Many psychiatric disorders, including disruptive disorders, anxiety disorders, and depressive disorders, have an onset in childhood or adolescence
(1,
2). Long-term longitudinal studies have shown that those childhood disorders increase the risk of negative outcomes in late adolescence and adulthood
(3–
5), although the course of pathology across the child-to-adult transition still remains unclear
(6). In contrast, the appearance of axis II personality disorders has been attributed primarily to late adolescence and adulthood. Personality pathology logically has its origins in childhood and adolescence
(7); nonetheless, there is limited information available on what characteristics presage adult personality disorders.
Antecedents of adult personality disorders, especially borderline and schizoid disorders, have been traced to personality disorder precursors observed in childhood
(8,
9). Certain adult personality disorders also have been linked empirically to childhood psychiatric disorder, particularly the well-established association between conduct disorder and adult antisocial personality disorder
(3,
5,
10). Less is known about the association between childhood affective disorders and later personality disorder, despite the high co-occurrence of affective disorders and personality disorder in adults, including mood disorders and the emotional dramatic (cluster B) and anxious fearful (cluster C) personality disorders
(11,
12), and anxiety disorders and the odd eccentric (cluster A) and cluster C
(13) personality disorders.
Childhood antecedents of later personality disorder also have been investigated in more representative samples. Adolescent disruptive, anxiety, depressive, and substance use disorders were associated with elevated personality disorder dimensional scores obtained 6 years later in a community sample of young adults
(14). In an epidemiological sample overlapping with the current study sample, behavioral and affective problems and immature social behavior in early and middle childhood heightened the risk of adolescent personality disorder
(15), and disruptive and affective syndromes measured later in childhood and in adolescence increased the risk of personality disorder symptoms in young adulthood
(16).
Childhood psychiatric disorders may precipitate a chain of behaviors and environmental responses that predispose the individual to a more persistent form of adult pathology reflected in axis II personality disorders. This study examined the link between childhood pathology and young adult personality disorder in an epidemiological sample. It is singular in that predictive effects of both prior axis I disorders and earlier manifestations of personality pathology on young adult personality disorder can be examined prospectively at the diagnostic level. In addition, the earlier focus on the outcomes of childhood disruptive disorders is broadened to include outcomes of childhood affective disorders. On the basis of prior evidence we anticipated associations between disruptive disorders and all personality disorder clusters
(10,
14,
17), between anxiety disorders and personality disorder in clusters A and C
(13,
14), and between major depression and personality disorder in clusters B and C
(11,
12,
14). Because comorbid disorders are reported to be more debilitating than are outcomes of single disorders
(18), we also examined whether the odds of a personality disorder in young adulthood are higher among youths with co-occurring axis I-axis II disorders than among youths with a disorder on a single axis. The following questions were addressed:
Do childhood psychiatric disorders increase the risk of adult personality disorder, and, if so, is that risk independent of adolescent personality disorder?
Does comorbidity between prior psychiatric and personality disorders heighten the risk of later personality disorder beyond their separate effects?
METHOD
Subjects
Subjects were drawn from the Children in the Community study, a longitudinal investigation of risk factors and childhood psychopathology. In 1975, 976 families with a child between 1 and 10 years old were randomly sampled from two upstate New York counties (85% of those asked)
(19). In the first follow-up in 1983, 722 families (74%) were reinterviewed, 156 families (16%) were lost to follow-up, and 49 families (5%) refused to continue participation; interviews were not conducted with the remaining 49 families because of study time constraints (44 families), death of the study child (three families), or severe mental retardation in the study child (two families). Because those lost to follow-up were disproportionately among the urban poor, 54 new families were randomly sampled from urban poverty areas in the original two counties and were added to the 1983 sample, for a total of 776 families. According to 1980 U.S. census data, the 1983 sample is closely representative of families in the sampled counties on income and family structure, urbanicity of residence, and other demographic characteristics
(20).
