Although many people are exposed to trauma, only some individuals develop posttraumatic stress disorder (PTSD); most do not
(1–
4). Further, in a large proportion of individuals who do develop the disorder, the disorder fully remits over time. These findings suggest that chronic PTSD may represent a specific type of adaptation to trauma that is not typical of most individuals, but rather is seen in individuals who have a particular kind of vulnerability to stress. Researchers have identified several specific psychosocial risk factors for PTSD, including a history of exposure to traumatic events, exposure to multiple traumatic events, exposure to childhood sexual or physical trauma, and the subjective experience of fear for one’s life
(5–
7). However, because these factors still leave a great deal of the variance unexplained, investigations evaluating risk factors for the development of PTSD continue.
Over the past decade, numerous investigators have begun to reexamine the relationship between trauma, symptoms of dissociation, and the development of PTSD
(8–
17). Taken together, the data from several studies suggest that peritraumatic symptoms of dissociation (i.e., symptoms of dissociation experienced during and for a short time immediately after exposure to a traumatic event) represent a significant risk factor for the subsequent development of PTSD. Symptoms of dissociation also appear to be significantly related to somatic complaints reported by victims of trauma
(18) and may play a significant role in the reported relationship between PTSD and physical health
(19).
Although intriguing, these findings cannot be interpreted with a high degree of certainty because they were based on retrospective accounts. Consequently, it remains unclear whether: 1) dissociation serves as a risk factor for subsequent development of PTSD, 2) trauma independently causes dissociation and PTSD, or 3) individuals with current dissociative symptoms are biased toward overreporting the presence and severity of dissociative symptoms at the time of a past trauma.
Although peritraumatic dissociation appears to be a risk factor for stress-related illness, surprisingly little is known about its nature and frequency in individuals (such as military personnel) who are at high risk for exposure to trauma and PTSD. At present, it is not known whether the propensity to dissociate is the result of trauma exposure or whether it represents a trait that not only predisposes an individual to dissociate during stress but also renders that person more vulnerable to the development of PTSD. Examining individuals’ propensity to dissociate before, and in response to, stress exposure—before the development of PTSD—would provide data about whether dissociation is a relatively common response to realistic threats and whether there is a relationship between history of trauma exposure and propensity to dissociate when confronted with high stress. This type of information would help clarify the nature of the relationship between dissociation and PTSD.
This study was part of a larger investigation examining the neuroendocrine profiles of healthy soldiers participating in survival training conducted by the U.S. Army
(20,
21). The design permitted an assessment of the presence and severity of state dissociative symptoms in healthy military subjects before and after exposure to highly intense stress. The design also permitted an assessment of whether factors such as the amount (or type) of previous trauma, as well as the nature of response to previously experienced trauma, would significantly contribute to symptoms of dissociation before and during acute stress.
The U.S. Army’s survival training course is among the most difficult and rigorous training programs in the U.S. Armed Forces. Several factors make the survival course an ideal environment in which to study the relationship between highly intense stress and symptoms of dissociation. First, the course participants represent a healthy, nonclinical group of subjects who are at high risk for exposure to military-related trauma and, consequently, at risk for the development of combat-related stress disorders such as PTSD. Second, the course allows for a highly controlled and uniform application of stress across subjects. Third, the training scenario represents the best analog of realistic military stress, as it is multidimensional (combining psychological, physical, and environmental stress) and results in neurobiological alterations that are on a par with those that occur in actual threat-to-life experiences (see the last paragraph in this section)
(20,
21).
The survival course is 19 days long and includes a low-stress didactic (classroom) phase and a highly stressful experiential phase. During the experiential phase, students are confronted with a variety of stressors, including semistarvation, sleep deprivation, lack of control over personal hygiene, and external control over movement, social contact, and communication. The experiential phase provides students with the opportunity to apply their training in a controlled, albeit stress-laden, environment.
Previous investigations have provided robust evidence that the stress of the experiential phase of the survival school training produces significant alterations in neuroendocrine responses, including changes in glucocorticoids, catecholamines, gonadal steroids, and neuropeptide Y
(20,
21). The magnitude of these responses is analogous to that produced in real-world life-threatening situations and is also similar to that found in previous studies of high-stress military training (nocturnal landings on an aircraft carrier, military free-fall, and Ranger training). As such, survival school training provides an ethologically realistic setting for studying neurobiological aspects of acute stress in humans and is well suited for a prospective examination of the relationship between acute stress and psychological symptoms of dissociation.
Method
Subjects and Procedure
Two studies with separate groups of subjects were conducted. The subjects of study 1 were 50 Special Forces and 44 general infantry soldiers (mean age=31.6 years, SD=4.8, and mean age=28.9 years, SD=5.1, respectively). The subjects of study 2 were a separate group of 18 Special Forces and 41 general infantry soldiers (mean age=27.1 years, SD=4.4, and mean age=22.0, SD=3.6, respectively). Special Forces soldiers—also known as Green Berets—are individuals who have successfully completed the Special Forces Selection and Assessment course, followed by the Special Forces Qualification Course. These training hurdles involve high levels of challenge to physical endurance, academic abilities, and stress tolerance. Only 25% of applicants are ultimately successful in the Special Forces Selection and Assessment course. Thus, Special Forces soldiers represent a highly selected population of military subjects.
