Since the introduction of the construct of expressed emotion more than 40 years ago, studies have repeatedly shown that this construct taps family attitudes and behaviors predictive of psychiatric relapse. Assessed by using the Camberwell Family Interview
(1,
2), expressed emotion is not a measure of overall emotionality but, rather, a measure of the extent to which a family member expresses critical, hostile, and/or emotionally overinvolved attitudes toward a psychiatric patient during an interview conducted in the patient’s absence. When patients return home from the hospital to live with relatives who are rated as high in expressed emotion, relapse is two to three times more likely to occur in the following 9–12 months
(3,
4).
Expressed emotion was initially developed and validated as a predictor of relapse in patients with schizophrenia
(5,
6). However, subsequent work has established that the construct has predictive validity across a variety of psychiatric and medical conditions, including mood disorders
(6–
8), alcoholism
(9), obesity
(10), and diabetes
(11). A recent meta-analysis demonstrated that expressed emotion is an even stronger predictor of poor outcome for patients with mood disorders and eating disorders than it is for patients with schizophrenia
(12). However, although expressed emotion has been well studied across a range of axis I disorders, to our knowledge no research to date has explored the relevance of the expressed emotion construct for axis II diagnoses. In this article we report the first data concerning the predictive validity of expressed emotion for borderline personality disorder.
Borderline personality disorder is a diagnosis that is characterized by complex and intense emotional experiences as well as by impulsivity, suicidal and parasuicidal behavior, and fears of abandonment. The etiology of the disorder is generally viewed as multidimensional, involving a biological or constitutional component coupled with inadequate parenting. The biological factors are explained in different ways depending on the particular theoretical orientation. For example, Kernberg
(13) views the constitutional factor as an excess of aggression. This may be experienced by the patient and others in their environment as hostility, outbursts of rage, and extreme irritability. Linehan
(14), on the other hand, regards the constitutional factor as a deficit in emotion regulation. This emotional vulnerability renders the individual feeling incapable at times of effectively managing his or her feelings, which often leads to maladaptive coping mechanisms. Consistent with both of these explanations is the growing evidence implicating serotonin in borderline personality disorder
(15–
17).
Although clinicians and researchers do not always agree on the nature of the underlying constitutional diathesis, there is general agreement about the importance of environmental factors in the development of borderline personality disorder. Both Kernberg
(13) and Gunderson
(18) have hypothesized that patients with borderline personality disorder grew up in overinvolved and hostile environments. These environments strike some as “reminiscent of the concept of expressed emotion”
(19, p. 166). Moreover, retrospective studies have reported that overinvolvement, hostility, separation, neglect, and physical and sexual abuse were often salient in the early parental relationships of patients with borderline personality disorder
(20–
23). Linehan
(14) coined the term “invalidating environment” to describe the early home environments of patients with borderline personality disorder. An invalidating environment is described as an atmosphere that does not acknowledge or tolerate negative feelings and that is also highly critical and underinvolved emotionally. Like others, Linehan views this type of family environment as “similar to the pattern of high expressed emotion”
(14, p. 50).
Borderline personality disorder has become the most researched of the axis II disorders in the last 10 years
(24,
25). However, the main emphasis of this research has been on the early childhood experiences and perceptions of patients. This may explain why there are so few data on the relationship between familial/environmental variables and the course of established borderline personality disorder. The present investigation was designed to explore the association between expressed emotion and clinical outcome of inpatients with borderline personality disorder in an effort to learn more about the role of the family in this little-studied area.
METHOD
Subjects
Subjects were recruited from three inpatient units at The New York Hospital/Cornell Medical Center–Westchester Division in White Plains, N.Y. All consecutively admitted patients were screened and considered eligible for participation if they 1) met DSM-III-R criteria for borderline personality disorder, 2) were between 16 and 50 years of age, and 3) lived with or had regular contact with their family of origin or a significant other such as a spouse. After complete description of the study to subjects, written informed consent was obtained. Each patient also designated a key relative or relatives to be contacted and included in the study. These family members also provided written informed consent.