The 1985 follow-up included 734 families (94.7%) from the 1983 follow-up and 42 families from the original sample who were located but not reinterviewed in 1983. In all, 818 families were seen for the 1983 or 1985 interviews; of these, 714 (87.3%) participated in a third follow-up in 1992. The current study used data from families who participated in 1992 and in at least one prior follow-up. Youths from the 104 families who did not participate in 1992 were compared to youths from the 714 families who did, with regard to demographic characteristics and diagnostic measures used in the current study. Nonparticipants and participants, respectively, did not vary statistically in age at the time of the 1983 follow-up (13.7 versus 13.7 years) (two-tailed t=–0.06, df=1, 774, p=0.95) or the 1985 follow-up (16.4 versus 16.3 years) (two-tailed t=–0.87, df=1, 774, p=0.39) or in rates of disruptive disorders (14.4% versus 11.3%) (χ2=0.83, df=1, p=0.36), anxiety disorders (9.6% versus 14.4%) (χ2=1.76, df=1, p=0.18), major depression (4.8% versus 5.7%) (χ2=0.15, df=1, p=0.70), cluster A personality disorders (8.1% versus 6.8%) (χ2=0.23, df=1, p=0.63), cluster B personality disorders (7.1% versus 7.2%) (χ2=0.003, df=1, p=0.96), or cluster C personality disorders (8.1% versus 7.7%) (χ2=0.02, df=1, p=0.88). However, the proportion of boys was greater in nonparticipants than in participants (64.4% versus 49.0%) (χ2=8.62, df=1, p=0.003).
The current sample was limited to the 551 youths who were 16 years of age or younger when the 1983 assessment took place. Most subjects were white (91%) and Catholic (59%), and 48% were male. Mean age was 12.7 years (SD=2.1) in 1983, 15.2 years (SD=2.1) in 1985, and 21.1 years in 1992 (SD=2.2).
Procedure
After a full explanation of study procedures, written informed consent was obtained from all participating mothers and from participating youths 13 or more years of age. Interviews of mothers and youths were conducted simultaneously but separately in their homes by pairs of trained lay interviewers. In all three follow-ups, mothers responded to an interview covering family background and parenting and to a diagnostic interview and questionnaire about the study child that covered psychiatric and personality pathology. Youths were interviewed on parallel diagnostic instruments and responded to interviews and self-report inventories about friends, school, and work.
Measures
In the 1983 and 1985 follow-ups, DSM-III-R axis I diagnoses, including attention deficit hyperactivity disorder (ADHD), conduct disorder, oppositional defiant disorder, overanxious disorder, separation anxiety disorder, social phobia, and major depressive disorder, were derived from mothers’ and children’s responses to the Diagnostic Interview Schedule for Children
(21). Information obtained from the Diagnostic Interview Schedule for Children was augmented with questions asked elsewhere in the protocol in order to adequately assess DSM-III-R symptoms. In keeping with current best practice, a positive response from either parent or youth was taken as evidence of symptom presence. In order to counteract known problems of specificity in diagnostic interviews, youths who met diagnostic criteria and had scaled symptom and impairment scores of two or more standard deviations above the sample mean were considered to have each disorder. Axis I disorders were grouped into disruptive disorders (ADHD, conduct disorder, oppositional defiant disorder), anxiety disorders (overanxious disorder, separation anxiety disorder, social phobia), and major depressive disorder in order to increase statistical power (by increasing group size) and to reduce type I error (by reducing the number of independent variables). Thus, some youths were assigned to more than one disorder group.
In all three follow-up waves, DSM-III-R axis II diagnoses, including antisocial, avoidant, borderline, dependent, histrionic, narcissistic, obsessive-compulsive, paranoid, passive-aggressive, schizoid, and schizotypal personality disorder, were derived from mothers’ and youths’ responses to interview items written for that purpose
(17) or adapted for adolescent respondents from the Personality Diagnostic Questionnaire
(22) or the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II)
(23). It was anticipated that the instrument, like its predecessors, would have high sensitivity but low to moderate specificity. To address this problem, only youths who met diagnostic criteria in both the 1983 and 1985 assessments (average interval=2.5 years) for a personality disorder in the same personality disorder cluster were identified as having a personality disorder. The validity of personality disorder diagnoses made before late adolescence in this study was shown by the prediction of subsequent negative life outcomes, including poor occupational and educational achievement and later deviance
(17). Assessment of young adult personality disorder was cross-sectional in nature; however, items, as in the Personality Diagnostic Questionnaire and SCID-II, were worded to elicit enduring deviant characteristics. Personality disorder diagnoses were grouped according to DSM-III-R clusters A (paranoid, schizoid, schizotypal), B (antisocial, borderline, histrionic, narcissistic), and C (avoidant, dependent, passive-aggressive). Obsessive-compulsive personality disorder, as assessed, did not relate to dysfunctional outcomes that characterized all other diagnoses; therefore, it was not included in cluster C. Antisocial personality disorder is not measured in children; therefore, it was measured and included in cluster B diagnoses only in the 1992 adult follow-up. As with the axis I disorders, youths could be assigned to more than one personality disorder cluster.
