Contrary to previously held beliefs, pregnancy does not protect women against mood and anxiety disorders. In fact, reports have indicated that 13.5%–17% of women suffer from depression in pregnancy
(1) . While the existence of anxiety disorders during pregnancy is unequivocal, the exact prevalence rates of these disorders in pregnant women remain unknown to date. Treating mood and anxiety disorders in pregnancy poses a particular challenge to clinicians. Balancing the consequences of exposure to unstable maternal mood/anxiety with the risks of prenatal exposure to psychotropic medications is critical. Either way, the fetus is “exposed,” invariably to the disease itself, and additionally to medications when pharmacological treatment is instituted. Few methodically strong studies have examined the impact of psychotropic medications administered during pregnancy on the development of the infant; even fewer have followed the exposed children over time in order to assess lasting consequences on children’s behavior.
Behavioral teratogenicity is a complex concept, variably defined. In its most simplistic version it can be divided into two general categories: internalizing and externalizing behaviors. Internalizing behaviors (emotional reactivity, depression, anxiety, irritability, and withdrawal) are behaviors that are directed internally “within the self.” Externalizing behaviors (noncompliance, verbal/physical aggression, disruptive acts, emotional outbursts) can develop into externalizing disorders. These disorders include attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder. Externalizing disorders are noticed because of their disruptive nature and are readily identified by clinicians, parents, and the school system. In contrast, children with internalizing disorders often go unrecognized and receive inadequate treatment. Internalizing disorders, after a threshold effect, may exhibit as externalizing disorders and perpetuate into adulthood
(2) . Therefore, it is of paramount importance to diagnose them and delineate risk factors associated with the development of internalizing disorders in childhood. For example, it is possible that prenatal exposure to selective serotonin reuptake inhibitors (SSRIs) changes central prenatal 5-HT levels at times of neural development, leading to altered serotonin-mediated behaviors as demonstrated in animals
(3) and humans
(4) . Furthermore, maternal depression and anxiety are key risk factors affecting childhood behaviors
(5 –
11) .
In this study we prospectively examined the relationship between prenatal SSRI exposure and internalizing behaviors in 4-year-old children and report the influence of maternal mood on the children’s behavior. The externalizing behaviors are being reported independently.
Literature on the effects of prenatal exposure to psychotropic medication is conflicting. Some studies have found no negative effects of prenatal exposure on child development. Nulman and colleagues
(12,
13) examined children between 15 and 86 months of age who had been exposed throughout gestation to tricyclic antidepressants or fluoxetine, comparing them with an unexposed group. No differences were found in the children’s global IQ, language development, or behavioral development as measured by the Child Behavior Checklist
(14) . Mattson and colleagues
(15) reported no differences in cognition and neurobehavioral development between children 4–6 years of age prenatally exposed to fluoxetine and nonexposed children. In contrast, a study by Casper and colleagues
(16) reported that children with prenatal exposure to SSRIs had significantly lower levels of psychomotor development and motor control than those of depressed, nonmedicated mothers.
Although the bulk of the literature focuses on depressed/anxious maternal mood as being a significant and well-studied risk factor for altered children’s behavior
(5 –
11), some studies present reports to the contrary
(17,
18) . Murray and colleagues showed that 5-year-old children exposed to postpartum depressed mothers demonstrated no deficits in cognitive tasks
(17) . Van den Bergh and Marcoen
(18) found no significant associations between maternal anxiety and internalizing behaviors in 8- and 9-year-old children as reported by parents and caregivers. However, they did find that children’s externalizing behaviors were significantly related to antenatal maternal anxiety. Another study, conversely, found that antenatal maternal anxiety predicted behavioral and emotional problems in 4-year-old children
(11) . These studies demonstrate that inconsistencies exist in the literature regarding long-term behavioral outcomes in children exposed to unstable maternal mood/anxiety in pregnancy and postpartum.
The present study is the fourth wave of prospective analyses of children exposed in utero to SSRIs alone and a combination of SSRIs and clonazepam
(4,
19,
20) . At birth, infants exposed to severe maternal depression and anxiety along with SSRIs and clonazepam in utero showed increased symptoms of transient poor neonatal adaptation relative to nonexposed infants
(4,
19) . The same cohort of infants continued to show negative effects (affect expressivity) of exposure to the same combination of medications at 3 months
(20) . Furthermore, this pattern persisted when the infants were examined at 8 months of age (Reebye PN et al., unpublished 2004 study). Maternal mood was additionally assessed at both 3 and 8 months postpartum within this cohort and was not correlated with infant expressivity at these times.