Per course requirements, all subjects received medical and psychological clearance before in-processing to survival school at Fort Bragg, N.C. All were free of illicit substances. After completing in-processing to the survival school, subjects were given a description of the nature and purpose of the study by the principal investigator (C.A.M.). Each gave written, informed consent to participate in the study. Each understood that refusal to participate in the study would not adversely affect their standing in the survival course. Sixteen subjects declined to participate in the study. Eleven of the 16 stated that they did not enroll in the study because they were not confident that research information would remain separate from their military records. They worried that such information, if inadvertently included in their military records, might jeopardize their subsequent evaluations. The remaining five did not offer an explanation for refusing to participate in the study.
Subjects in study 1 were administered the Clinician-Administered Dissociative States Scale after completing the experiential phase of the survival training. The Clinician-Administered Dissociative States Scale is a reliable, valid, self-report instrument designed to assess state symptoms of dissociation in response to a specified stressor
(22). The scale includes 19 self-report items and eight observer-rated (clinician-rated) items. Subjects rated the intensity of the dissociative experiences on a scale from 0, not present, to 4, extreme. The scores for individual items were summed to produce the total score. Subjects were instructed to respond to the scale items by using the experiential period of the survival training as the reference point. Due to the design and nature of the survival training, it was not possible to accurately determine ratings for the eight observer-rated items. Thus, only the subjective items were rated. This modification is compatible with other self-report inventories and does not alter the validity or reliability of the Clinician-Administered Dissociative States Scale
(22; J.D. Bremner, personal communication, 1999).
Subjects in study 2, a separate cohort from those in study 1, completed the Clinician-Administered Dissociative States Scale and the Brief Trauma Questionnaire during the week of classroom activities before exposure to acute stress. These subjects completed the dissociation scale again at the conclusion of the experiential phase of the training. When filling out the dissociation scale at baseline, subjects were instructed to use the two previous days of classroom activities as their reference point. When filling out the poststress assessment, subjects were given instructions to complete the scale in response to the two previous days of the experiential phase.
Subjects in study 2 also completed the Brief Trauma Questionnaire in the didactic phase of the course, prior to stress exposure. The Brief Trauma Questionnaire is a valid, reliable, self-report instrument designed to assess the number and types of traumatic events to which an individual has been exposed in life
(23). The scale also permits an assessment of whether an individual suffered “physical injury” or experienced “fear for one’s life” in relation to a previous trauma. Endorsement of either of these items is interpreted as exposure to a traumatic event, as outlined in criterion A of the DSM-IV criteria for posttraumatic stress disorder.
Finally, just after completing the experiential phase of the survival course, a randomly selected group of subjects in study 2 (N=36) were administered the Health Problem List. The Health Problem List is a valid and reliable self-report instrument comprising 80 items designed to assess current somatic symptoms (such as heartburn, chest pain, ringing in ears, etc.)
(24). The total score is the number of items endorsed. In this paper this score will be referred to as the somatic symptom score to avoid any misconception that this instrument reflects a medical history inventory.
Data Analysis
In study 1, t tests were used to compare Special Forces and general infantry soldiers on poststress Clinician-Administered Dissociative States Scale scores. In study 2, paired t tests were used to examine change over time in dissociation scale item scores and total score. In addition, independent t tests were used to evaluate whether dissociation scale item scores differed between Special Forces and general infantry soldiers. Pearson and point-biserial correlations were used for univariate comparisons within each time point (prestress and poststress) in order to select variables for multivariate analysis. Simultaneous multiple hierarchical regression analyses were used to examine predictors of Clinician-Administered Dissociative States Scale scores after the stress of the experiential phase. A p value of 0.05 was used for interpreting statistical significance.