Statistical Analysis
Logistic regression analyses estimated effects when age and sex were controlled. For each outcome, predictors were entered into the equation to assess effects of prior disruptive disorders, anxiety disorders, major depression, adolescent personality disorder in the same cluster, and comorbidity of axis I and axis II disorders. A high rate of comorbidity precluded adequate statistical tests of independent effects of multiple axis II groups in the same equation; thus, equations include consideration of adolescent personality disorder in the same cluster only.
RESULTS
Prevalence of Disorders
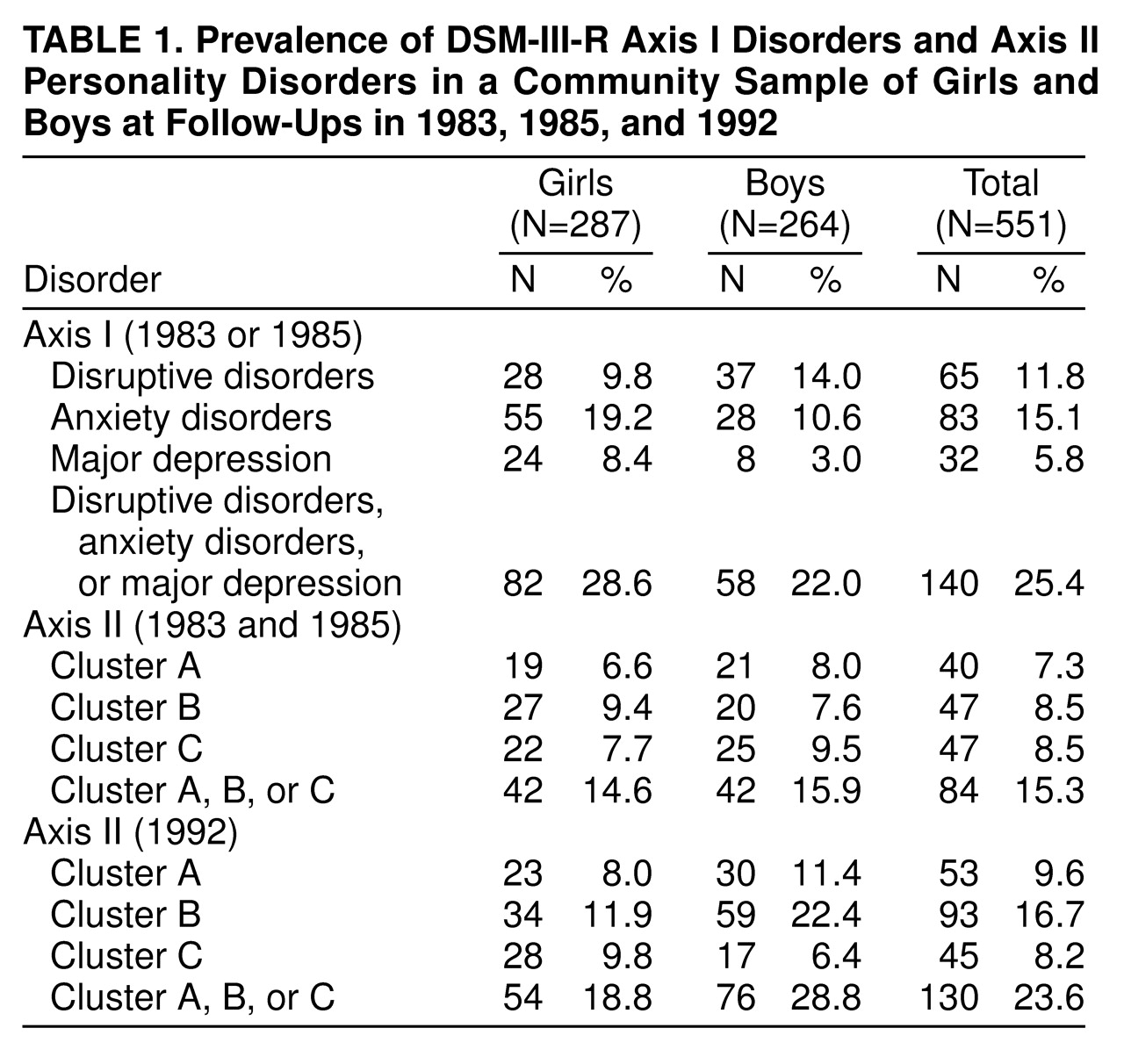
The prevalence of all disorders is shown in
Table 1 for the total sample and separately for girls and boys. Yates’s corrected chi-square values for significant sex differences are given in the text.
