Children account for approximately 31% of all burn injuries in the United States
(1) . Few studies of young children have examined psychological, physiological, and behavioral responses to burns. This is due, in part, to the difficulty of identifying symptoms of posttraumatic stress in preschoolers. This multidisciplinary collaboration of child psychiatrists, developmental psychologists, surgeons, and nurses caring for acutely burn-injured children and their families’ attempts to fill in some of these gaps in knowledge.
Posttraumatic stress symptoms have been a focus of research with older children, with progress occurring in psychological and pharmacological treatments. Little research has been done with young children, although they account for over 40% of all pediatric burn injuries
(1) . This study accounts for most of the burns suffered by young children. In 2003, there were 42,149 burn injuries (29% of all pediatric burns) among children 1–2 years old and 17,412 burn injuries (12% of all pediatric burns) among children 3–4 years old.
Among older children with burns, between 25% and 33% eventually developed PTSD, and 53% met full or partial lifetime PTSD DSM-III criteria
(2) . An article by Terr
(3) was the first to describe the differences in PTSD symptoms in a study of young kidnapped children in Chowchilla, Calif. An initial article described “posttraumatic play” and posttraumatic games in 14 of 23 children ages 7 months to 17 years. In a later clinical study of children under 5, a study by Terr
(4) found that children less than 28–36 months old at the time of the trauma could not fully verbalize their traumatic experience, but memories expressed in posttraumatic play revealed signs of trauma.
Our group
(5) found that children with burns, ages 12–48 months, manifested the full range of acute stress symptoms. With the use of path analysis
(6), we reported factors contributing to the development of acute stress symptoms in these very young burned children. The analytic model yielded two independent pathways to acute stress symptoms:
From the size of the burn to the mean pulse rate in the hospital to the burned children’s acute stress symptoms
From the children’s pain as a stressor to parental acute stress to the emergence of their children’s acute stress symptoms
Studies of children burned at young ages have described major developmental stresses for the child and the mother during the course of treatment
(7 –
9) . Meyer et al.
(10) studied young burned children and found that burned children between the ages of 2 and 3 had increased internalizing behaviors, as measured by the Child Behavior Checklist; these children had high rates of social withdrawal and depressive behaviors. An article by Alfred
(11), in collaboration with our group, compared our study
(2,
12) with national diagnostic data and analyzed these data by age at the time of the burn. The results in the report by Alfred
(11) showed high rates of psychopathology among those burned at younger ages. In particular, the study reported higher rates of separation anxiety and enuresis in children burned at young ages. Burned children ages 4 and younger had a mean of total PTSD symptoms comparable to those in the older group. Although it is possible that the response to burns may be expressed differentially in younger children, the symptoms in these children did result in impairments in their psychosocial functioning.
There is an emerging literature on the developmental importance of social smiling and positive vocalizations in young children. For example, Rosenbaum et al.
(13) found that children of patients with panic disorder and depression smiled less than comparison subjects. Also, Kagan et al.
(14) found that children who had been categorized as behaviorally highly reactive as infants and who showed fewer smiles and vocalizations in early childhood were more likely to be rated by their mothers as showing anxiety symptoms at age 7. Finally, Schwartz et al.
(15) found that children categorized as inhibited at 2 years displayed fewer smiles and vocalizations, and at age 13, they scored lower on the Child Behavior Checklist on total externalizing, delinquent behavior, and aggressive behavior scales. As described in an article by Kagan
(16), children who are temperamentally inhibited and who demonstrate a lower frequency of social smiling and vocalizations are vulnerable to the later development of anxiety.
Children who experience a stressful life event may react with disturbances in their biological stress system with “increased baseline activity of catecholamines as well as inherent temperamental traits”
(17) . Another article by DeBellis et al.
(18) suggested that traumatic experiences are also associated with “adverse brain development” in children who were maltreated. Kagan et al.