Results
Study 1
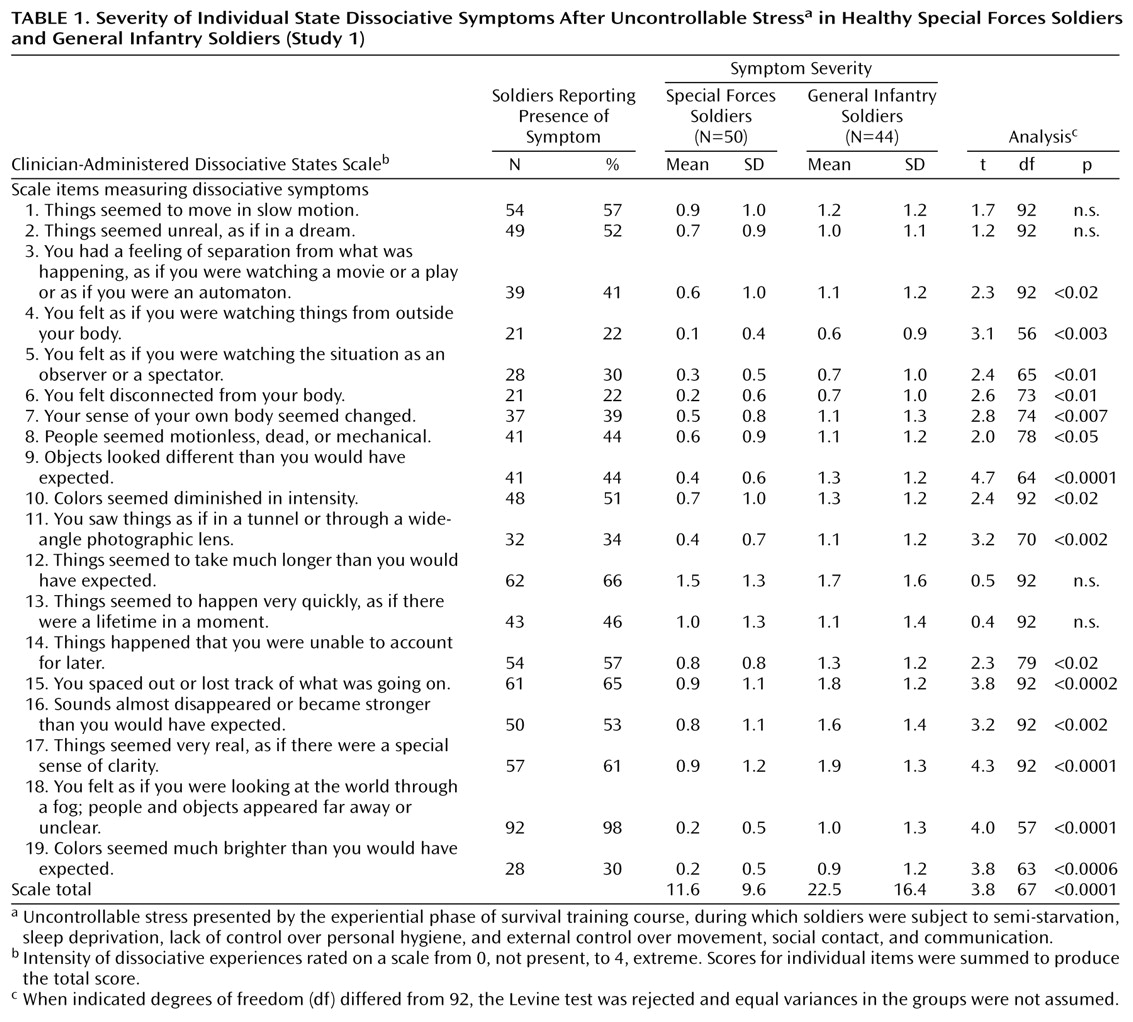
Total mean Clinician-Administered Dissociative States Scale scores after stress were significantly lower in the Special Forces subjects, compared to the general infantry subjects. As shown in
Table 1, comparisons between the two groups for each dissociation scale item revealed significant differences on all but four items (items 1, 2, 12, and 13).
Table 1 also shows that the most common symptoms of dissociation for the overall group of subjects were those in items 18, 12, and 15 (“looking at the world through a fog” [98%], the experience taking longer than expected [66%], and “spacing out” [65%], respectively).
Study 2
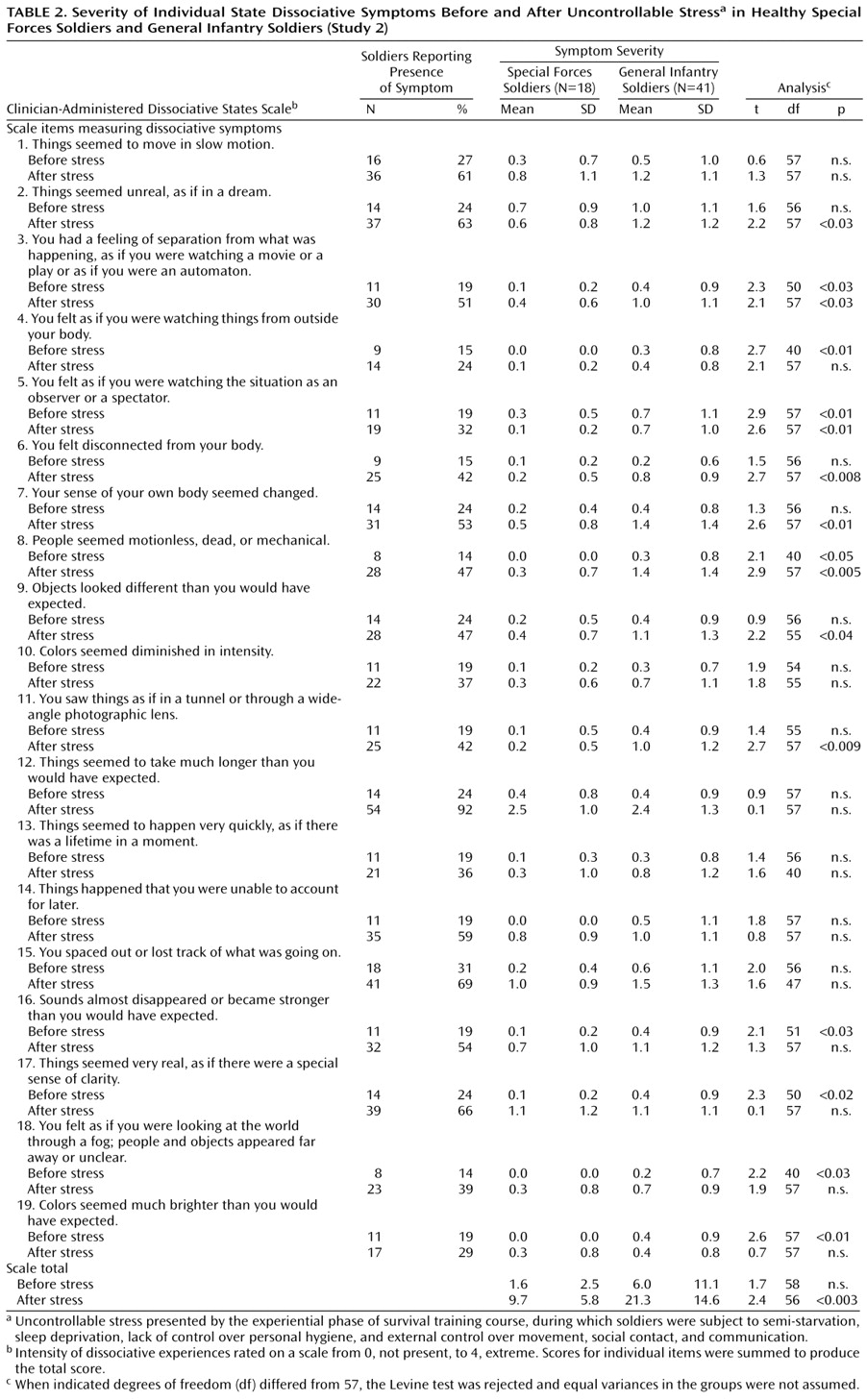
There was a substantial overall increase in reports of dissociative symptoms from before to after the acute stress of the experiential phase, indicating that the experiential phase of the survival course was highly stressful (
Table 2). Pre- and poststress scores were significantly correlated (r=0.45, df=57, p<0.001). Paired t tests (not shown in
Table 2) indicated that significant within-subject differences existed between the prestress and the poststress total scores on the Clinician-Administered Dissociative States Scale (t=6.8, df=56, p<0.0001). Significant within-subject increases in scores were also observed on the individual scale items, with the exception of items 4 and 19 (item 1: t=4.1, df=56, p<0.0001; item 2: t=4.2, df=56, p<0.0001; item 3: t=3, df=56, p<0.003; item 4; t=0.7, df=56, p<0.40; item 5: t=2.3, df=56, p<0.03; item 6: