate in testimony interviews, which were adapted from the brief psychotherapeutic method described for working with survivors of political violence (
9). All 34 subjects participated in testimony interviews as part of their initial evaluation, which may have influenced their clinical course.
RESULTS
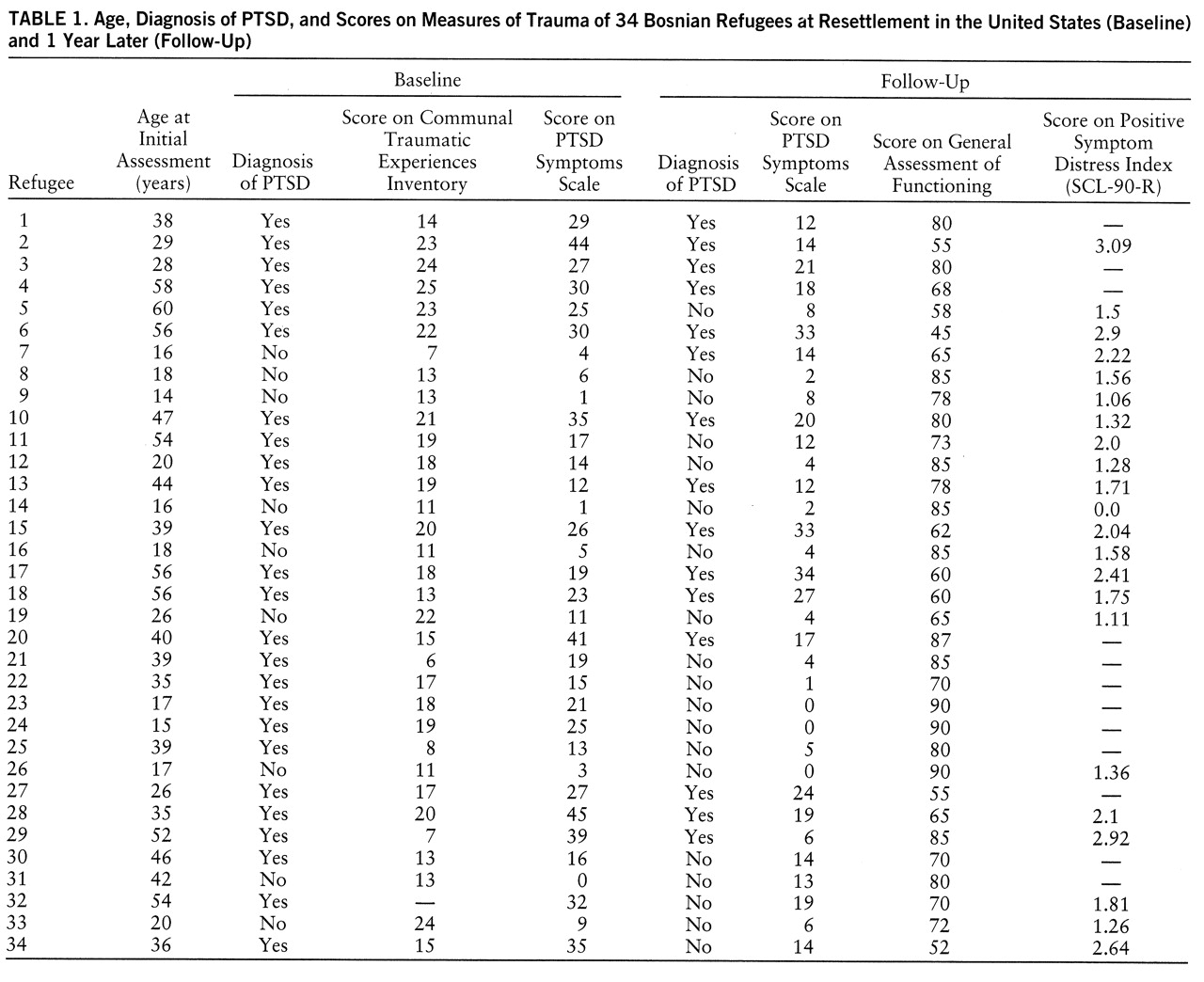
Table 1 summarizes baseline and follow-up assessment data—including age, diagnosis of PTSD, Communal Traumatic Experiences Inventory score, PTSD Symptom Scale score, Global Assessment of Functioning scores, and Positive Symptom Distress Index (PSDI) scores from the SCL-90-R. At baseline, 25 subjects met criteria for PTSD; symptom severity scores were generally high (mean=20.6, SD=13.0). At follow-up, 15 subjects met criteria for PTSD, and only one of these subjects did not have PTSD at baseline; severity scores were lower at follow-up (mean=12.5, SD=9.9). Twenty-five subjects showed decreases in PTSD severity over the follow-up interval, eight showed increases, and one remained the same.