We present here the consequences of exposure to psychotropic medications in the same cohort of children at 4 and 5 years of age. Specifically, we studied the internalizing behaviors of children exposed to either SSRIs alone or SSRIs in combination with clonazepam and compared them with a nonexposed group. Furthermore, we examined the effects of maternal mood/anxiety on the internalizing behaviors of the children.
Method
Participants
Ethics approval was obtained from the University of British Columbia Research Ethics Board and the Children’s and Women’s Health Centre of British Columbia Research Review Committee. After a description of the study was provided, written informed consent was obtained both during the initial perinatal study and when the participants were studied 4 years later.
All participants were initially recruited between 1997 and 1999. The exposed group was recruited from the Reproductive Mental Health Program at British Columbia Women’s Hospital in Vancouver. Eighty-two expectant mothers from this program were approached regarding participation in the present study, of which 52 were eligible and agreed to participate. Of these 52 women, one miscarried and five discontinued the study, leaving a total of 46 women who comprised the original cohort. When the children reached 4–5 years of age their mothers were contacted again and asked to participate in a follow-up investigation, at which time the internalizing behaviors of their children were assessed. Between birth and this follow-up visit 24 of the mother-infant dyads in the exposed group were lost due to attrition, leaving us with complete data on 22 dyads. The comparison group of nondepressed, nonmedicated, healthy mothers and their infants was recruited after delivery from pediatricians’ offices. Initially, 23 mother-infant dyads entered the study in the comparison group, however, nine of these pairs did not return for the follow-up visit 4 years later, leaving 14 comparison dyads.