t=3.8, df=56, p<0.0001; item 7: t=4.6, df=56, p<0.0001; item 8: t=5.0, df=56, p<0.0001; item 9: t=3.1, df=56, p<0.003; item 10: t=2.7, df=56, p<0.01; item 11: t=2.8, df=56, p<0.008; item 12: t=12.4, df=56, p<0.00001; item 13: t=2.4, df=56, p<0.02; item 14: t=3.5, df=56, p<0.001; item 15: t=5.0, df=56, p<0.0001; item 16: t=4.2, df=56, p<0.0001; item 17: t=4.7, df=56, p<0.002; item 18: t=3.2, df=56, p<0.002; and item 19: t=0.8, df=56, p<0.40).
Table 2 indicates the most common symptoms of dissociation before and after stress exposure for the group as a whole and also compares the Special Forces and general infantry groups on each of the pre- and poststress dissociation scale items. As in study 1, alterations in perception of time, perception of the environment, and clarity of thought (for example, items 12, 15, and 17) were among the ten most common symptoms reported by subjects.
Table 2 also shows the results of the independent t tests comparing the two groups’ scores on each of the dissociation scale items before and after stress. As in study 1, scores on items 3, 5–9, and 11 differed significantly between the Special Forces and the general infantry soldiers after stress exposure, whereas items 12 and 13 did not. Unlike the findings in study 1, the study 2 findings showed that the two groups did not differ significantly in their poststress scores on items 4 and 14–19. The probability values for these items were at the 0.09 significance level, and the findings may be the result of a lack of power given the smaller number of Special Forces soldiers in study 2.