An initial study group of 41 inpatients with borderline personality disorder was recruited. Of these, 35 (85%) contributed data to the follow-up study. The mean age of these patients (25 women and 10 men) was 29.6 years (SD=8.4), and the majority (74%, N=26) had never been married. The mean age of their relatives (26 [74%] of whom were parents) was 52.4 years (SD=9.9). According to the Goldthorpe and Hope classification scheme
(26), which rates socioeconomic status on a 1 (high) to 36 (low) scale, the mean socioeconomic status of the study group was 21.6 (SD=11.0). Socioeconomic status ratings in this range represent such occupations as clerical worker and cashier. Patients had typically been ill for a mean of 6.3 years (SD=5.8) and had a mean number of 5.9 previous psychiatric hospitalizations (SD=5.9). On admission to the hospital their mean score on the Global Assessment Scale (GAS) (27) reflected considerable impairment in global functioning (mean=38.3, SD=7.4).
Subjects in the follow-up group did not differ from subjects in the original study group with respect to age, sociodemographic status, number of previous hospitalizations, GAS score, or duration of hospitalization. However, several differences in their relatives were observed with respect to the expressed emotion variables. The 35 subjects for whom follow-up data were available had relatives who were more critical (13.1 versus 6.3 criticisms) (t=2.52, df=39, p<0.05), more emotionally overinvolved (1.6 versus 0.03) (t=3.82, df=39, p<0.001), and made more positive remarks about them (3.9 versus 0.7) (t=4.39, df=39, p<0.001) than did the relatives of the six subjects who were not available for follow-up. The relatives of the patients who were not included in the follow-up study thus appear to have been less engaged than the relatives of the patients who were included in the follow-up study.
Diagnostic Assessment
Axis II diagnoses were established by using the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II)
(28). This was administered to patients in its entirety. In addition, patients were interviewed with the mood disorders, psychotic disorders, and eating disorders modules of the Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P)
(29) to identify any comorbid axis I pathology.
All clinical assessments were administered and scored by two experienced clinicians (with 10 and 15 years of psychiatric experience, respectively) and one psychology intern who was trained by the senior clinicians. For the seven patients who refused a SCID interview or were discharged before it could be completed, data from the patient’s therapist together with hospital records were used to provide additional relevant clinical information.
Further information about the severity of borderline symptoms was obtained for a subgroup of 24 patients who were involved in another research protocol by using the Borderline Personality Disorder Dimensional Score Interview (Clarkin et al., unpublished 1991 measure). This is a clinician-administered interview that rates the severity of the patient’s difficulties across a range of domains relevant to borderline personality disorder (e.g., unstable interpersonal relations and labile affect). The Borderline Personality Disorder Dimensional Score Interview was given after the SCID-II had been completed and was administered by the same clinical interviewers. All interviewers were trained in the administration and scoring of the Borderline Personality Disorder Dimensional Score Interview. Reliability data for the SCID-P and the SCID-II indicated that interrater agreement across the three raters at the level of symptom ratings was good for both axis I disorders (mean intraclass correlation coefficient [ICC]=0.91, range=0.87–0.94) and axis II disorders (mean ICC=0.88, range=0.85–0.91).
Expressed Emotion
Expressed emotion was assessed by using the Camberwell Family Interview
(2). This is a semistructured interview that assesses the attitudes and feelings expressed by a key relative about the patient. The Camberwell Family Interview, which is conducted in the absence of the patient, asks the relative about events in the home in the 3 months preceding a psychiatric hospitalization. It also obtains information about the patient’s psychiatric history and recent symptoms. The interview lasts between 1 and 2 hours and is audiotaped for later coding.
The three major expressed emotion scales are criticism, hostility, and emotional overinvolvement. Critical remarks reflect frank disapproval or dislike of something the patient does and are rated on the basis of either their content or because of voice tone changes that occur in the relative’s speech during the comment. Hostility is a more extreme form of criticism and is rated when there is a more generalized negative feeling toward the patient or when there is evidence of rejection. Finally, emotional overinvolvement reflects a variety of extreme behaviors, including an exaggerated emotional response to the illness, devoted or self-sacrificing behavior, dramatization, or overprotective behavior on the part of the relative.
In this study, all Camberwell Family Interviews were conducted by interviewers who had received appropriate training and were coded by an independent rater who had been trained to achieve the conventionally accepted level of reliability (minimum ICC=0.70) on each of the three major expressed emotion scales.
