Studies in the past decade have noted the frequent co-occurrence of eating disorders and obsessive-compulsive disorder (OCD)
(1–
13). Most studies have focused on patients with anorexia nervosa and have found that between 9% and 69% of subjects with anorexia nervosa have a coexisting diagnosis of OCD. Fewer studies have focused on bulimia nervosa, but these studies show that 8% to 33% of subjects with bulimia also have OCD. In addition, high rates of bulimia (5%
[14] to 15%
[15]) have been reported in samples of people with OCD.
Determining whether such symptoms are a consequence or a potential cause of pathological eating behavior or malnutrition is a major methodological issue in this field. It is impractical to study eating disorders prospectively due to the young age at onset and difficulty in premorbid identification of people who will develop eating disorders. One means of teasing apart cause and effect is to compare subjects who are ill with bulimia and those who are have long-term recovery from bulimia. The assumed absence of confounding nutritional influences in women who have recovered from bulimia raises a possibility that persistent psychobiological abnormalities might be trait-related and potentially contribute to the pathogenesis of this disorder.
In this study, we assessed symptoms of OCD in female patients who were ill with bulimia, female patients who had recovered from bulimia, and women with no psychiatric diagnoses, using a cross-sectional design and a standardized interview measure of OCD symptoms. We studied patients with bulimia who had never had a diagnosis of anorexia nervosa to avoid any potentially confounding effects of the anorexia diagnosis. In addition, we examined the relation of OCD symptoms to depression, anxiety, and cognitive and behavioral dimensions associated with eating disorders.
METHOD
Subjects included 31 women who had symptoms of bulimia nervosa, 29 women who had recovered from bulimia nervosa, and 19 healthy women (comparison subjects). Two experienced psychiatrists (W.H.K. and T.E.W.) made the bulimia nervosa diagnoses using DSM-III-R criteria. Subjects were free of psychotropic medications at the time of assessment, although some were taking birth control pills. Axis I diagnoses were assessed in patients who had recovered from bulimia and in comparison subjects by using a modified Schedule for Affective Disorders and Schizophrenia—Lifetime Version according to methods described elsewhere
(18).
Women who were ill with bulimia were receiving inpatient or outpatient eating disorder treatment at Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center. Subjects were studied within 2 weeks of entrance into treatment.
Subjects who had recovered from bulimia had previously received eating disorder treatment at Western Psychiatric Institute and Clinic or were recruited through advertisements. All of these recovered bulimia patients had maintained their body weight above 85% of normal body weight
(19) since developing the eating disorder; thus, no subjects had a history of anorexia nervosa. For at least 1 year before the study, subjects who had recovered from bulimia 1) had maintained a stable, normal weight, 2) had experienced regular menstrual cycles, and 3) had not binge eaten, purged, or engaged in restrictive eating patterns.
Comparison subjects had no history of any psychiatric disorder (including eating disorder) or medical or neurological illness and no first-degree relatives with an eating disorder. Their body weight had remained in a normal range since menarche, and they experienced normal menstrual cycles. These subjects were recruited through local advertisements. After complete description of the study was provided, written informed consent was obtained from all subjects.
Subjects were evaluated for the presence of OCD-like symptoms by using the Yale-Brown Obsessive Compulsive Scale
(20,
21), a semistructured interview designed to rate the severity and type of symptoms in patients with OCD. Yale-Brown scale assessments were performed on admission to the Western Psychiatric Institute and Clinic treatment programs or at the time of recruitment into the study by one of two psychiatrists (W.H.K. or T.E.W.). Items related to obsessions or compulsions about ritualized eating behaviors or body image were omitted from the scoring. Other measures obtained included the Hamilton Depression Rating Scale
(22), Hamilton Anxiety Rating Scale
(23), and Eating Disorder Inventory
(24).
Variables such as age, body weight, and Yale-Brown scale scores were compared by using analysis of variance with two-tailed, Bonferroni-corrected, post hoc t tests. The strength of associations between variables was examined by using Spearman correlations. The significance of differences between correlation coefficients was investigated with z tests. Pearson’s chi-square analyses were used to compare frequencies of the two patient groups’ target symptoms.