(16,
19 –21) have studied groups of young children in a longitudinal study to understand the physiological correlates of inhibition. Inhibited young children who react to stress with avoidance and anxiety show greater reactivity in the cardiovascular system: they have larger increases in their heart rate and blood pressure
(16,
19 –21) .
Additionally, symptoms of PTSD appear to be influenced by the excitability of the CNS, specifically the amygdala and its projections. Several decades of research have revealed that a primary function of the amygdala is to respond to unfamiliar events
(22,
23) . When the amygdala is activated by unfamiliar events, behavioral immobility, retreating, and crying are the typical reactions of children. Peripheral sympathetic responses include increased heart rate and blood pressure. The laboratory protocol used in the current study involved presenting children with unfamiliar events or situations and observing their behavior and physiology.
Almost all that has been learned about burns or other trauma in young children is from cross-sectional research, leaving open the potential for bias in long-term outcomes that are not longitudinal. Reassessing children over time prevents this kind of bias. The goal of the current longitudinal study is to provide more than a simple “snapshot” assessment by carefully assessing the unfolding of traumatic stress symptoms over time through psychological, physiological, and behavioral measures and assessing how traumatic stress symptoms influence later developmental outcomes.
Method
Subject Selection
The families of 72 children ages 12–48 months who were admitted to the Shriners Burns Hospital in Boston with an acute burn were contacted by the principal investigator (F.J.S.) or his designee within 3 days of admission or when the child was considered to be medically stable and was invited to participate in the study. Excluded from the study were children with non-English-speaking parents, neurological impairment, mental retardation, or other chronic conditions that might have prevented completion of the assessment or participation in the evaluation by the infant study at Harvard. After a complete description of the study was given to the families, written informed consent was obtained from a parent.
Between January 2001 and November 2004, 193 children, ages 12–48 months, were admitted to the acute burn unit. Ninety-one children did not meet eligibility criteria; the most common reason for exclusion was that the parents did not speak English. Seventy-two parents consented to participate in the study, and 30 parents declined. Of the 72 subjects who completed the initial interview for the project, 32 participated in the follow-up assessment at our laboratory. Thirty-six subjects declined to participate in the laboratory assessment, the usual reason being insufficient free time for the mothers of young children. An additional four subjects were lost to follow-up because the families moved or their telephone numbers were disconnected. Finally, two of the follow-up assessments were found to be unusable as a result of poor-quality videotapes. Thus, the final analyzed group size for the follow-up assessment at the laboratory, which included smiles and vocalizations, was 30 subjects.
Informed Consent and Privacy Protection
The institutional review boards of Massachusetts General Hospital and Harvard University approved the study, including its privacy protection. The parents provided informed consent for the study and its provisions for privacy protection under Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulations.
Clinical Assessments
Procedure
The principal investigator (F.J.S.) or his designee interviewed the burned child’s parents and asked them to complete several paper-and-pencil questionnaires to be described. In addition, the study nurse summarized physiological data from the medical record about the patient. Approximately 1 month after the child’s discharge from the hospital, the parents of the burned patient repeated the interview and paper-and-pencil questionnaires and the children were assessed at Harvard University.
Laboratory assessment
A research assistant gathered and videotaped behavioral and physiological data on the child with the parent present. The videotapes were later coded for several variables, including the frequencies of smiles and vocalizations. One of the authors (J.K.) rated on a 3-point scale the frequency of vocalizing (or talking, for older children) and smiling over the entire protocol. This rater had made similar ratings on a separate group of 350 children, and an independent coder had done the same. The interrater reliability for both variables was more than 0.90
(24) .
The child’s display of fear to five stimuli was coded, where fear referred to crying or withdrawal to the incentives. The incentives were attachment of the heart rate electrodes and the blood pressure cuff, being approached by a stranger, a request to touch and pick up a rubber snake, and reluctance to approach a person in a clown costume who invited the child to approach and play. In addition, one of the authors (J.K.) rated each child on a 4-point scale for the degree of inhibition (1=relaxed, not anxious, to 4=anxious). The high reliability of the coding of a fear response and the rating of inhibition had also been established earlier on the same independent group just mentioned (Kagan and Snidman, reference
24 ).