Follow-Up Assessments
One year after they had been discharged from the hospital, all patients were contacted by telephone and interviewed about the symptoms and problems they had experienced in the past year. To increase the reliability of the outcome assessments, patients’ relatives were also interviewed and asked to provide information about the patients’ symptoms and level of functioning since leaving the hospital. The follow-up interview (Hooley and Hoffman, unpublished 1995 measure) was designed to cover a wide range of symptoms and behaviors relevant to borderline personality disorder, including mood symptoms and suicidality, self-destructive behavior, anger, impulsivity, and abandonment concerns. In addition, information about the patients’ level of functioning across a variety of domains (e.g., job, school, and interpersonal relationships) during the follow-up period was also obtained, as was information about any rehospitalizations or visits to an emergency room. All interviews were conducted by telephone and audiotaped for later coding.
The taped interviews were coded by the two of us, and the information from these ratings was reduced to a global rating of clinical outcome on a 5-point scale. The points on this scale ranged from 1=sustained remission to 5=rehospitalization. In addition, the patient’s lowest level of functioning during the follow-up period was also rated by using the GAS. Because one of us (P.D.H.) was familiar with most of the patients and was not blind to expressed emotion, the other (J.M.H.), who was blind to all patient information, was used as the primary rater in cases of disagreement. Interrater agreement between the two raters, based on 21 cases, was high for both the global outcome scale (ICC=0.97) and the GAS (ICC=0.92).
RESULTS
Clinical Outcome in Borderline Personality Disorder
In general, and consistent with clinical expectation, the overall outcome of the patients was quite poor. More than half (54% [N=19]) of the patients were rehospitalized during the 1-year follow-up. One patient (3%) received emergency room care without hospitalization, and four (11%) continued to exhibit clinically significant symptoms (e.g., continued depression and extreme behavior when angry), although they received no inpatient or emergency room treatment.