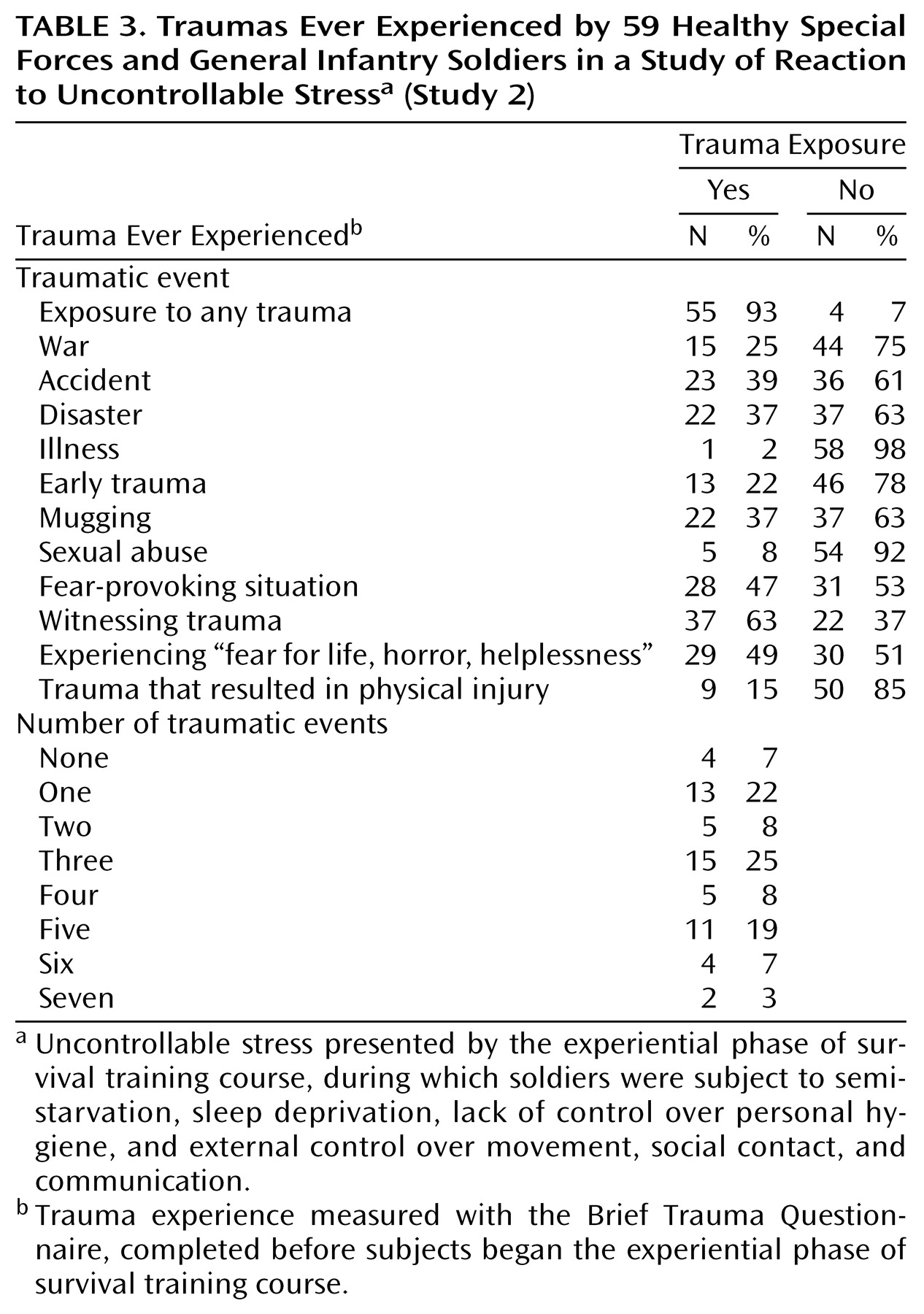
Table 3 shows the frequency of and types of trauma that subjects in study 2 had previously experienced. The subjects provided this information before beginning the experiential phase of the survival course. More than 90% of the subjects reported previous exposure to a potentially traumatic stressor.
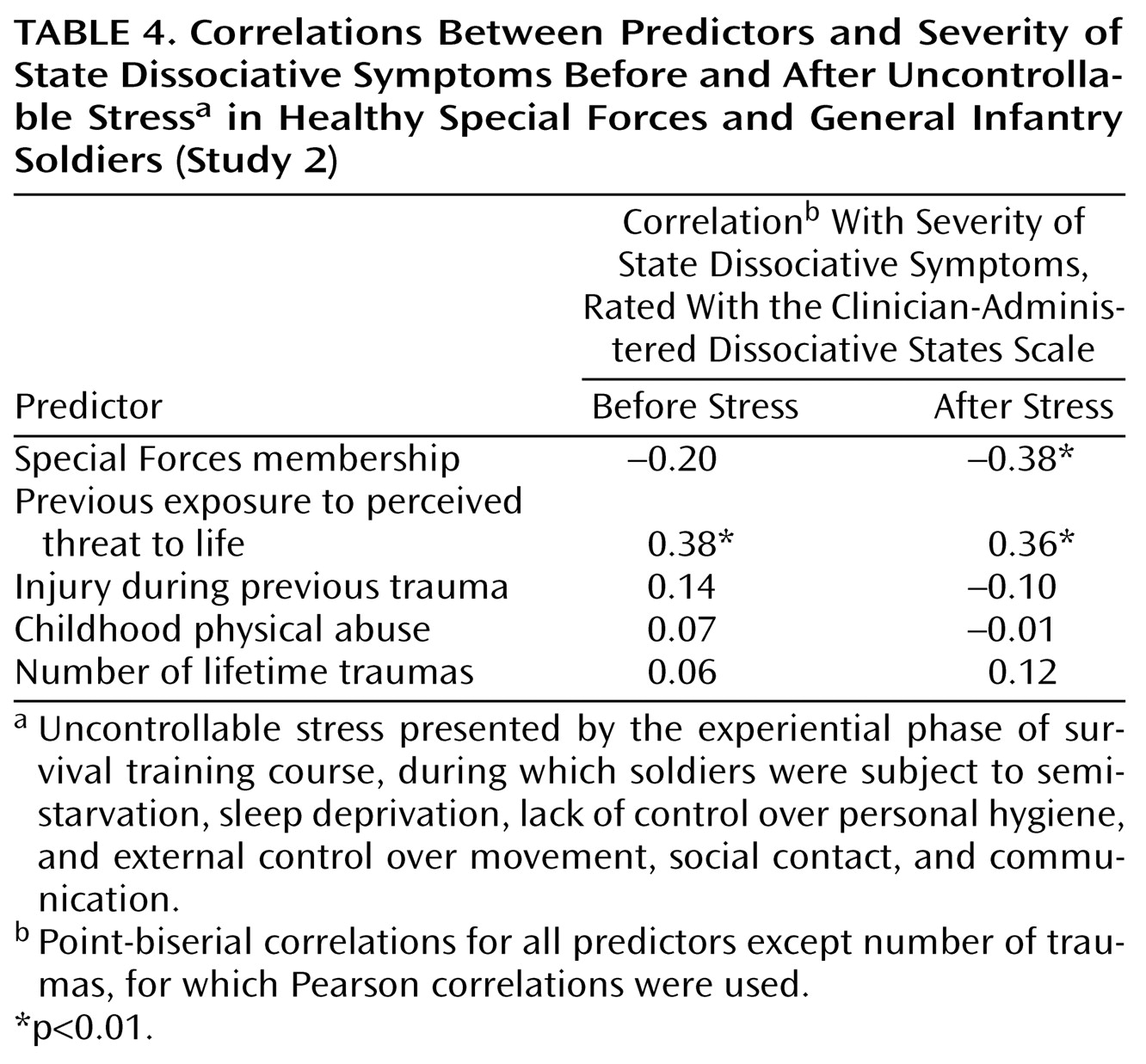
Table 4 presents the results of univariate tests of association for baseline and poststress Clinician-Administered Dissociative States Scale scores with Special Forces membership and trauma exposure. To facilitate comparisons among the predictors, the data are presented as correlations. All results are point-biserial correlations except for those involving number of traumas, which are Pearson correlations. Only two variables were correlated with dissociation scale scores at one or both time points. Special Forces membership was unrelated to the prestress score but was related to the poststress score, replicating the findings of study 1. Perceived life threat during a trauma was related to higher dissociation scale scores both before and after stress.
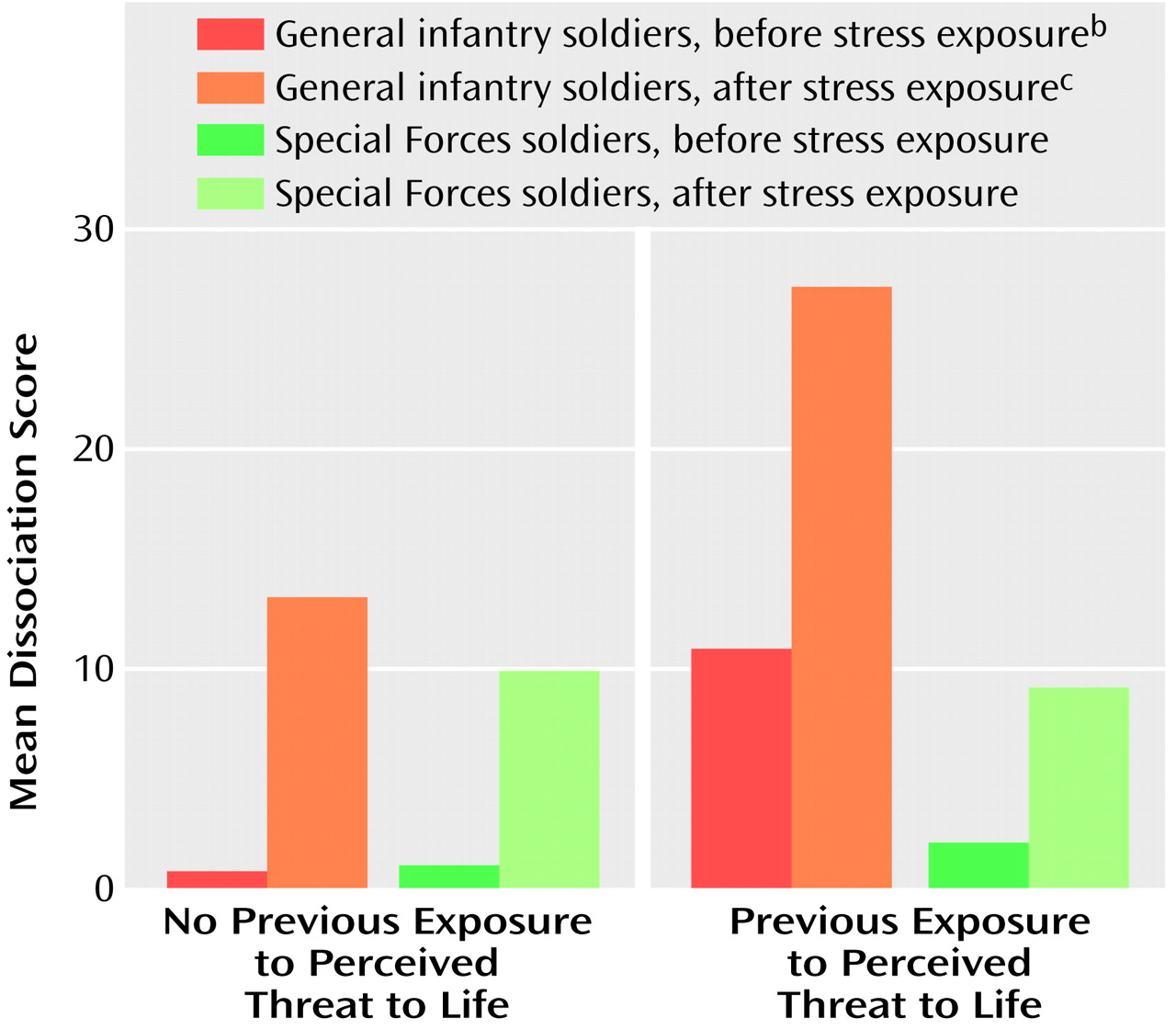
The fact that only two dichotomous variables were related to dissociation scale scores provided an opportunity to examine change in scores after stress exposure in subtypes of individuals who differed in potential vulnerability. Three dummy variables were created to reflect the following natural groups: Special Forces soldiers with previous exposure to a perceived threat to life (N=8), general infantry soldiers with no prior perceived threat to life (N=20), and general infantry soldiers with prior exposure to a perceived threat to life (N=20). The Special Forces subjects with no prior perceived threat to life (N=9) were selected as the reference group because we assumed they would have the least reaction to the stress of the experiential phase of the survival course. The three dummy variables were used in a multiple regression analysis predicting