The procedures were first explained to the parent while the child played with toys on the floor. The incentives for fear were meant to be moderately provocative of anxiety. The parent could request the termination of any procedure, but no parent did so. The child was seated in a chair appropriate for his or her age (a high chair or a small child’s chair). Three electrodes for measuring the heart rate were placed in a standard configuration on the chest. A 1-minute heart rate baseline measurement was taken while the child was sitting, followed by a 1-minute baseline measurement while the child stood. The experimenter then placed a blood pressure cuff on the child’s arm, and baseline measures were obtained with sitting and standing postures. These biological measures were followed by the introduction of several novel stimuli. In the third procedure, a person covered in a black cloth entered the room, stood by the door for 30 seconds, approached the seated child slowly for another 30 seconds, spoke to the child for 30 seconds, and then left the room. The examiner then presented the child with a rubber snake in a small glass jar. After waiting 15 seconds, she invited the child to reach in and remove the snake if the child had not already done so. Finally, the examiner told the child that he or she could play with the toys on the floor again. Once the child was playing, a person in a clown costume entered the room and sat close to the door, talking about herself in a neutral tone of voice (“I’m a clown. Don’t I have a funny costume?”). After 30 seconds, if the child had not approached, the clown held out two small toy animals and asked the child to come play with them. The clown left after 2 minutes. If the child became fretful or cried during any procedure, it was stopped, and the experimenter and parent comforted the child.
Diagnostic Interview for Children and Adolescents
To gather data on PTSD, which is most frequently diagnosed in traumatized children in this age range
(25 –
28), parents were interviewed with the module on this disorder from the Diagnostic Interview for Children and Adolescents (DICA). This semistructured interview schedule has been widely used in clinical and nonclinical groups and has demonstrated reliability and validity
(29 –
31) . It has been used in a number of different groups of traumatized children, including burn survivors
(2,
12) and victims of an earthquake
(32) .
Data from medical records
Primary nurses recorded the child’s heart rate and level of pain as part of the standard of care during the hospitalization. The heart rate was recorded at least every 4 hours, and the primary nurse evaluated pain intensity every 8 hours on a scale of 0 to 10 (with 10 being the highest level of pain). For young children, the nurses used the Visual Analogue Scale to evaluate pain
(33) . All nurses received formal training on the Visual Analogue Scale, a standard of care followed by Shriners Burn Hospital in order to be compliant with the Joint Commission Accreditation of Health Care Organizations.
At a later point in time, nurses from the study staff compiled the heart rate and pain data as well as information on medical procedures (e.g., the number of dressing changes, the number of days in the hospital, and the number of surgeries). The stress of medical intervention was defined as the frequency of dressing changes and the average amount of pain that the child experienced. The frequency of dressing changes was obtained from chart reviews and scored as the mean number of dressing changes per week during the child’s hospitalization. Our variables for heart rate and pain are the mean for all observations of these respective variables over the course of the child’s hospitalization. The child’s total body surface area burned was computed by the child’s physician. For burn injuries, the standard scoring is by percentage of the burn on the total body surface area, specifying anatomic locations on a human figure chart, front and back, and including delineation of specific areas of facial, extremity, perineal, truncal, and other burns
(34) .