At baseline, older age was associated with a higher rate of diagnosis of PTSD (r=0.59, df=32, p<0.0001, point biserial correlation coefficient), higher PTSD severity scores (r=0.46, df=32, p<0.01), and higher PSDI scores (r=0.47, df=29, p<0.01); older age at baseline was inversely related to Global Assessment of Functioning score (r=–0.46, df=32, p<0.01). At 1-year follow-up, the correlation of age with PTSD diagnosis approached but did not reach significance (r=0.32, df=32, p=0.06, point biserial correlation coefficient). At follow-up, older age was still associated with higher PTSD severity scores (r=0.57, df=32, p<0.0001) and higher PSDI scores (r=0.41, df=20, p<0.05), and older age was inversely related to Global Assessment of Functioning score (r=–0.44, df=32, p<0.01). At baseline, Communal Traumatic Experiences Inventory scores did not correlate significantly with PTSD diagnosis or with PSDI or older age, although the correlation between Communal Traumatic Experiences Inventory score and the diagnosis of PTSD approached significance (r=0.31, df=31, p=0.08, point biserial correlation coefficient). Similarly, at follow-up, Communal Traumatic Experiences Inventory scores did not correlate with PTSD diagnosis, older age, or PSDI.
At baseline, the three symptoms that occurred most frequently at the highest severity ratings were avoiding thoughts of the war, intrusive memories, and being upset when reminded of the traumata. Twenty-one subjects reported reexperiencing cluster symptoms, 18 reported avoidance cluster symptoms, and 12 reported hyperarousal cluster symptoms. At follow-up, the most frequent symptoms were being upset when reminded of the traumata, intrusive memories, and feeling that the future was unclear. Twenty subjects reported re~experiencing cluster symptoms, 11 reported avoidance cluster symptoms, and 13 reported hyperarousal cluster symptoms.
DISCUSSION
We found a high rate of PTSD among 34 Bosnian refugees, indicating that there are continued, serious mental health problems—even 1 year into resettlement and several years after the initial traumatization. The substantial decreases in the rate of PTSD diagnosis and in the severity of symptoms, however, are evidence of clinical improvement. This recovery process is likely due to many factors, including 1) the passing of time since the most severe traumata, 2) the passing of time since the shock of displacement on coming to the United States, 3) acculturation, 4) increased stability in the realms of family, work, community, or other aspects of life structure, and 5) participation in testimony or other opportunities to communicate traumatic memories. We also found continued evidence of age-related differences in PTSD at follow-up.
Our findings regarding the symptom clusters suggest that after 1 year, Bosnian refugees were using less of what might be characterized as more primitive defensive functions—such as avoidance, numbing, splitting, and denial—to distance themselves psychologically from traumatic memories. A growing ability to relate flexibly to their traumatic memories may also be a consequence of participation in testimony—as well as other opportunities to express and communicate memories made possible by adjustment and acculturation or other time-dependent changes in mind/brain functioning.
This study has several limitations. The number of subjects is small, limiting generalizability. Not all of our subjects completed all of the assessments. Finally, the validity of our instruments may have been affected by language and ethnocultural differences. This study has captured some but not all of the dynamics of the natural history of posttraumatic conditions. Of course, it does not address changes that may be subsequent to the first year in the evolutionary processes of recovery and resettlement. Further studies are needed to address other facets of trauma and PTSD—including ethnocultural, developmental, human rights, and memory dimensions.