Thus, the participants for the present investigation included 36 dyads: 22 children of depressed/anxious mothers exposed to psychotropic medications during pregnancy (the exposed group) and 14 children of healthy, nondepressed, and nonmedicated mothers (the comparison group). Of the 22 mothers treated with SSRIs, five were prescribed fluoxetine, 14 paroxetine, and three sertraline. Furthermore, nine of these women received the benzodiazepine clonazepam as well (the SSRI/clonazepam group), leaving 13 children prenatally exposed solely to SSRIs (the SSRI only group).
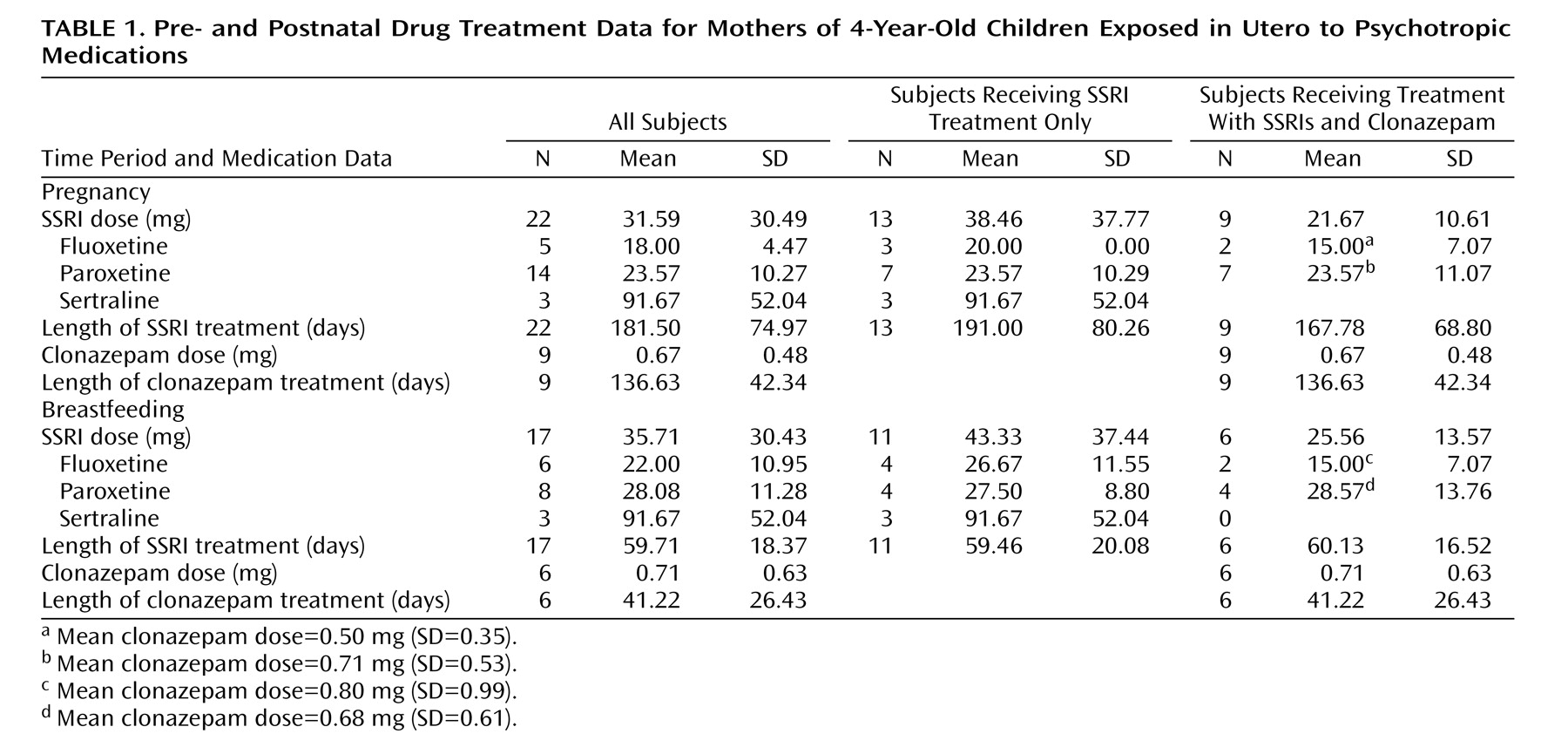
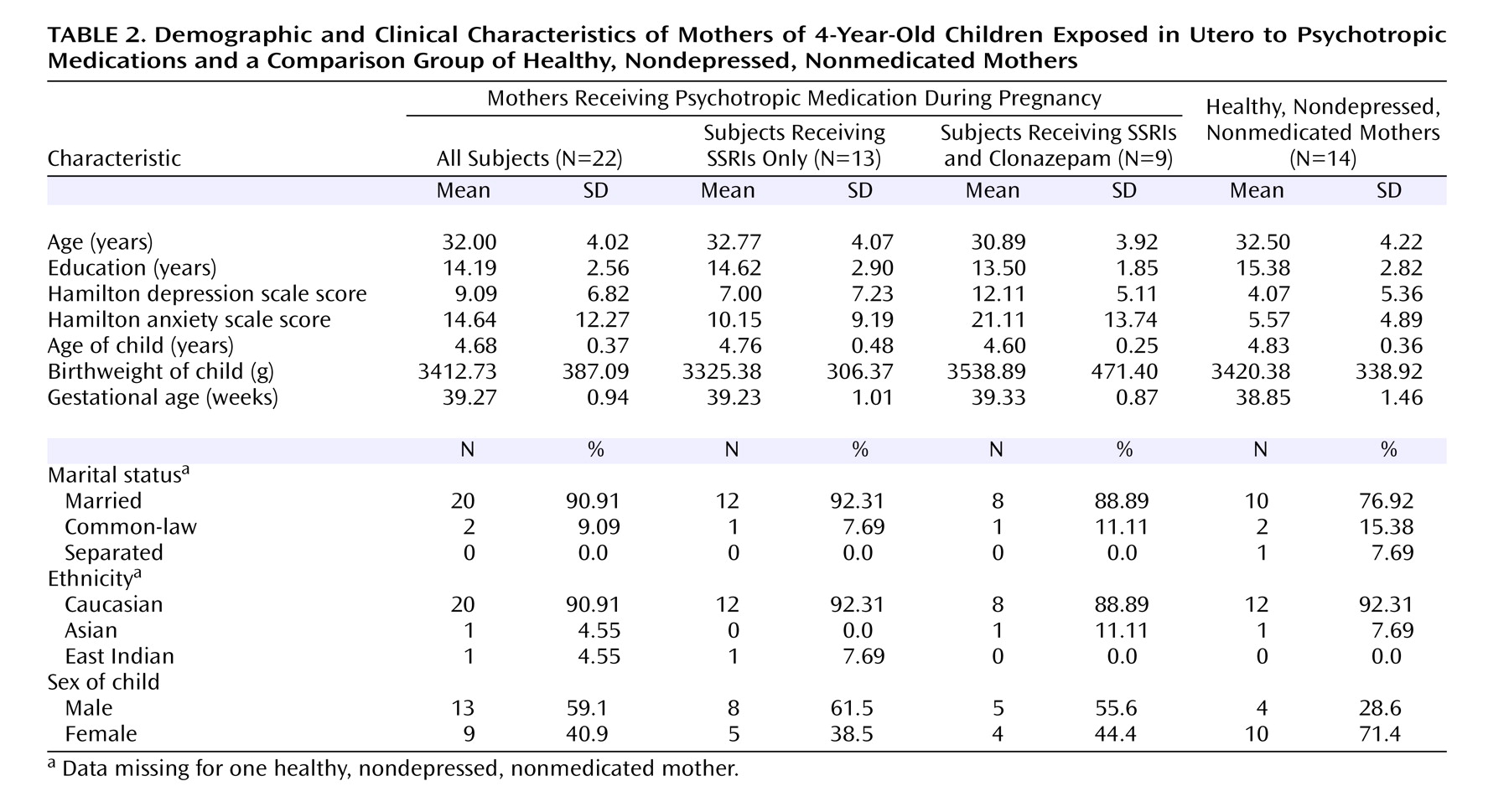
Table 1 depicts the average dosages and length of prenatal exposure for each medication. Participant demographic information is presented in
Table 2 . There were no differences among the groups in demographic characteristics.
Procedure
Prior to enrollment, participants were contacted, and a detailed description of the study was provided. The study took place at the Centre for Community Child Health Research in Vancouver. This research facility is specifically set up and designed for conducting biobehavioral studies of children. The lab is equipped with a one-way mirror that allows observations of mothers with their children during study procedures. Once maternal consent was obtained, Child-Teacher Report Forms were mailed to the children’s teachers. Next, demographic information was recorded, then the interaction between mother and child was observed. After a break, the mothers completed the Child Behavior Checklist. Last, maternal mental health questionnaires (i.e., Hamilton depression and anxiety scales) were administered by a blind rater.
Measures
For the purposes of the current study, only the subscales of the Child Behavior Checklist
(14) and Child-Teacher Report Form
(14) specific to internalizing behaviors are reported. These subscales include ratings regarding how emotionally reactive, anxious/depressed, and withdrawn the child is as well as how frequently the child makes somatic complaints. There is also a total score for internalizing behaviors, which incorporates all of these subscores.
