Overall Outcomes
Eighty-one percent (N=237) of the 291 patients completed the 12-week program; 82% (N=119 of 145) completed the day treatment program, and 81% (N=118 of 146) completed enhanced standard care, with no difference in survival time (day treatment program: mean=10.9 weeks, SD=2.7; enhanced standard care: mean=10.7 weeks, SD=2.9; log rank=0.17, p=0.68). Nine dropouts were transferred to inpatient drug treatment, six were incarcerated, four were hospitalized for medical reasons, two requested detoxification, and the rest were administratively discharged for missing three consecutive methadone doses. The patients who completed treatment did not differ from the treatment dropouts in demographic characteristics, psychiatric diagnosis, or drug use history with one exception: patients with a diagnosis of antisocial personality disorder were less likely to be retained, regardless of assigned treatment intensity (χ2=7.99, df=1, p<0.005).
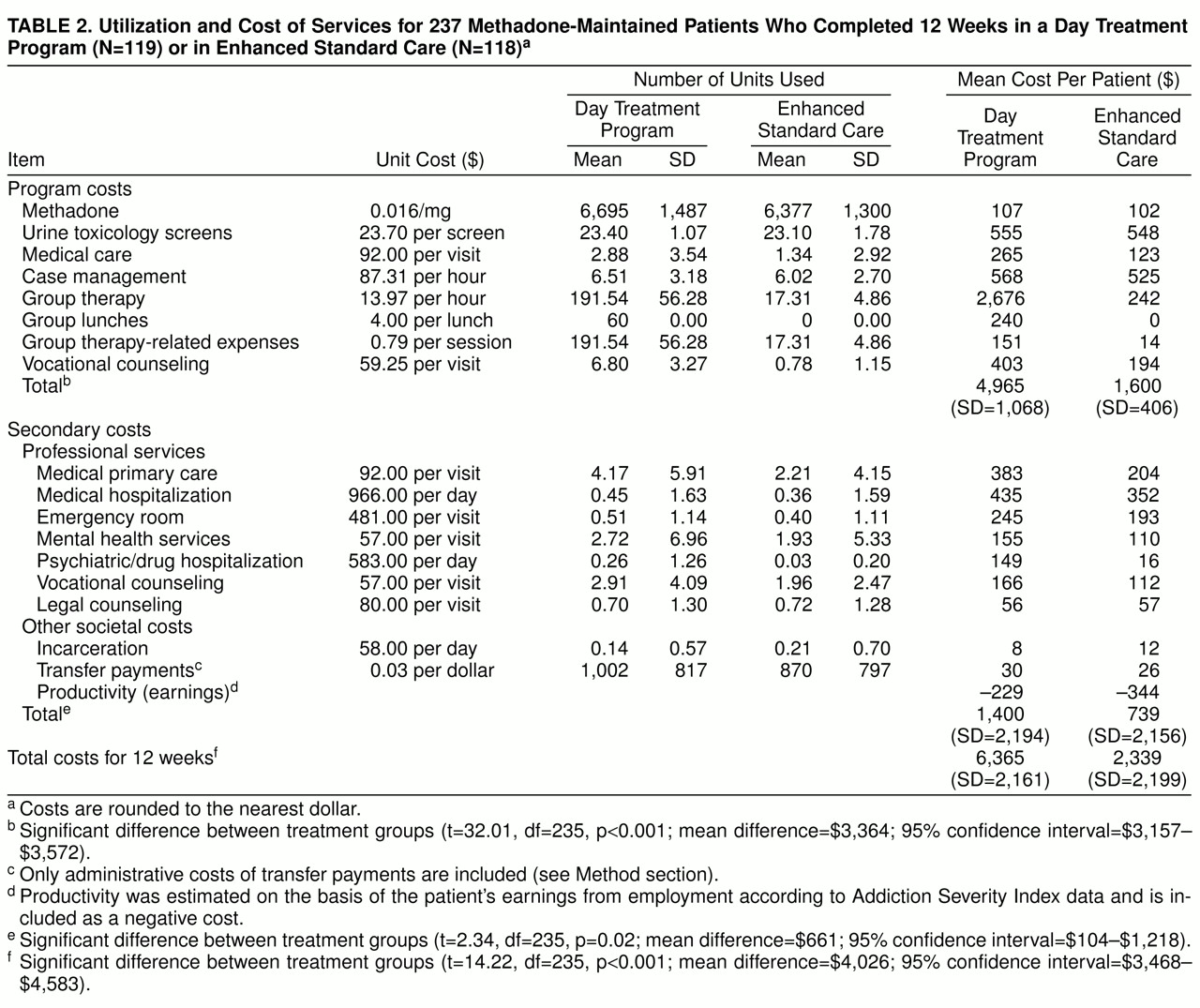
There was no significant difference between the day treatment program and enhanced standard care in methadone dose (day treatment program: mean=81.7 mg/day, SD=17.0; enhanced standard care: mean=78.1 mg/day, SD=14.9; t=1.75, df=232, p=0.08); in the number of days methadone was received out of 84 possible days (day treatment program: mean=81.7 days, SD=3.2; enhanced standard care: mean=81.5 days, SD=3.4; t=0.46, df=234, p=0.64); or in hours of case management (day treatment program: mean=6.51 hours, SD=3.18; enhanced standard care: mean=6.02 hours, SD=2.70; t=1.28, df=230, p=0.20). Patients who completed the day treatment program attended a mean of 191.54 hours (SD=56.28) of day treatment, and patients completing enhanced standard care attended a mean of 17.31 hours (SD=4.86) of skills training groups (t=33.60, df=120, p<0.0001). A multivariate analysis of variance (MANOVA) conducted on the seven