RESULTS
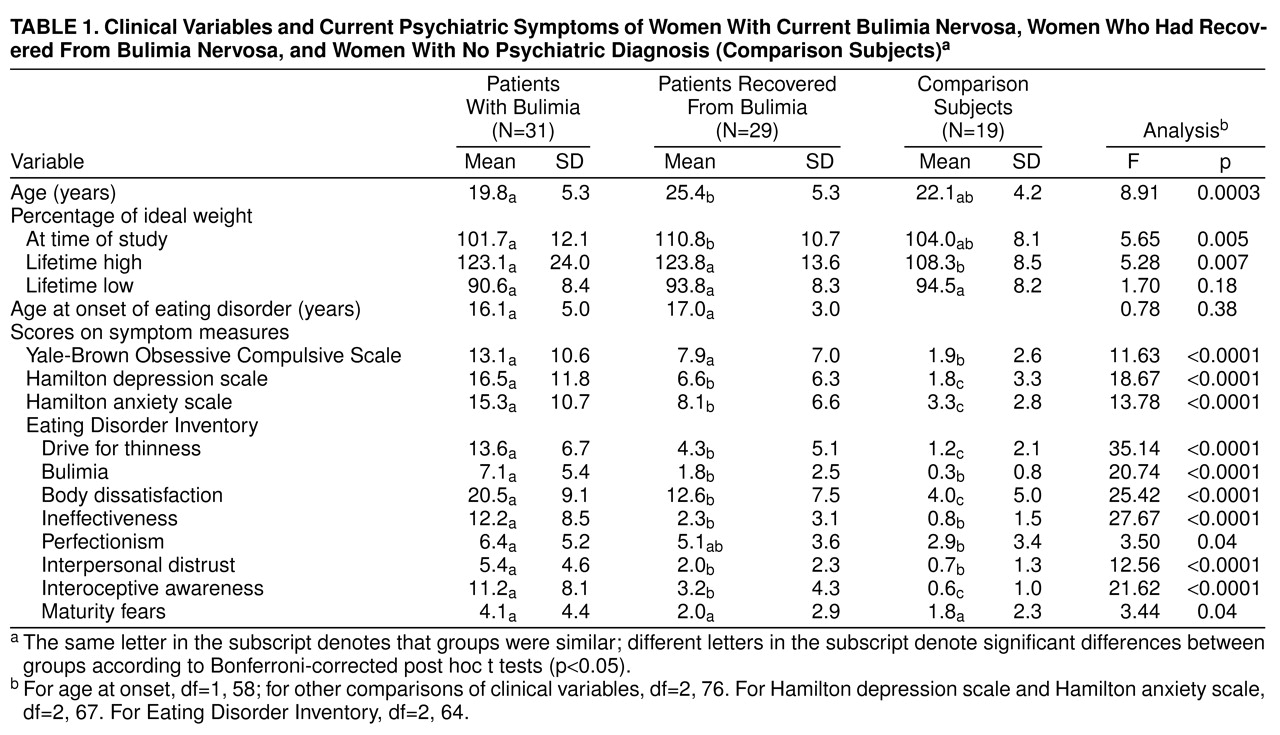
The mean age of all subject groups was late teens to mid 20s, but the subjects who had recovered from bulimia were significantly older than those who were ill with bulimia (
table 1). The age of comparison subjects was similar to both those who were ill with bulimia and those who had recovered from bulimia. At the time of this study, all three groups of subjects were within a normal weight range. However, subjects who were ill with bulimia weighed less than subjects who had recovered from bulimia, and comparison subjects were intermediate between the two patient groups. Subjects’ lifetime low body weights were similar, but the two bulimia groups had significantly higher lifetime peak body weights than comparison subjects. Age at onset of bulimia did not differ significantly between the two patient groups. Women who had recovered from bulimia had been recovered for a mean of 36 months (SD=24) at the time of this study.
Patients who were ill with bulimia nervosa and those who had recovered from bulimia had similar Yale-Brown scale total score; however, these scores were significantly higher in both groups of bulimia patients than in the group of comparison subjects (
table 1). There was a trend toward significance in the comparison of Yale-Brown scale scores of seven subjects who had recovered from bulimia and had a diagnosis of OCD in their lifetime (mean=11.4, SD=8.3) and 21 subjects who had recovered from bulimia and had no lifetime diagnosis of OCD (mean=6.2, SD=6.0) (t=–1.83, df=26, p=0.08).
Subjects who were ill with bulimia had higher scores on measures of depression and anxiety and on seven of the eight Eating Disorder Inventory subscales than the other two groups. Subjects who had recovered from bulimia had significantly higher scores than comparison subjects on depression and anxiety measures and on three of the eight Eating Disorder Inventory subscales (drive for thinness, body dissatisfaction, and interoceptive awareness).