poststress Clinician-Administered Dissociative States Scale scores, while controlling for prestress scores. This approach is analogous to predicting change in dissociation scale scores from before to after stress exposure. Relative to the Special Forces subjects without a prior threat to life, only the general infantry subjects who had experienced a threat to life had a significantly greater score after stress exposure. The unstandardized regression coefficients, which represent the difference in adjusted mean change in scores between each group and the group of Special Forces subjects with no prior threat to life, were as follows: Special Forces soldiers with a prior threat to life (B=–1.48, n.s.), general infantry soldiers with no prior threat to life (B=3.46, n.s.), and general infantry soldiers with a prior threat to life (B=12.97, p<0.005). To facilitate interpretation of the regression analysis, prestress and poststress Clinician-Administered Dissociative States Scale scores are represented in
Figure 1.
Scores on several dissociation scale items, however, were significantly different between groups before acute stress. These items pertained to a sense of separation from one’s body—watching things as if outside one’s body—and to altered perception of other individuals and the environment. Nevertheless, scores on many items (items 3 and 5–11) were once again found to be significantly lower in Special Forces subjects than in general infantry subjects.
No significant correlations were observed between age, number of traumas, the baseline Clinician-Administered Dissociative States Scale score, and the somatic symptoms score. Significant, positive correlations were observed between the somatic symptoms score and the poststress dissociation scale score (r=0.54, df=34, p<0.02) as well as between the somatic symptoms score and the change in the dissociation scale score from the baseline to the poststress assessment (r=0.67, df=34, p<0.01).
Discussion