Results
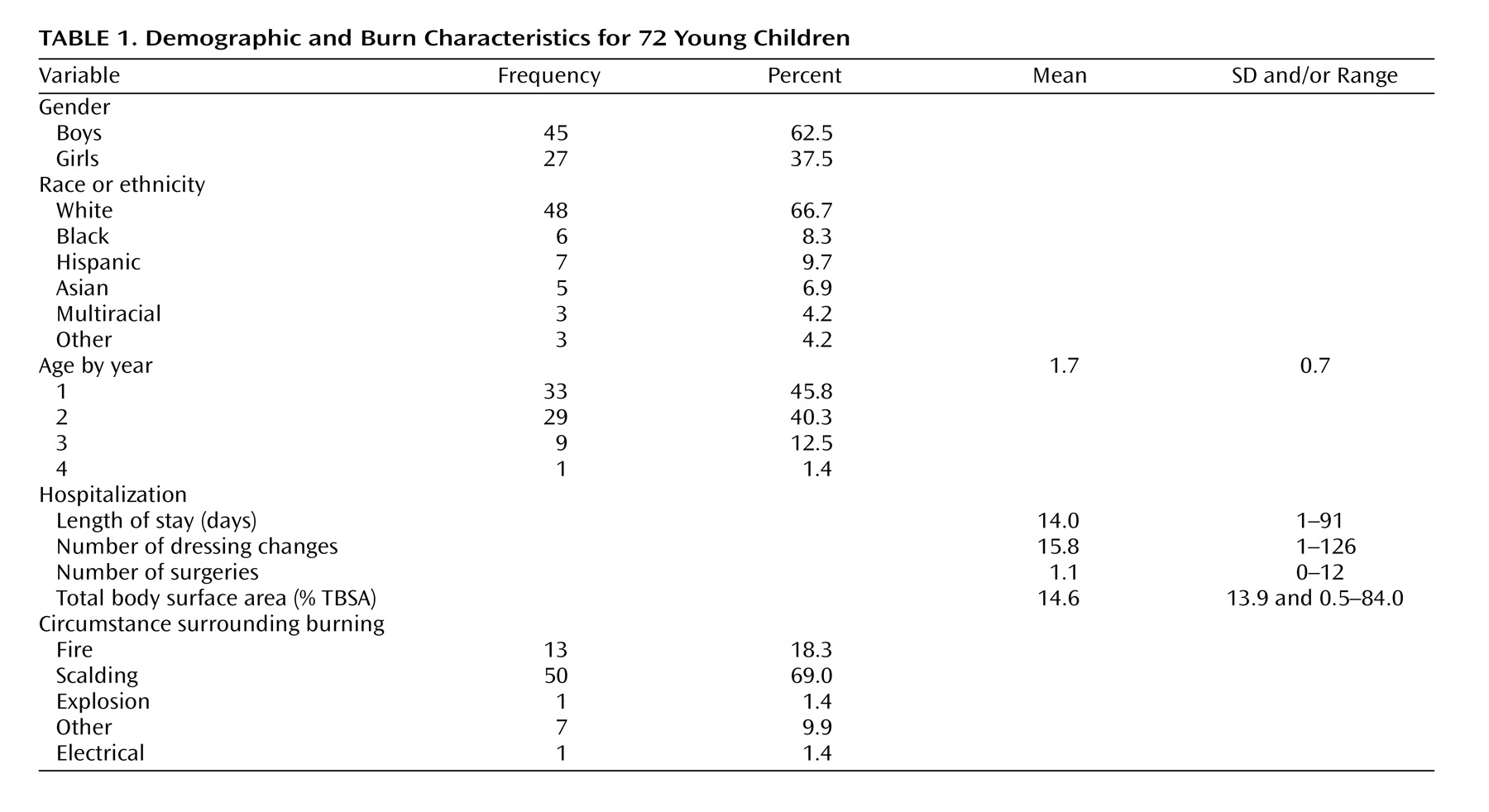
Demographic and burn characteristics are presented in
Table 1 . The study group included more boys (62.5%) than girls and more whites (66.7%) than ethnic minorities. The study group, which was representative of the hospital’s population, had an average total body surface area burned of less than 20% (burn size: mean=14.6%, SD=13.9%), with a range of 0.5%–84.0%. Children ages 12–48 months who were admitted to the acute unit during this time had an average total body surface area burned of 14.3%. The average age of the subjects was very young, with a mean of 1.7 years (SD=0.7): 45.8% of the subjects were 1-year-olds.