Axis I psychiatric disorders. By 18 years of age, almost 12% of the sample had a disruptive disorder at one or both youth assessments, and about half as many had major depression. About 15% had an anxiety disorder. Overall, about one of four youths was diagnosed with one or more disorders. Compared to boys, girls had significantly higher rates of anxiety disorders (19.2% versus 10.6%) (χ2=7.22, df=1, p<0.01) and major depression (8.4% versus 3.0%) (χ2=6.21, df=1, p<0.05). Boys had a nonsignificantly higher rate of disruptive disorders than did girls (14.0% versus 9.8%) (χ2=2.01, df=1, p=0.16), including more ADHD (6.8% versus 4.2%) (χ2=1.38, df=1, p=0.24) and significantly more conduct disorder (8.0% versus 2.4%) (χ2=7.57, df=1, p<0.01) but lower rates of oppositional defiant disorder (4.9% versus 8.0%) (χ2=1.67, df=1, p=0.20).
Axis II personality disorder clusters. Cluster A personality disorder was diagnosed in both youth assessments for 7.3% of the sample; rates for cluster B and cluster C personality disorders were slightly higher. About 15% of youths had a personality disorder before young adulthood, with rates comparable across gender. The prevalence of personality disorder in young adults was 9.6% for cluster A, 16.7% for cluster B, and 8.2% for cluster C. Close to one of four young adults had a personality disorder. Female subjects had fewer personality disorders (18.8% versus 28.8%) (χ2=7.04, df=1, p<0.01) and fewer cluster B disorders (11.9% versus 22.4%) (χ2=10.07, df=1, p<0.01). Those differences were due to differential antisocial personality disorder: removal of that personality disorder resulted in no significant sex difference in cluster B (10.1% of female subjects versus 13.3% of male subjects) (χ2=1.04, df=1, p=0.31) or in any personality disorder.
Relative risks of young adult personality disorder in youths previously diagnosed. Relative risks of young adult personality disorders were as follows: for youths with and without a corresponding personality disorder: 30.0%÷8.0%=3.8 for cluster A, 42.6%÷14.5%=2.9 for cluster B, and 23.4%÷6.8%=3.4 for cluster C; for youths with and without disruptive disorders: 26.2%÷7.4%=3.5 for cluster A, 46.2%÷13.0%=3.6 for cluster B, and 23.1%÷6.2%=3.7 for cluster C; for youths with and without anxiety disorders: 24.1%÷7.1%=3.4 for cluster A, 21.7%÷16.0%=1.4 for cluster B, and 16.9%÷6.6%=2.6 for cluster C; and for youths with and without major depression: 21.9%÷8.9%=2.5 for cluster A, 46.9%÷15.0%=3.1 for cluster B, and 34.4%÷6.6%=5.2 for cluster C.