The current data provide evidence that symptoms of dissociation are extremely common in healthy humans experiencing acute, highly intense stress. Further, such symptoms are significantly associated with the way in which a person has responded to, or has interpreted, a previously experienced traumatic event. The experience of “fearing for one’s life” significantly influenced the degree to which subjects experienced symptoms of dissociation before and during the stress of survival school. Dissociation was least prevalent in Special Forces soldiers—considered “stress hardy” by the U.S. Army—and was most prevalent in general infantry soldiers. Because Special Forces soldiers, as a group, tended to report more early trauma, yet dissociated the least under stress, they may represent individuals who have been “stress inoculated” by previous life events. Finally, symptoms of dissociation accounted for 41% of the variance in the physical health problems reported by subjects after stress exposure. This finding supports the idea that somatic distress and psychological adaptation to stress are linked.
The fact that acute stress-induced symptoms of dissociation were extremely common provides evidence that realistic military stress produces high levels of dissociation in psychologically healthy individuals. Indeed, the highly similar poststress dissociation scale scores in study 1 and study 2 indicate that the majority, and not the minority, of subjects experienced dissociation under stress. These findings suggest that the studies describing a “causal link” between peritraumatic dissociation and PTSD must be viewed with caution. Additional research is needed to clarify whether an etiological link between dissociation and PTSD exists.
General infantry soldiers experienced significantly more dissociative symptoms compared to Special Forces soldiers. This finding is consistent with the observations of other researchers that a large number of cases of combat-related stress reactions and subsequent PTSD arise in military personnel who are not front-line, elite, combat arms soldiers
(25).