Yale-Brown scale total symptom scores for patients who were ill with bulimia and those who had recovered from bulimia were not significantly related to demographic variables (rs=–0.12–0.16, all n.s.). For women who had recovered from bulimia, duration of recovery was not related to Yale-Brown scale scores or the number of target symptoms (rs=0.01 and rs=0.05, respectively). For both bulimia groups, Yale-Brown scale scores were positively related to depression (for patients who were ill with bulimia, rs=0.62, p<0.01; for patients who had recovered from bulimia, rs=0.36, p<0.05) and anxiety (for patients who were ill with bulimia, rs=0.62, p<0.01; for patients who had recovered from bulimia, rs=0.54, p<0.05). In addition, positive relationships were evident between Yale-Brown scale scores and Eating Disorder Inventory body dissatisfaction scores for the patients who were ill with bulimia (rs=0.47, p<0.05) and Eating Disorder Inventory ineffectiveness scores for both bulimia groups (for patients who were ill with bulimia nervosa, rs=0.33, p<0.05; for patients who had recovered from bulimia nervosa, rs=0.41, p<0.05).
There was a significant difference between bulimia groups on only one scale: Yale-Brown scale scores of the patients who had recovered from bulimia nervosa were positively correlated with the bulimia scale (rs=0.35), but the scores of the patients who were ill with bulimia nervosa scores were negatively correlated with the bulimia scale (rs=–0.32, p<0.05).
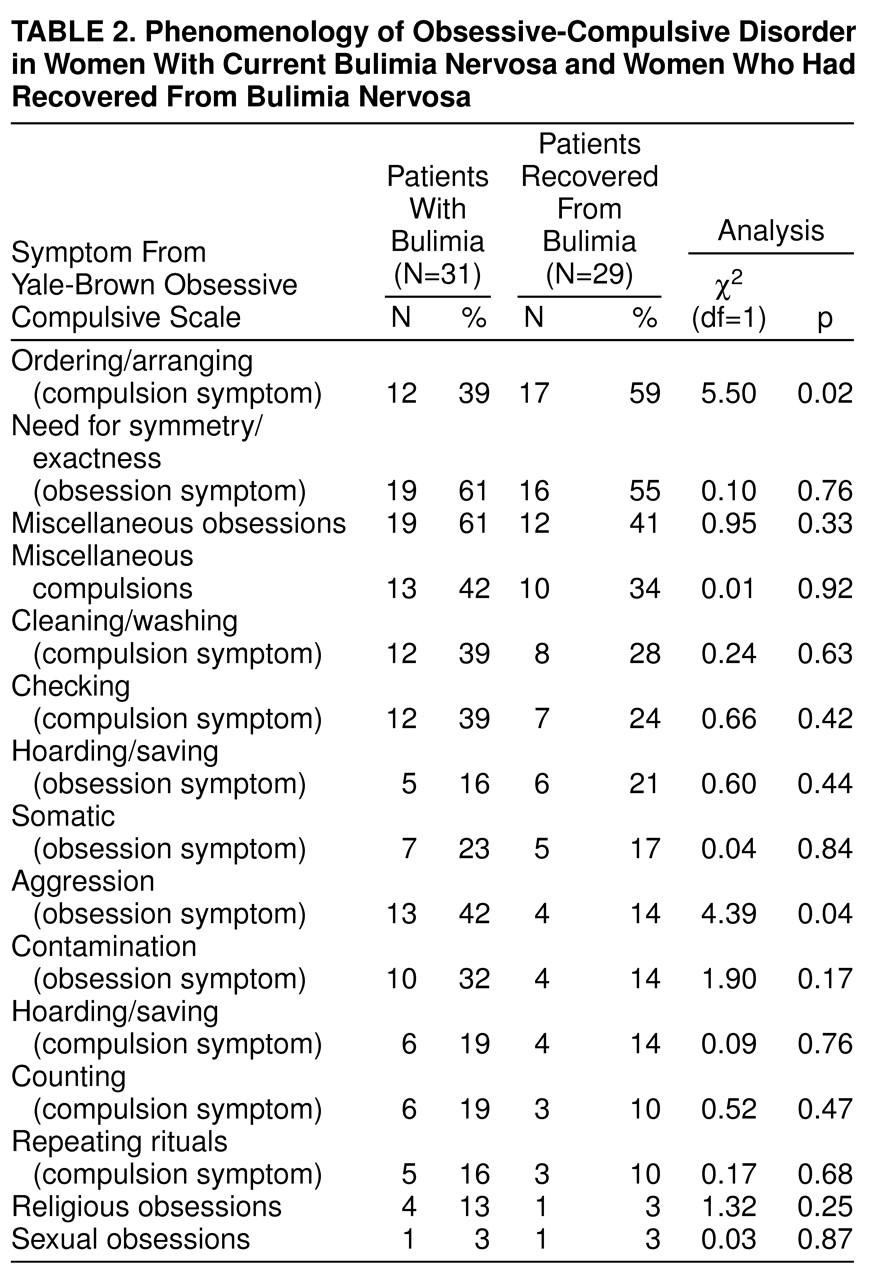
The Yale-Brown scale includes 15 clusters of target symptoms (
table 2). Overall, the two groups’ patterns of symptoms were quite similar. That is, when the number of counts for each cluster was compared for the patients who were ill with bulimia and those who had recovered from bulimia, the number of target symptoms within each cluster was highly correlated (r
s=0.80, p<0.001). The most common target symptoms in patients who had recovered from bulimia involved ordering/arranging and symmetry/exactness. Less frequent were cleaning/washing and checking symptoms, whereas other obsessive-compulsive symptoms were relatively uncommon.
Of the five most common symptoms experienced by each patient group, only two occurred significantly more often in one group than the other: 1) the women who were ill with bulimia reported aggressive obsessions more frequently than did those who had recovered from bulimia; 2) ordering/arranging compulsions were more common among those who had recovered from bulimia nervosa than those who were ill with bulimia (
table 2). However, as noted above, ordering/arranging compulsions were still among the most common OCD symptoms in subjects who were ill with bulimia.
Miscellaneous obsessions and compulsions were relatively common in both bulimia nervosa groups (