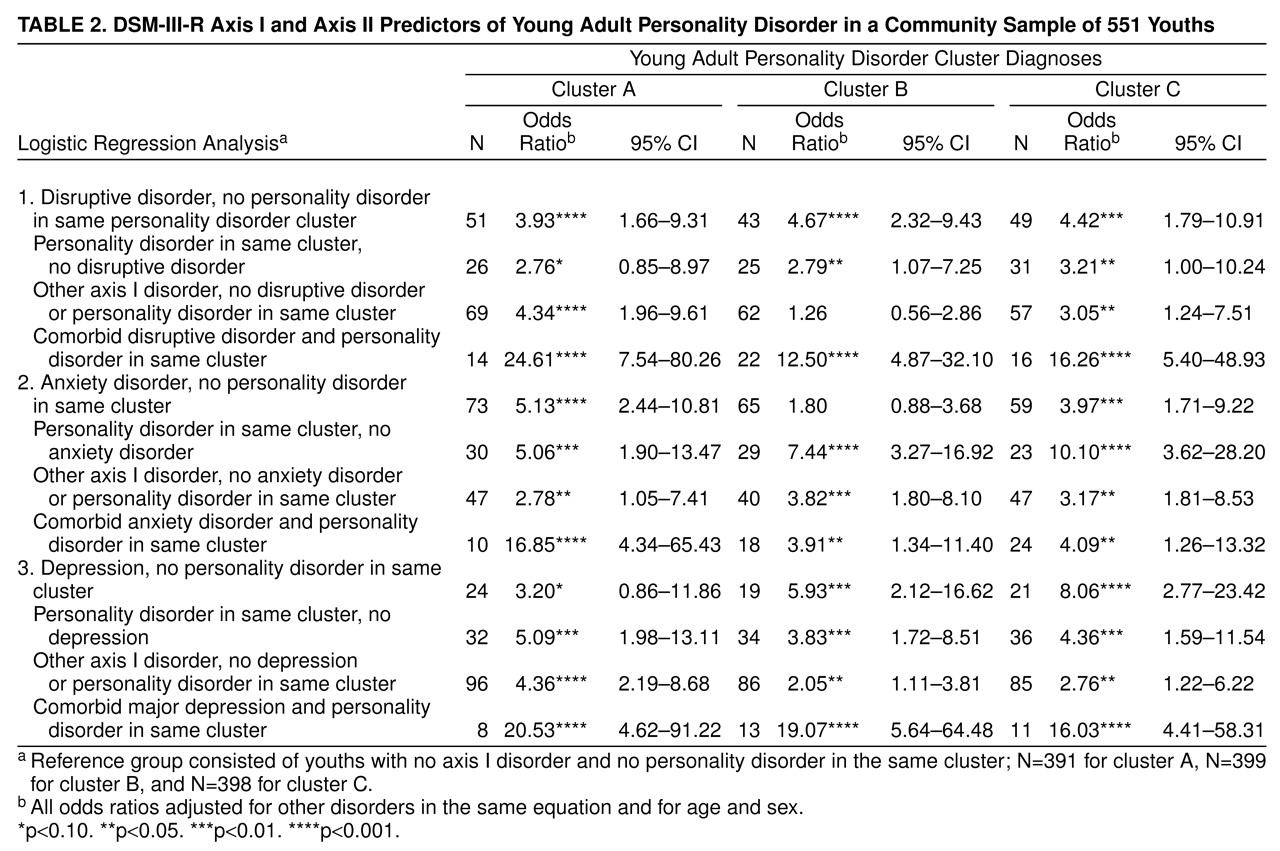
Predictive Effects
Table 2 gives the adjusted odds for each identified diagnostic group compared to undiagnosed youths, partialing the effects of the other diagnostic groups in the set, age, and sex. Overall, the odds of young adult personality disorder increased substantially with an adolescent personality disorder in the same cluster. As expected, there also were significant effects of a prior axis I disorder on young adult personality disorder. Disruptive disorder increased the odds of personality disorder in clusters A, B, and C by about fourfold; anxiety disorder increased the odds of personality disorder in clusters A and C by, respectively, fivefold and fourfold; and major depression increased the odds of personality disorder in clusters B and C by, respectively, sixfold and eightfold. In seven of the nine equations, the odds of young adult personality disorder were higher in the group with comorbid axis I and axis II disorders than in the other groups; however, because of small numbers, the difference was statistically significant only when compared with the undiagnosed group. That comorbid effect was not seen in the case of anxiety disorders and a cluster B or C personality disorder, where the odds were nonsignificantly higher for adolescent personality disorder without anxiety disorders.