In study 2, individuals with the highest levels of dissociation were those who reported intense subjective responses to a previous trauma experience (“feared for their life”). These subjects reported higher levels of dissociation in the relatively mild classroom setting. However, when assessed after the high stress phase of the training, this group split into two subgroups: one that experienced an increase in dissociation and another that experienced low levels of dissociation. The subjects with lower levels of dissociation during stress were Special Forces soldiers. Although they had reported fearing for their life in response to a previous trauma, they exhibited the lowest increase of symptoms of dissociation in response to the actual stress of the experiential phase of survival school. By contrast, general infantry soldiers who reported fearing for their life in a previous trauma exhibited the greatest increase in dissociation in response to survival school stress.
One possible explanation is that exposure to early trauma or exposure to previous military training allowed the Special Forces soldiers to develop enhanced resistance to (or tolerance of) high-intensity stress. This phenomenon would be consistent with the concept of stress toughening
(26). A second possible explanation is that individuals prone to higher levels of stress-induced dissociation may be screened out in the program used to select soldiers for the Special Forces.
Third, an individual’s formulation of his experience after a previous trauma may determine his subsequent responses to stress
(27,
28). Individuals who form an appraisal of their experience that is nonalarming may be more stress tolerant. The relationship between postevent narratives, arousal, and responses to stress remains to be explored
(29).
In both study 1 and study 2, Special Forces and general infantry soldiers differed significantly on poststress scores on Clinician-Administered Dissociative States Scale items that referred to an altered sense of one’s body, the environment, and other people. Previous investigation has shown that Special Forces subjects exhibited significantly higher plasma levels of neuropeptide Y in response to survival school stress
(20). Neuropeptide Y has been shown to exhibit antianxiety and antistress properties, as well as an ability to enhance memory, alertness, and perception during stress
(30,
31). It is possible that the differences in scores on the dissociation scale items are linked to an enhanced capacity for neuropeptide Y release during stress in Special Forces soldiers.
There was a significant and positive correlation between perceived health and dissociation. Dissociation accounted for 41% of the variance in somatic complaints. The presence of empirical, prospective evidence linking physical distress and dissociation is noteworthy and underscores the degree to which psychological adaptation to uncontrollable stress is linked to physical well-being
(21,
32). These data highlight the need for medical professionals to assess concurrent psychological stress in patients being evaluated for physical complaints
(33–
35). Recent evidence has shown a significant, negative relationship between the severity of psychological symptoms of dissociation and the level of stress-induced release of neuropeptide Y. Although additional research is needed to clarify this issue, the current data raise the possibility that neuropeptide Y may also play a role in certain somatic complaints
(20,
36).
This study has several limitations. First, due to the inherent restrictions of a naturalistic study, two separate groups of subjects participated in the study. In addition, subjects completed the Clinician-Administered Dissociative States Scale after being removed from the stressful situation, and not during the stressful situation. The degree to which the time elapsed since stress exposure may have influenced the subjective ratings is not known. For example, it is possible that the Special Forces and general infantry subjects experienced symptoms of dissociation to an equal degree during stress exposure, but that the Special Forces soldiers did not report these symptoms at the poststress assessment. Such differences in reporting may be due to a personality style (or sense of machismo) that minimizes distress or discomfort—a style often seen in law enforcement personnel. It is unlikely that a reporting bias satisfactorily accounts for the current data since the Special Forces and the general infantry soldiers did not differ in their subjective reports of distress and anxiety during the training, as measured by Subjective Units of Distress Scales
(20,
21). In addition, the Special Forces soldiers, as a group, tended to report early trauma on the Brief Trauma Questionnaire. Neither of these findings suggests that these subjects tended to underreport distressing symptoms. Further, our previous reports on the neuroendocrine responses of Special Forces soldiers showed that they had less overall stress-induced release of cortisol during this training than general infantry soldiers. Thus, the subjective and objective data both point to a diminished distress response in the Special Forces subjects compared to the general infantry subjects.
Another limitation is that this study included a combination of physical stressors (physical fatigue, starvation, sleep deprivation, etc.), environmental pressures (e.g., exposure to relative extremes of heat and cold), and psychological stress. Each of these elements may have contributed to participants’ responses on the Clinician-Administered Dissociative States Scale. Thus, it is not possible to determine which symptoms of dissociation were elicited by psychological stress alone. However, survival school stress is considered to represent a reasonable analog of the combination of physical and psychological stress experienced in combat situations. The use of an ethologically valid experience for soldiers increases the likelihood that the data can enhance our understanding of combat-related peritraumatic dissociation
(37). Finally, the Health Problem List data were collected in a randomly selected group of participants. Although the significance of the regression analysis of the health problem data is noteworthy, given the small number of subjects, these findings may be influenced by the overall homogeneity of the military population and may not be representative of the civilian population. Nevertheless, military populations are routinely exposed to high-intensity stress, and these data underscore the degree to which psychological and physical responses may be linked.
In summary, symptoms of dissociation were common in healthy military subjects exposed to high-intensity stress. Individuals with a history of perceived threat to life in response to a traumatic event reported more symptoms of dissociation before experiencing the stress of survival training. Special Forces soldiers experienced significantly fewer symptoms of dissociation during stress, compared to general infantry soldiers. Symptoms of dissociation explained 41% of the variance in subjects’ physical health complaints after stress exposure.