Treatment Services Review variables revealed a main effect for treatment intensity: patients assigned to the day treatment program received more services overall than patients assigned to enhanced standard care (F=72.1, df=7, 201, p<0.0001). Subsequent analyses of these seven variables with the use of a significance level of 0.007 after Bonferroni correction revealed that patients assigned to the day treatment program received significantly more medical services (t=8.66, df=172, p<0.001), employment services (t=11.78, df=145, p<0.001), psychological services (t=16.39, df=121, p<0.001), and drug treatment services (t=15.49, df=155, p<0.0001) in the methadone program. Outside the program, day treatment program patients received significantly more medical services (t=2.73, df=207, p<0.007).
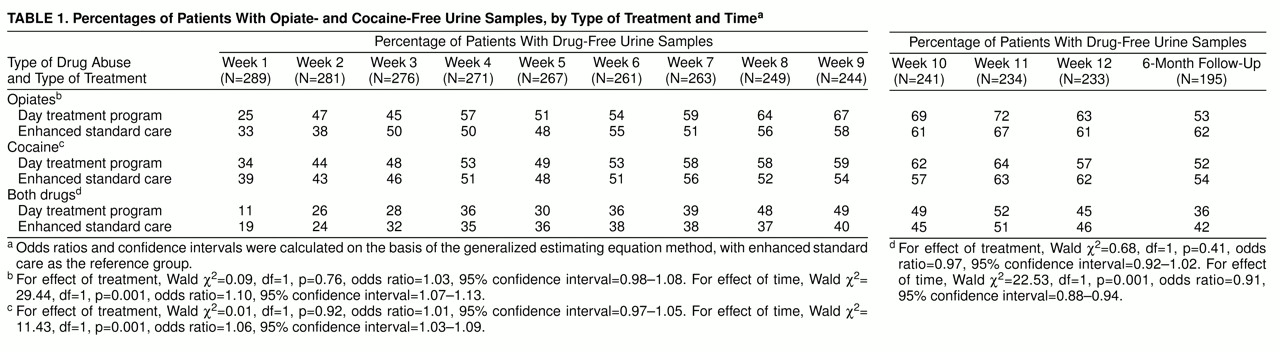
As shown in
table 1, there were no differences between groups in rates of opiate- and cocaine-free urine screens during treatment or at follow-up. There was a significant increase across weeks in the percentage of patients who were abstinent from opiates, from cocaine, or from both drugs (p values <0.001). Follow-up urine data were available for 74% of the patients who completed the 12-week treatment program (75% in the day treatment program; 73% in enhanced standard care). At the follow-up interview, 71% (N=75) of the day treatment program patients and 67% (N=64) of the enhanced standard care patients continued to receive standard methadone maintenance, which included drug counseling and random urine testing. Abstinence status did not change significantly from the end of treatment to 6-month follow-up (McNemar’s test: for cocaine, χ
2=2.27, df=1, p=0.13; for opiates, χ
2=0.39, df=1, p=0.54); 65% of the 85 patients available for follow-up who were abstinent from opiates and cocaine at treatment completion were still abstinent at the 6-month follow-up.