Effects of Increasing Number of Disorders
To determine whether multiple disorder effects were attributable to a simple severity effect of more symptoms, in contrast to more specific influences, the number of adolescent diagnostic groups (clusters A, B, and C; disruptive disorders; anxiety disorders; major depression) was counted for each youth and regressed against the three outcomes. With each addition of a comorbid group, the odds nearly doubled for a young adult personality disorder in cluster A (odds ratio=1.90, 95% confidence interval [CI]=1.55–2.34), cluster B (odds ratio=1.70, 95% CI=1.41–2.04), and cluster C (odds ratio=1.85, 95% CI=1.50–2.29). The impact of these findings is seen clearly with rates of young adult personality disorder in groups based on number of prior diagnoses: for youths with none (N=380), one (N=96), two or three (N=59), and four or more (N=16) diagnoses, rates of young adult personality disorder were, respectively, 4.5%, 15.6%, 20.3%, and 56.3% for cluster A personality disorders; 11.6%, 21.9%, 33.9%, and 50.0% for cluster B disorders; and 4.5%, 10.4%, 20.3%, and 37.5% for cluster C disorders. Thus, some clear indication of a severity effect was seen. In an effort to determine whether there was any attributable specificity, we contrasted the chi-square value of the logistic regression model for the index of number of adolescent diagnostic groups with the chi-square value of the model in which the four diagnostic groups were considered separately with three more degrees of freedom. Given the three additional degrees of freedom, the chi-square value difference required for a significance level of <0.01 is 11.3. For clusters A and C those differences were small (4.05 and 4.34, respectively) and, had this been a true nested design, not significant. However, for cluster B the chi-square difference was 20.5; thus, we may conclude that the risk of a cluster B disorder in young adulthood is not merely a severity effect of the number of adolescent disorders.
DISCUSSION
Effects of Adolescent Personality Disorder
Adolescent personality disorder predicted young adult personality disorder independent of axis I disorders; these findings add evidence of the validity of personality disorder diagnoses during early and middle adolescence. There remains much controversy over whether personality disorder symptoms are transitory during that period and whether symptoms shown in adolescence will have as negative a prognosis as the same symptoms in adults. A developmental perspective on personality disorder can be traced to Erikson
(24), who attributed the origins of later personality pathology to poor resolution of the increasing psychosocial demands of childhood and adolescence. Thus, late adolescent and adult disturbances in role performance and interpersonal relationships, key features of all personality disorders, may, in effect, be the cumulative outcome of severe developmental failure.
Effects of Adolescent Axis I Disorders
Disruptive disorders. Disruptive disorders were strong predictors of all personality disorders, as is consistent with previous findings of long-term negative life outcomes suggestive of personality pathology in youths with disruptive disorders. Adult antisocial behaviors and criminality have been attributed to childhood conduct and ADHD
(3,
5). Lewinsohn et al.
(14) found an increase in elevated dimensional scores for clusters A and B personality disorders in young adults who had a disruptive disorder in adolescence. Adolescents referred for disruptive disorders were found to have elevated rates of personality disorder, especially in clusters B and C, 6 years later
(10). Others have noted a link between childhood disruptive disorder and later more pervasive maladaptive functioning in a number of adult life domains, including the workplace, social relationships, love and marriage, and parenting
(3,
5).
Anxiety disorders. Anxiety disorders predicted young adult personality disorder in clusters A and C. Lewinsohn et al.
(14) reported a strong association between adolescent anxiety disorders and young adult paranoid, schizoid, and schizotypal personality disorders and noted that this was one of the two strongest links found between adolescent axis I disorders and young adult personality disorder. Anxiety disorder also has been noted to be a comorbid feature of paranoid and schizotypal personality disorders in an adult clinical sample
(25). Essential characteristics of cluster A personality disorders are misinterpretation of others’ behaviors (paranoid), indifference to social relationships (schizoid), and deficits in interpersonal relatedness and peculiarities of behavior (schizotypal). The main features of two of the childhood anxiety disorders examined here, discomfort in social situations outside the immediate family (separation anxiety) and persistent fear and avoidance of social situations perceived as threatening (social phobia), may act as deterrents to social involvement. Consequently, the number and type of social interactions would be restricted, making them less anxiety provoking. It may be that a lessening of anxiety when social avoidant behaviors are implemented reinforces their repetition, thus fostering an arrest of social development and, subsequently, a more traitlike pathology. The predictive effect of axis I anxiety disorders on the anxious fearful personality disorders in cluster C suggests that similar mechanisms may be operating, given the more persistent behavioral pattern of reduced and poorly negotiated social interactions in individuals with a cluster C personality disorder.