table 2). There was some overlap between groups in individual symptoms endorsed, but no overall pattern of miscellaneous symptoms emerged. The miscellaneous obsession symptoms most commonly endorsed by subjects who had recovered from bulimia were being bothered by certain sounds/noises (endorsed by seven [30%]), intrusive nonsense sounds, words, or music (N=6 [26%]), and fear of losing things (N=5 [22%]); those most frequently endorsed by subjects who were ill with bulimia were fear of not saying just the right thing (N=10 [35%]) and being bothered by certain sounds/noises (N=7 [24%]). Miscellaneous compulsion symptoms most frequently endorsed by subjects who had recovered from bulimia included excessive list-making (N=5 [22%]), superstitious behaviors (N=3 [13%]), and other (N=3 [13%]); those endorsed most often by subjects who were ill with bulimia were excessive list-making (N=5 [17%]), need to tell, ask, or confess (N=5 [17%]), and other (N=4 [14%]).
Each bulimia group was subdivided into subjects who endorsed any Yale-Brown scale symmetry obsessions and ordering compulsions and those who endorsed neither. The subgroups had similar values for the measures described in
table 1. However, it should be noted that as a result of dividing the groups, there were small numbers of subjects in some cells.
DISCUSSION
Yale-Brown scale scores of women who were ill with bulimia and those who had recovered from bulimia were similar and showed mild to moderate obsessionality. For both bulimia groups, Yale-Brown scale scores were significantly higher than those of healthy women. Other studies
(4–
6,
10,
12–
15) have found elevated levels of obsessionality in clinical and nonclinical samples of women with symptomatic bulimia; however, to our knowledge, this is the first report of measures of obsessionality after recovery from bulimia.
The Yale-Brown scale scores of subjects who were ill with bulimia were substantially lower than those reported for people with anorexia nervosa or OCD
(25,
26). Mean Yale-Brown scale scores in both anorexia nervosa and OCD samples have been reported to be in the low 20s, but the patients who were ill with bulimia in our study had a mean score of 13 (SD=11). However, the scores of the patients who had recovered from bulimia nervosa were similar in magnitude to the scores of subjects who had recovered from anorexia nervosa
(27), suggesting that individuals recovered from an eating disorder experience similar levels of functional impairment from OCD symptoms.
This study found that subjects who were ill with bulimia and those who had recovered from bulimia tended to endorse similar types of OCD-like target symptoms. These symptoms tended to include an obsessive need for symmetry and exactness and a compulsion to order and arrange. Other studies have found similar results in people with anorexia nervosa and bulimia. Thiel et al.