Only one of the patients (3%) was considered to have shown a full remission of symptoms with no functional impairment, although 10, a substantial minority (29%), did improve to the point where they had only minor impairment. Examples of such impairment included occasional eating binges, not currently having a job, some problems with motivation, or difficulties in one close relationship. Thus, approximately two-thirds of the patients did poorly, and only one-third of the patients did relatively well. Given that the average length of inpatient treatment for the patients in our study was 5.6 months (SD=3.5) (most of the patients were receiving Medicare or Medicaid), these data highlight the chronic nature of borderline personality disorder.
Demographic and Clinical Predictors of Clinical Outcome
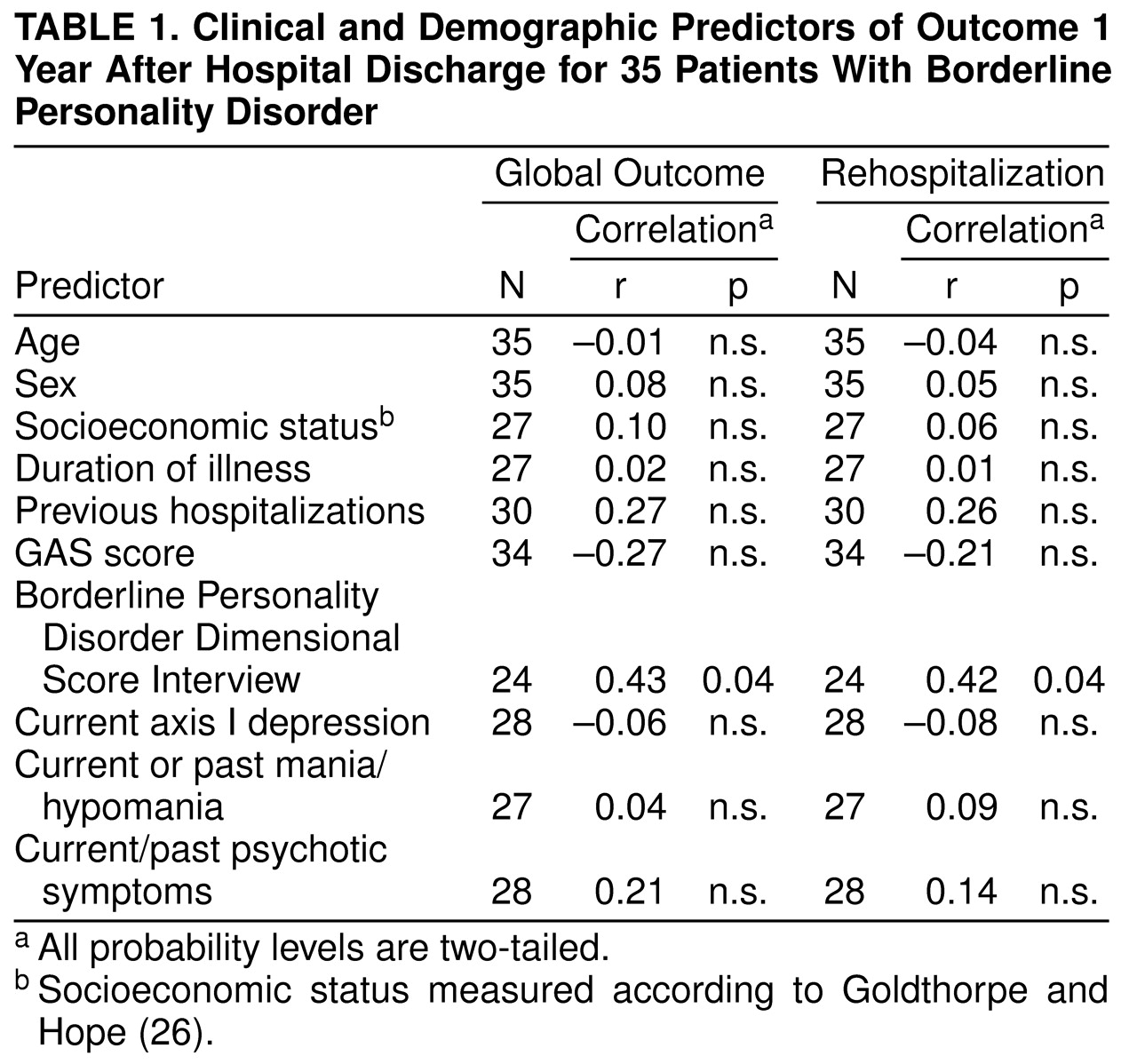
We conducted a series of analyses designed to identify clinical or demographic predictors of poor outcome in our patient group. For simplicity and to facilitate comparisons with other research samples, these are presented as simple correlations in
Table 1. Outcome was operationalized as either as 1) score on the 5-point global outcome scale or 2) readmission to a psychiatric hospital during the 1-year follow-up period.
As is apparent from
Table 1, age, sociodemographic status, duration of illness, initial level of functioning on the GAS, and several other clinical and demographic variables all failed to predict 1-year outcome. The only clinical variable that was significantly associated with how patients fared over the follow-up period was the Borderline Personality Disorder Dimensional Score Interview. The more severe patients’ borderline symptoms were during the index hospitalization, the more likely patients were to do poorly in the following year. However, neither an axis I diagnosis of current major depression (present in 19 [68%] of 28 patients), current or past history of mania or hypomania (present in 11 [41%] of 27 patients), nor previous or current psychotic symptoms such as somatic delusions or olfactory hallucinations (present in 12 [43%] of 28 patients) was significantly predictive of 1-year clinical outcome.
Expressed Emotion
When more than one family member received the Camberwell Family Interview, we followed the convention of selecting the ratings for the most highly critical relative for use in the statistical analyses. This allowed the number of relatives to be equal to the number of patients and was important for the integrity of the statistical analyses. Using this approach, we found that the mean frequency of criticism among the 35 relatives was 13.1 (SD=10.6). Hostility was present in 16 (46%) of the relatives (mean=1.1, SD=1.4), and 10 (29%) of the relatives were rated as high (rating of 3 or more) in emotional overinvolvement (mean=1.5, SD=1.5). The mean warmth rating was 2.5 (SD=1.5), and the mean frequency of positive remarks was 3.9 (SD=3.2).