A series of 2 × 3 mixed ANOVAs conducted on Addiction Severity Index and HIV Risk Assessment Battery composite scores revealed no main effects of treatment intensity and no significant treatment intensity-by-time interactions. However, main effects of time were found on two of the seven Addiction Severity Index scores at the 0.007 alpha level with the Bonferroni correction: severity of drug abuse (F=61.62, df=2, 398, p<0.0001) and severity of legal problems (F=26.92, df=2, 398, p<0.001). Both problem areas decreased from pretreatment to posttreatment, with no significant change from posttreatment to 6-month follow-up. Changes on the remaining five Addiction Severity Index scores failed to reach statistical significance (employment problems: F=3.46, p=0.03; medical problems: F=0.26, p=0.77; family/social problems: F=1.36, p=0.26; psychiatric problems: F=0.64, p=0.52; alcohol problems: F=0.84, p=0.43; all df=2, 398).
On the three Risk Assessment Battery composite scores, with a corrected alpha level of <0.02, there were main effects of time on the overall Risk Behaviors Index composite score (F=22.74, df=2, 370, p<0.001), the Drug Risk Index composite score (F=26.03, df=2, 370, p<0.001), and the Sexual Risk Index composite score (F=8.79, df=2, 370, p<0.001). Drug and sexual high-risk behaviors decreased significantly from pretreatment to posttreatment, with further reductions in the overall risk index and drug risk behaviors from posttreatment to 6-month follow-up (overall risk index: F=5.16, df=1, 185, p<0.02; drug risk index: F=11.59, df=1, 185, p<0.001).
At treatment completion, 10.1% (N=12) of the 119 patients who completed the day treatment program and 14.9% (N=17) of the 118 patients who completed enhanced standard care had gained employment, a nonsignificant difference (χ2=1.04, df=1, p=0.33). The difference in number of hours engaged in work or seeking work during the 12-week treatment phase also failed to reach statistical significance (enhanced standard care: mean=71.2 hours, SD=120.7; day treatment program: mean=43.1 hours, SD=81.8; t=1.99, df=211, p=0.05).
A MANOVA conducted on the eight treatment satisfaction ratings revealed a significant interaction between satisfaction and treatment intensity (F=2.56, df=7, 1568, p=0.01). Subsequent univariate analyses, with alpha at <0.006, revealed that patients in the day treatment program were significantly more satisfied with two of eight dimensions: employment counseling (t=2.87, df=219, p=0.005) and leisure time activities (t=2.46, df=221, p=0.01). Differences between the two treatment intensities in satisfaction with the remaining six dimensions failed to reach statistical significance (satisfaction with methadone: t=0.09, df=224, p=0.92; with quality of groups: t=0.44, df=224, p=0.66; with relapse prevention: t=0.52, df=224, p=0.61; with help for medical problems: t=0.30, df=157, p=0.76; with help for family problems: t=0.29, df=222, p=0.77; with community referrals: t=2.87, df=210, p=0.03).