In general, the young children’s affective responses to the three separate fear measures differed in quality and in intensity. Most children stopped whatever play they were engaged in when either the stranger or clown first entered the room and continued to stare with expressions ranging from neutral to increasing wariness as the unusual person approached them. A few of the children who looked unperturbed and relaxed spoke to the stranger or clown, whereas a small number became more distressed and reached for or went to their mother and fretted or cried and were comforted. Most children greeted the snake with curiosity, and many were willing to reach in the small jar to take it out.
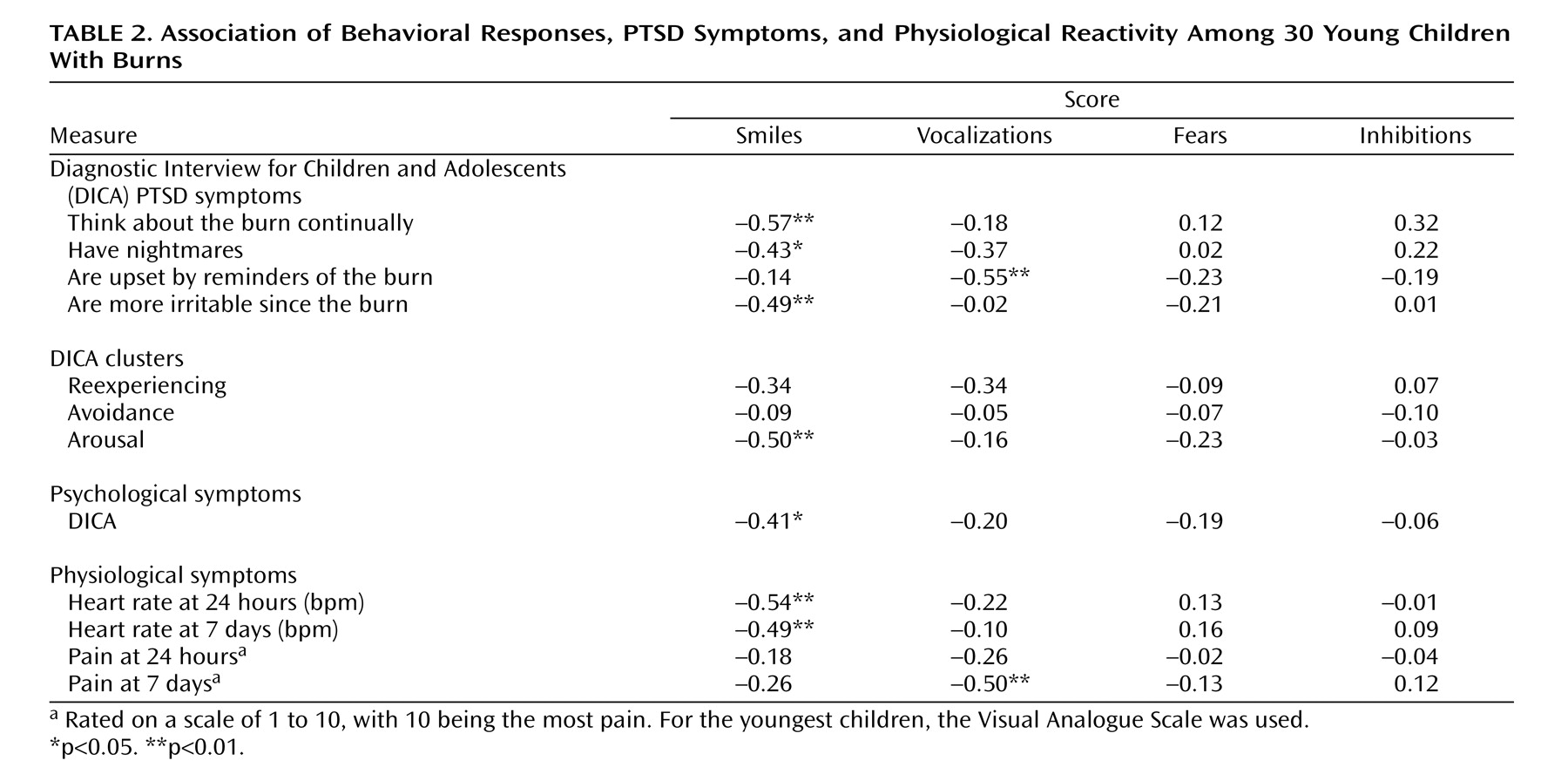
Table 2 reveals that many of the symptoms of PTSD assessed immediately after the burn were associated with behavioral measures 1 month later. The children of the parents who said the child thought about the burn regularly smiled less when assessed 1 month later (r=–0.57, p<0.01). The children who were described as being upset by reminders of the burn vocalized less in the laboratory 1 month later (r=–0.55, p<0.01). The children who were described as more irritable in the hospital smiled less in the laboratory 1 month later (r=−0.49, p<0.01). The higher the DICA arousal cluster score during hospitalization, the less likely the child smiled 1 month after hospitalization (r=–0.50, p<0.01). The higher the heart rate was at 24 hours (r=–0.54, p<0.01) and at 7 days (r=–0.49, p<0.01), the less frequent the spontaneous smiles 1 month later. Finally, the child’s rating of pain at 24 hours was related to reduced vocalizations 1 month later (r=–0.50, p<0.01).