Expressed Emotion and Clinical Outcome
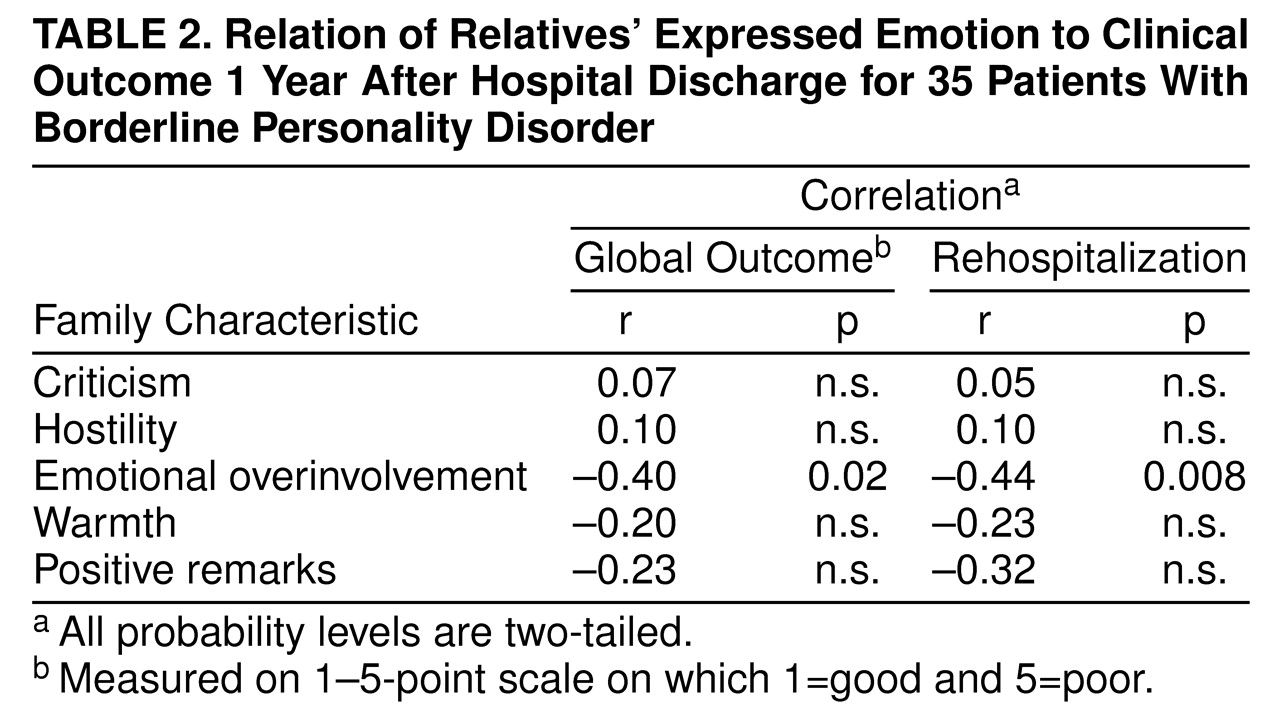
Correlations between the five measured expressed emotion variables (criticism, hostility, emotional overinvolvement, warmth, and positive remarks) and patients’ clinical outcomes are provided in
Table 2. Contrary to what has been found for several axis I disorders, criticism was not significantly predictive of 1-year clinical outcome in the patients with borderline personality disorder. This was true regardless of whether clinical outcome was assessed by using the 5-point outcome scale or indexed according to rehospitalization status. Stated another way, the number of critical comments made by the most critical relative of the rehospitalized patients was not significantly different from the number of critical comments made by the most critical family member of patients who were not rehospitalized (13.6 versus 12.5) (t=–0.30, df=33, n.s.). A subsequent analysis selecting only those patients who lived at home continuously during the follow-up period also failed to reveal any association between criticism and patients’ clinical outcomes (r=0.13, N=14, for rehospitalization and r=0.15, N=14, for global outcome).
Relatives’ scores on the emotional overinvolvement scale of the Camberwell Family Interview, on the other hand, did predict how well patients fared after they were discharged from the hospital. Contrary to what has been found for schizophrenia, however, family emotional overinvolvement was associated with better rather than worse clinical outcomes. The more emotionally overinvolved the patients’ relatives were, the more likely patients were to do well during the follow-up period and the less likely they were to be rehospitalized.
It is important that these results also held when the severity of the borderline symptoms that the patient had at the time of the index hospitalization was considered. Entering both variables simultaneously into a logistic regression analysis to predict rehospitalization resulted in an improvement in statistical significance (χ2=14.51, df=2, p=0.0007). However, only emotional overinvolvement made an independent contribution that was significant (Wald statistic=6.04, p=0.02).
These results highlight the importance of emotional overinvolvement in the prediction of clinical outcome in the patients in this study group. However, in expressed emotion research, emotional overinvolvement is typically used as a dichotomous variable with scores above 3 indicating sufficient emotional overinvolvement for a rating of high expressed emotion to be made on the basis of this variable alone. When we reclassified relatives in this manner, high emotional overinvolvement was still associated with patients receiving better (i.e., lower) ratings on the global outcome scale (mean=2.9 versus mean=4.1) (t=2.43, df=33, p<0.05). Patients with relatives who were rated high on emotional overinvolvement were also significantly less likely to be rehospitalized (χ2=10.80, df=1, p=0.001).