Major depression. Despite its low prevalence, major depression was a strong predictor of young adult personality disorders in clusters B and C. Childhood depression has been implicated in a number of diverse short- and long-term outcomes, including recurrent depressive episodes, suicidal behavior, conduct problems, substance abuse, personality pathology, and disturbed role performance in adult work and social domains
(26). As with disruptive and anxiety disorders, impaired interpersonal relationships and global functioning co-occur with childhood depression and may continue after the depressive episode remits
(27,
28). Given the 7–9-month mean duration of a depressive episode in childhood
(28,
29), impaired functioning may be maintained for long periods of time, thus fostering more persistent maladaptive behaviors. Findings here underscore the serious nature of severe childhood depression and suggest that although the specific consequences may vary, later role performance in adulthood may be seriously compromised.
Effects of Axis I-Axis II Comorbidity
Compared to youths with a disorder on a single axis, the odds of young adult personality disorder were substantially higher in youths with personality disorder and co-occurring disruptive disorder or major depression and in youths with cluster A personality disorder and a co-occurring anxiety disorder. That finding is supported in part by high levels of comorbid depressive and anxiety disorders reported in young adult patient samples with borderline and other axis II personality disorders
(30). The combined effects of clinical level impairment indicative of personality disorder and the more florid pathology of an axis I disorder may be more likely to persist into adulthood than the separate effect of each. However, small cell sizes for comorbid disorders precluded testing for statistically reliable differences; thus, findings should be considered preliminary and in need of replication.
Severity Effect
There was evidence of a severity effect of increasing number of adolescent disorders on young adult personality disorder, suggesting that more is, indeed, worse; however, there also was some indication that cluster B personality disorders were not merely an outcome of multiple disorders. Impaired functioning is a feature of psychiatric disorder; with multiple disorders, functioning may be compromised to a greater extent. Consequently, the cognitive and behavioral resources needed to cope with the psychosocial demands of childhood and adolescence may be diminished, thus contributing to negative life outcomes in adulthood.
CONCLUSIONS
In sum, we found that childhood personality disorder and axis I disorder are independent risks for adult personality disorder. An important implication of those findings stems from the similar consequences of axis I disorders and personality disorder. Are the characteristics that differentiate the axes more blurred than was previously thought? By definition, the later identification and greater endurance of personality disorder relative to axis I disorders with childhood onset separate the axes. Yet the progression of childhood conduct disorder to antisocial disorder suggests that personality disorders may, indeed, have their origins in earlier developmental stages, whereas the recurrence of childhood and adolescent depressive episodes implies that axis I disorders may be perpetuated into adulthood. Findings here suggest an underlying characteristic or set of characteristics that may operate in both axis I and axis II pathology. Adolescent personality disorder implies a persistent maladaptive mode of thinking and acting that may delay more mature role functioning in the transition to adulthood. Severe psychiatric disorder in childhood or adolescence may interfere with developmental tasks, particularly those that are concerned with the processing of social information and the acquisition of interpersonal skills
(31), so that the risk of later role disturbance and social dysfunction is heightened. Thus, as in any learning situation, when the basic foundation skills are weak, attaining more mature competence may be compromised. It may be that childhood or adolescent axis I disorders, themselves often a result of negative life experiences, set in motion a pattern of maladaptive social behaviors that persist as more traitlike characteristics. It also may be that deficits or impairments in social adaptation (due to genetic and contextual factors) precede both axis I and axis II disorders. Consequently, an increasingly negative reaction from the environment may foster a more maladaptive response, which in time becomes an integral part of the personality system. These findings have implications for intervention at the childhood level in order to circumvent the added risk of subsequent personality disorder in young adulthood. Because axis I disorders in children may be more amenable to treatment than is adult personality disorder, early treatment among at-risk children would be desirable.
Most of the study sample was white (91%) and Catholic (59%); thus, caution should be exercised when generalizing the findings to other groups. Assessment of axis I disorders focused on the year before the interview; consequently, lifetime prevalence by age 18 was not obtained. Thus, it is probable that some youths who met criteria for axis I diagnoses were not identified, which serves to depress the effects of prior disorder on subsequent pathology. Finally, other axis I disorders not used in the analyses may have influenced the outcome; however, other disorders typically were rare (e.g., eating disorders, schizophrenia) or did not meet severity criteria (e.g., simple phobia).
This study used diagnoses that were obtained prospectively from multiple informants in a randomly selected community sample over a 10-year interval. In addition, stringent diagnostic criteria were imposed: axis I diagnoses were at the severe level cutoff and included diagnosis-specific impairment criteria, and, for an adolescent axis II diagnosis, diagnostic criteria were met in both 1983 and 1985.