(12) found an obsessive need for symmetry and compulsion for order to be common symptoms in patients with eating disorders and OCD in Germany. Symmetry and order were the most frequently identified symptoms in Japanese patients with bulimia and OCD
(28). Previous research with anorexia nervosa subjects
(27) has found that symptoms of symmetry, exactness, ordering, and arranging were the most commonly reported symptoms in ill and recovered subjects. Together, these data suggest that commonalties exist in the kinds of OCD symptoms experienced by women with eating disorders, regardless of type of eating disorder and whether subjects were ill or recovered, and independent of culture.
Leckman et al.
(29) found that four symptom dimensions occurred in OCD. One dimension was symmetry and ordering, which occurred most commonly in men. Symmetry, ordering, and perfectionism are the most common target symptoms in women with anorexia nervosa and bulimia, and these traits persist after recovery. These data raise the provocative question of whether these two disorders reflect sex-specific expressions (OCD in men, eating disorders in women) of a shared psychobiology related to symmetry obsessions and ordering compulsions.
A formal diagnosis of OCD was not made in the women who were ill with bulimia. However, using a structured diagnostic instrument, we found a 25% lifetime rate of a DSM-III-R diagnosis of OCD in the women who had recovered from bulimia. It is important to note that we found mildly elevated Yale-Brown scale scores even in those women who had recovered from bulimia and had no diagnosis of OCD. Thus, the higher rate of obsessionality among the women who had recovered from bulimia relative to comparison subjects was not caused by extremely high Yale-Brown scale scores among the minority with a lifetime history of OCD. These results are consistent with results of a study by Thiel et al.
(30), who found that Hamburg Obsession-Compulsion Inventory scores did not differ significantly in individuals with and without comorbid OCD 30 months after the end of treatment for anorexia nervosa or bulimia.
Relative to the other groups, the women who were ill with bulimia nervosa had elevated levels of depression, anxiety, and symptoms related to eating disorders. In general, these symptoms were present to a milder degree after long-term recovery. Although they were significantly improved compared with the symptoms of women who were ill with bulimia, the levels of symptoms of depression and anxiety and certain attitudes related to eating disorders in the women who had recovered from bulimia were higher than those of the healthy subjects. However, on other measures of attitudes and behavior related to eating disorders, including self-reported bulimic symptoms, the responses of women who had recovered from bulimia resembled those of comparison subjects. These findings suggest that although subjects who had recovered from bulimia may have recovered behaviorally from bulimia and recovered partially on certain cognitive dimensions, some cognitive symptoms still persisted at a moderate level.
For both groups of bulimia subjects, significant correlations were found between the level of subjects’ OCD symptoms and depression, anxiety, and feelings of ineffectiveness. However, correlations with measures of depression and anxiety were stronger for the patients who were ill with bulimia nervosa than for the patients who had recovered from bulimia, suggesting that these relationships may diminish with recovery or cessation of binge eating and purging. It is possible that negative affect may inflate obsessional symptoms. Alternatively, obsessionality and negative affect may both be elevated secondary to malnutrition
(31).
The fact that OCD symptoms persist after recovery from an eating disorder, and after symptoms of depression and anxiety have improved, supports the possibility that obsessionality may be a trait-like attribute in bulimia. It is of interest that subjects who had recovered from bulimia nervosa have a persistent disturbance of brain serotonin activity after recovery, since it has been hypothesized that serotonin dysregulation may mediate a relationship between obsessionality and eating disorders
(18,
32).
Limitations of this study include its cross-sectional design and modest number of study subjects. A longitudinal study of symptoms of obsessionality in women with eating disorders through their recovery is needed to confirm the present findings. In addition, studies of women after longer recovery from bulimia might help clarify whether such symptoms are underlying personality characteristics or these symptoms resolve over a longer period of time.
The development of an eating disorder is often attributed to the effects of our cultural environment, such as mass media, on body image. However, all women in our society are exposed to cultural mores that value slimness, but only a small percentage of women exposed to these messages develop an eating disorder. Thus, it is possible that there may be underlying vulnerabilities that place someone at risk for developing bulimia. The persistence of obsessional traits related to exactness, negative affect, and core eating disorder symptoms after recovery raises the question of whether these are such “risk” traits. Prospective studies of girls with such behavioral traits are needed to determine whether they are at risk to develop bulimia.