DISCUSSION
To our knowledge, this is the first study to examine the association between expressed emotion and clinical outcome in patients with borderline personality disorder. The results suggest that the predictive validity of expressed emotion may not be the same for borderline personality disorder as it is for axis I conditions such as schizophrenia and mood disorders. Criticism and hostility did not predict poor clinical outcome in borderline patients during the course of a 1-year follow-up. Patients’ clinical outcomes were associated with relatives’ emotional overinvolvement, however. These findings also held when the severity of patients’ initial symptoms was statistically controlled. Higher levels of emotional overinvolvement were associated with better outcomes and absence of rehospitalization. These findings are particularly noteworthy in the light of the association between emotional overinvolvement and clinical outcome that has been found for schizophrenia, where emotional overinvolvement is more typically associated with worse clinical outcome
(30). The converse appears to be true in borderline personality disorder.
The lack of association between criticism and poor outcome in these borderline patients is all the more surprising when we consider how strongly criticism predicts outcome in patients with mood disorders. Mood disorders are highly comorbid with borderline personality disorder
(31), and borderline personality disorder is thought by some to be a form of mood disorder
(32). In fact, all of the patients for whom formal SCID data were available had a current or past diagnosis of an axis I mood disorder. Despite this, criticism did not predict clinical outcome in these patients with borderline personality disorder. This is an issue that obviously warrants further investigation.
Perhaps the most interesting aspect of this study is the link between family level of emotional overinvolvement and better clinical outcome in the borderline patients. In expressed emotion research, emotional overinvolvement is considered to reflect an extreme, dramatic, or overprotective response to the patient’s illness on the part of the family member. Although high levels of emotional overinvolvement in the family are thought to be overstimulating for patients with schizophrenia, the current data raise obvious questions about the meaning of emotional overinvolvement for patients with borderline personality disorder.
One possibility is that emotional overinvolvement may be a signal to borderline patients that the family cares and is engaged with them. Relatives who show high levels of emotional overinvolvement are typically worried and extremely concerned. They often show great attention to the patient’s needs and are extremely self-sacrificing in their behavior toward the patient. In short, they do not minimize or ignore the suffering of the patient. They react, they respond, and, in many cases, they suffer along with the patient. This raises the question of whether, for patients with borderline personality disorder, emotional overinvolvement may actually be a form of validation. Linehan
(14) has suggested that an invalidating environment is very detrimental to patients with borderline personality disorder. Perhaps in the emotional overinvolvement construct we have a family characteristic that is in direct opposition to this—that borderline patients experience emotional overinvolvement as positive. Moreover, for patients with abandonment concerns, the presence of a relative who shows marked emotional overinvolvement may provide a great deal of reassurance that there is someone in their life who will remain with them for the long-term. These are issues that we are now exploring in our current work.
This study is limited by the fact that follow-up data were collected by interviews conducted over the telephone. Face-to-face assessments would clearly have been preferable, although previous research suggests that telephone interviews can be used to assess symptoms in a reliable manner
(33). It is also possible that the association between higher emotional overinvolvement and lower rates of rehospitalization could be explained by a reluctance on the part of an emotionally overinvolved relative to allow the patient to reenter the hospital. However, the mean age of the patients was almost 30 years, and the majority of them were not living with the relatives who were rated high in emotional overinvolvement. The likelihood that relatives could actually prevent a rehospitalization thus appears somewhat limited. The correlation between higher emotional overinvolvement and better clinical outcome on the 5-point global outcome scale also suggests that the role of relatives in preventing rehospitalization is not likely to provide an adequate explanation for the findings.
Finally, it is important to keep in mind that the findings we have reported here, although statistically reliable, may simply reflect variance specific to this study group. An independent replication of this study is clearly necessary before any firm conclusions can be drawn. Replication of these findings would suggest that the link between expressed emotion and clinical outcome may be quite different in patients with borderline personality disorder than it is for patients with schizophrenia, mood disorders, or a variety of other axis I conditions. Although well developed in the case of schizophrenia
(34–
36), family-based treatments for patients with borderline personality disorder are still very much in their infancy. Before we rush to co-opt treatment approaches that have worked for other diagnostic groups, greater understanding of the characteristics of families that might facilitate improvement or maintain pathology in borderline patients is clearly necessary.