These measures provide standardized ratings and descriptive details of the functioning of children between the ages of 1.5 and 5 years, as seen by parents or parent surrogates (Child Behavior Checklist) and caregivers or preschool teachers (Child-Teacher Report Form). These measures have been shown to have high test-retest reliability (r=0.85 for the Child Behavior Checklist, and r=0.81 for the Child-Teacher Report Form) and interrater reliability (r=0.61 and r=0.65, respectively) as well as content, criterion-related, and construct validity
(14) . The Child-Teacher Report Form contains essentially the same problem items as the Child Behavior Checklist. However, items on the Child Behavior Checklist that refer to family situations are altered on the Child-Teacher Report Form to reference group situations.
The respondent rates each problem item on a scale from zero to two, with zero indicating not true for the child, one suggesting that the item is somewhat or sometimes true for the child, and two indicating very true or often true of the child during the preceding 2 months. Raw scores on each subscale are then converted to standardized T scores for interpretation: T scores <65 fall in the normal range, the borderline clinical range is from 65–69, and T scores >69 are considered to be in the clinical range
(14) .
Mother and child interaction was assessed by using the Crowell procedure, which describes a systematic approach to structuring interaction between a mother and her child and of coding certain variables during the interaction (Crowell JA, Rosenberg DM, unpublished 1985 manual). For the purposes of the present study, the Crowell procedure was used to augment the parent and teacher/caregiver reports of the children’s behaviors with a more objective rating made by a clinician in a structured laboratory setting. All sessions, which were approximately 35 minutes in duration, were videotaped and later coded by a trained infant psychiatrist blind to both groups. The content of the videotapes was analyzed for three aspects of a child’s affect: positivity (whether there was a substantial period of positive regard and sharing of happy feelings on the part of the child toward the mother), withdrawal, and irritability. Scores for these three responses are rated on a Likert-type scale ranging from zero to four, with zero indicating that the behavior was not observed, one being very low, and four being very high.
The Hamilton Rating Scale for Depression is a 21-item, clinician-administered scale that measures the severity of depression in adults. Scores on this scale can range from 0–63, with higher scores being associated with higher levels of depression in the patient. Scores ranging from 0–7 suggest no or minimal levels of depression, 8–17 indicate mild depression, 18–25 suggest moderate depression, and scores of 26 and above are associated with severe depression. Interrater reliability on this scale has been shown to range from 0.84–0.90.
The Hamilton Anxiety Rating Scale is a 14-item, clinician-administered scale that measures the severity of anxiety. Total scores on this scale have a possible range of 0–56, with higher scores on this measure being associated with higher levels of anxiety in the patient. Scores ranging from 0–7 suggest no or minimal levels of anxiety, while scores of 8 and above indicate the presence of anxiety. Average interrater reliability on this scale has been shown to be 0.89.
Data Analysis
Analyses were conducted for internalizing behaviors from three different sources: as reported by parents, caregivers, and as objectively coded from mother and child interactions by a clinician. For each source, an analysis was done comparing the exposed to the comparison group. Further, as previous findings have demonstrated an effect of prenatal exposure to clonazepam in addition to SSRIs (4, 19, 20), analyses were conducted in the present study comparing the SSRI only and SSRI/clonazepam groups. It is important to note that the influence of maternal mood and anxiety were factored into all analyses. The relationship between maternal mood/anxiety and the internalizing behaviors of the children was additionally examined. Ordered logistic regressions, independent-sample t tests, and univariate analyses of variance (ANOVAs) were used to compare outcomes between groups. Pearson correlations were used to determine associations between maternal mood and child behaviors. All tests were two-tailed comparisons.
Results
Maternal Mood
Mothers of children exposed in utero to psychotropic medications demonstrated significantly higher levels of depressed mood (t=2.33, df=34, p<0.05) and anxiety (t=3.10, df=29.80, p<0.01) than did the comparison group mothers. Furthermore, mothers treated with SSRIs in combination with clonazepam showed higher levels of depressed mood (t=2.03, df=21, p=0.055) and anxiety (t=2.44, df=21, p<0.05) than mothers treated with SSRIs alone.
Despite pharmacological treatment, the mothers of the exposed children remained symptomatic during pregnancy: 64% (N=14 of 22) scored greater than 7 on the Hamilton anxiety scale, and 73% (N=16 of 22) scored greater than 7 on the Hamilton depression scale. In the postpartum period, all 22 mothers of the exposed children were receiving medications at the 4-year visit, and nine had not changed the medications prescribed to them during pregnancy. Of the remaining 13, 12 were taking antidepressants, and one was taking clonazepam only. Despite their ongoing treatment, they were still symptomatic at the 4-year visit, with 59% (N=13 of 22) scoring greater than 7 on the Hamilton anxiety scale and 50% (N=11 of 22) scoring higher than 7 on the Hamilton depression scale.
Internalizing Behaviors
Parent and teacher/caregiver ratings
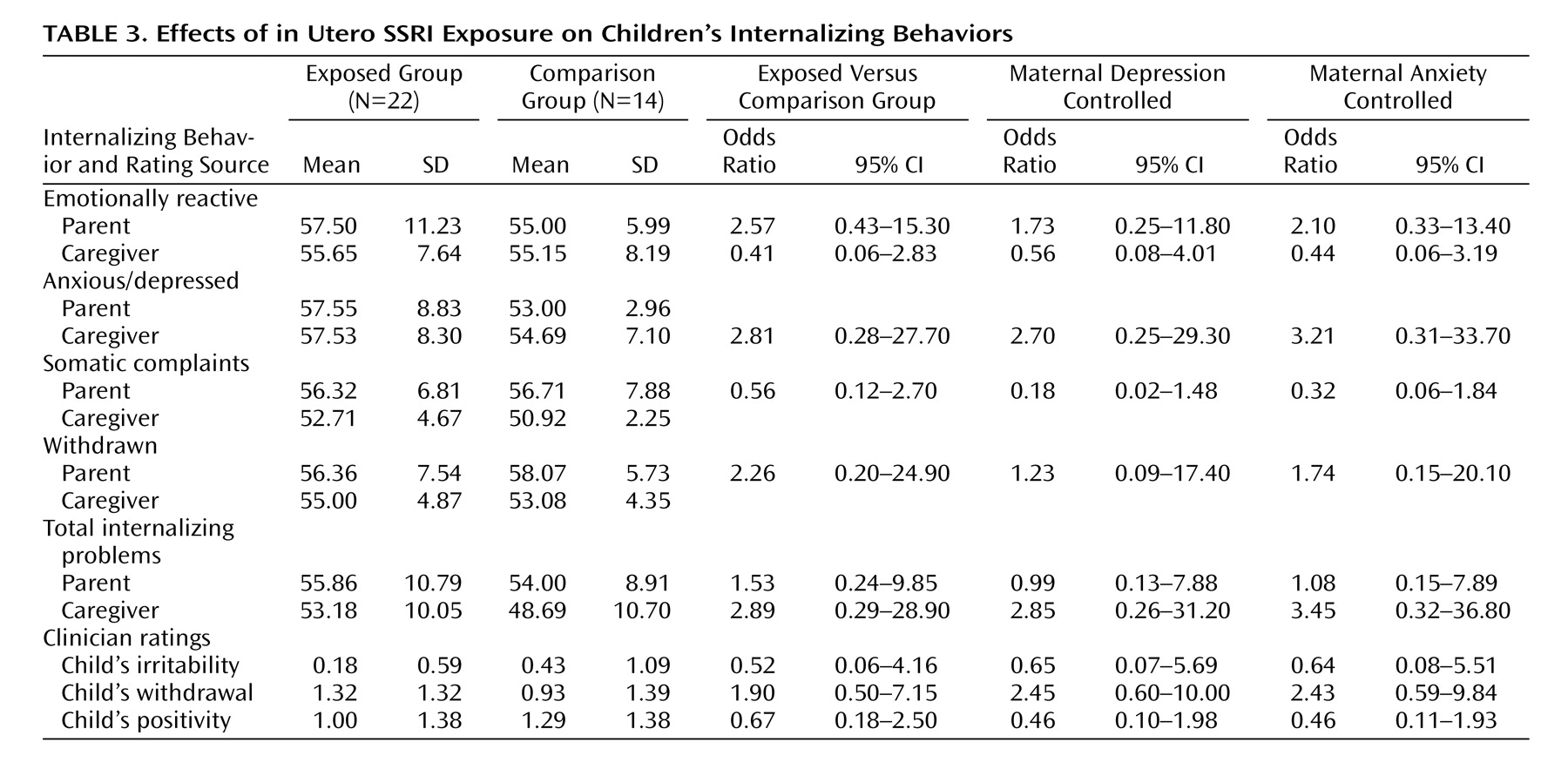
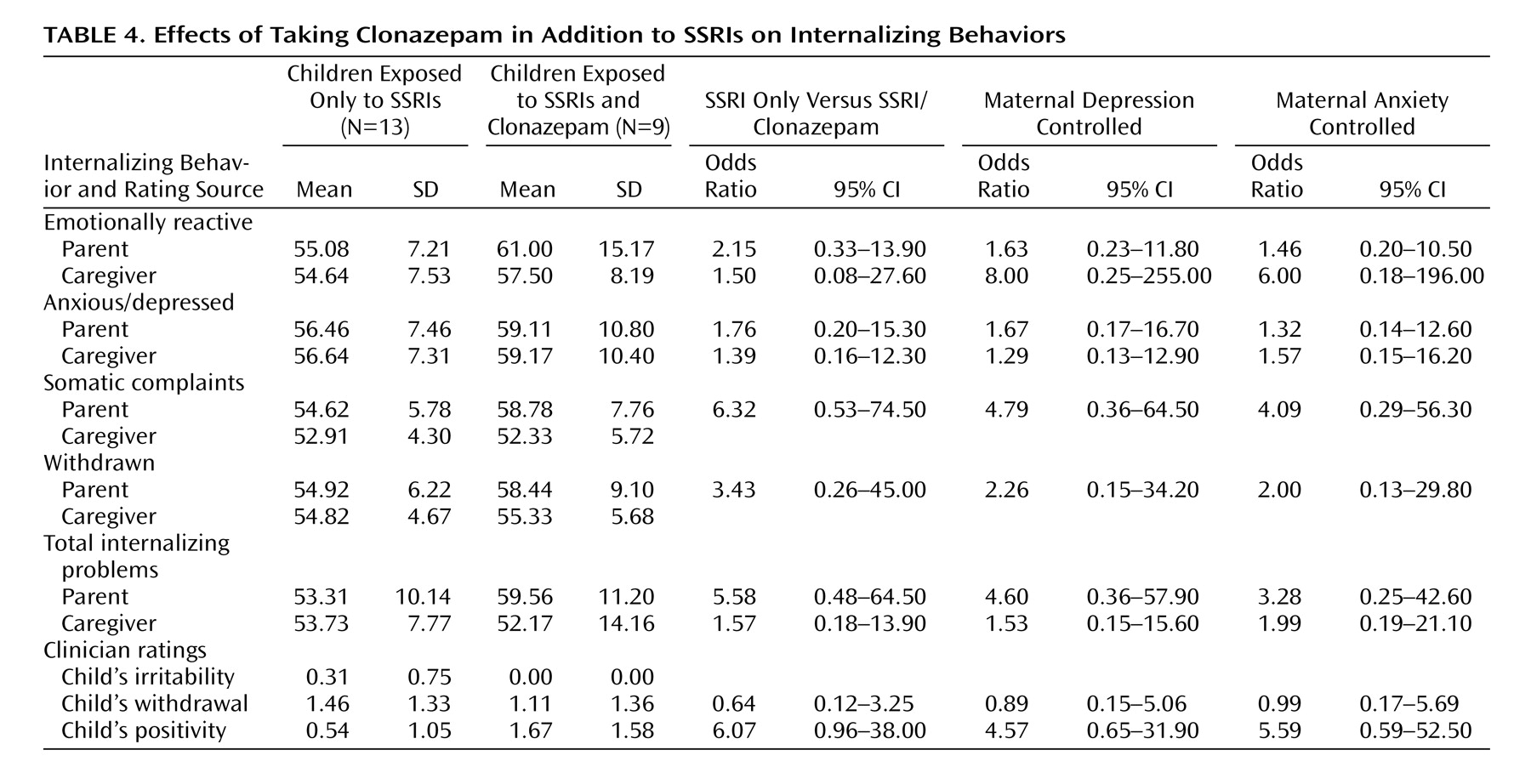
When comparing the exposed and the nonexposed children, no statistically significant differences were found in parent or caregiver ratings of internalizing behaviors (Table 3). Similarly, there were no significant differences found in parent or caregiver ratings of internalizing behaviors between children exposed to SSRIs only and those exposed to SSRIs and clonazepam (Table 4). However, we found that there were children in both the exposed (18%) and comparison (14%) groups that exhibited clinically significant total internalizing behavior scores as reported by both parents as well as teachers.
Among the entire cohort at the time of the follow-up assessment, increased parental—but not teacher—reports of total child internalizing behaviors were associated with maternal symptoms of depression (F=5.43, df=1, 36, p<0.05) and anxiety (F=6.88, df=1, 36, p<0.05). This relationship remained even when prenatal exposure was added to the regression model.
To further examine the impact of maternal depression and anxiety in the presence of prenatal medication exposure, the relationship between these symptoms and parent-reported child behavior was examined within the exposed group. Higher levels of maternal anxiety were significantly associated with increased total internalizing behaviors in the children (r=0.57, p<0.05), while depressed maternal mood was only slightly related to child behavior (r=0.41, p=0.055). Again, these effects did not change when prenatal medication exposure was added to the regression model. Levels of internalizing behaviors were not significantly associated with maternal mood in the nonexposed group.
Clinician ratings
A clinician coded the children’s positivity, withdrawal, and irritability during a structured laboratory interaction between mothers and their children. When comparing the exposed group to the comparison subjects, differences in behavior between groups were not significant (
Table 3 . When examining the effects of the type of drug administered, no significant differences in mother-child interaction were found between the SSRI only and SSRI/clonazepam groups (
Table 4 ). Of the three behaviors derived from the Crowell procedure, for the entire group only child positivity during the task was associated with maternal anxiety levels (r=0.36, p<0.05). None of the clinician-rated behaviors were related to maternal levels of depression.
Again, to further examine the impact of maternal depression and anxiety following prenatal medication exposure, the relationship between these symptoms and child behavior was examined within the exposed group. In this group, higher levels of child positivity were associated with increased levels of maternal depression (r=0.59, p<0.01) and anxiety (r=0.61, p<0.01). The remaining child behavior variables derived from this structured laboratory setting were not significantly associated with maternal mood. It is important to note that among nonexposed children none of the child behaviors were associated with maternal mood.
Discussion
Levels of childhood internalizing behaviors, as reported by parents and teachers and as rated by a clinician in a structured laboratory setting, were not significantly different between 4-year-olds with and without prenatal SSRI exposure. Similarly, outcomes between children with SSRI exposure alone versus in combination with clonazepam were also not substantially different. However, we established that there was a relationship between maternal mood/anxiety and the internalizing behaviors of the children. Those mothers who were depressed and anxious reported more problematic internalizing behaviors in their children than those who were not. In addition, although the correlation between increased child positivity and maternal depression/anxiety is seemingly counterintuitive, we can speculate that those children whose mothers were chronically depressed/anxious over a period of 4 years may have been attempting to engage their mothers by demonstrating increased positivity. This was specifically applicable when examining the cohort as a whole and the exposed group separately, but not the comparison group, likely because there was less psychopathology in the comparison group of mothers and their children. While this association between maternal mood and child behavior may not be causally related, it does highlight the importance of closely monitoring long-term developmental and behavioral outcomes of children exposed to mothers with chronic mental illness.
In this cohort, we have followed longitudinally the children’s affect expressivity, which constitutes one aspect of internalizing behaviors. At 3 and 8 months of age clear differences in affect expressivity existed between the infants prenatally exposed to SSRIs only and those exposed to a combination of SSRIs and clonazepam. This changed at 4 years, at which time maternal mood seemed to play a more significant role than prenatal drug exposure, whether the exposure was to SSRIs alone or in combination with clonazepam. The rationale for this change is unclear at this time, and further research is needed in order to clarify this finding. However, one possible explanation could be that the adverse effects of prenatal exposure to clonazepam may not persist to age 4. Our observations are consistent with those from earlier studies indicating an absence of impaired behavioral development in children with prenatal exposure to psychotropic medications
(12,
13,
15) .
Our study also adds to the literature reporting on relationships between maternal mood/anxiety and child development. Our findings are consistent with the extant literature emphasizing negative effects on children of unstable maternal mood
(5 –
11) . Of particular significance, our results are in line with those reported by Field and colleagues
(10), which specifically indicated a relationship between maternal depression and increased internalizing problems in children. While prenatal medication exposure was not associated with increased levels of internalizing behaviors in this study, a relationship between depressed and anxious maternal mood and internalizing problems in children was noteworthy. Thus, even in the presence of perinatal pharmacological therapy, altered maternal mood continued to have an impact on child behavior. It is important to note, since we know that the women in the present study remained chronically mentally ill with recurrent, relapsing episodes, this impact was likely a critical factor negatively influencing the development of the children seen in the present study.
A number of limitations of this study should be noted. Since several studies have specifically addressed the effects of prenatal exposure on psychomotor development of children, our present study focused on examining one specific aspect of child development, namely, internalizing behaviors. The size of this follow-up cohort was small. Moreover, we were not able to study children of depressed mothers who were not treated pharmacologically, which would have assisted our ability to separate the effects of maternal mood from those of prenatal medication exposure.
Clinical Implications/Conclusion
Although conclusive statements on the safety of psychotropic medications during pregnancy cannot be made, when a clinician is faced with the dilemma of managing mentally ill pregnant women, no decision is risk free. At the present time, these women are almost always treated with pharmacotherapy. Clearly, this treatment option is not without the attendant risks, both for the mother as well as the baby. We have attempted to answer the question of whether or not prenatal exposure in women with severe psychiatric illness has consequences for children 4 years later. There appears to be no direct correlation. However, what we found is that regardless of pharmacological treatment in pregnancy, maternal mood and anxiety 4 years later remained a significant determinant of childhood internalizing behaviors. This finding has a crucial message for caregivers. We endorse early intervention, close follow-up, and monitoring of maternal mood and anxiety during pregnancy, postpartum, and beyond.