Discussion
Characterization of posttraumatic stress in young children has been fraught with difficulties. Children at this age are largely nonverbal, or their verbal productions are not reliable. Characterization of other conditions in early childhood has varied. Pain assessment uses multiple modalities, including observational ratings and physiological and questionnaire data
(35) . Assessment of major depression in young children, after a long debate, settled on using symptoms similar to those for major depression in older children and adults
(36) . The limited evidence gathered so far for posttraumatic stress in young children supports use of the same criteria as for older patients,
but fewer criteria are required
(37) . The present study sought to clarify whether, similar to pain assessment, physiological and other observational variables can assist in identifying posttraumatic stress in young children.
Children who exhibited more reexperiencing and arousal symptoms shortly after a burn displayed fewer smiles and vocalizations in a laboratory setting 1 month later. These measures may be a sign of developmental risk and the need for intervention. This study demonstrates that psychological and physiological measures taken during hospitalization have a modest link to later psychological states such as mood, anxiety, sleep, conduct, elimination, learning, and attention problems—all of which have been found to be present in children after injuries and other trauma
(12,
32,
38,
39) .
The vast majority of PTSD studies are based on questionnaire and interview data. That methodology is problematic when the subjects are preverbal and the parents being interviewed are under acute stress and may not be able to accurately report their children’s symptoms. The advantage of including many sources and types of data sensitive to the symptoms of young children is a much more complete and accurate assessment of their stress responses. This study demonstrates how young children can be effectively recruited shortly after a burn, assessed, and subsequently followed up.
Early identification of young burn victims who also have elevated heart rates and high levels of pain and who exhibit symptoms of PTSD may help prevent the development of later psychopathology. If the assessment of stress is improved, then early interventions may be designed to prevent or reduce the later emergence of posttraumatic stress, including phobias and other associated symptoms and behaviors. Some interventions are already available for older children
(40 –
42), some of which have been attempted with pilot groups of young children
(43,
44) .
As a result of this study, there are four recommendations of great importance for future stress research in early childhood. First, further study is indicated to look at the physiological indices of stress that predicted increased posttraumatic stress symptoms. These included ratings of pain and elevated heart rates. Second, further research should investigate whether decreased social smiling or decreased vocalization should be added as clinical signs of posttraumatic symptoms or, alternatively, if they reflect inhibited temperament. Third, the effects of race and ethnicity and socioeconomic status should be examined. Fourth, other populations of traumatized children, such as those who have suffered neglect or abuse, other injuries, or disasters, should be studied with these parameters.
Limitations
One limitation to this study was the number of participants who completed the assessment 1 month after the burn. Forty-four percent of the original group completed the follow-up assessment at our laboratory. Retention of follow-up assessments in this age group is difficult because some mothers raising a number of young children cannot travel to Harvard University for assessment. To increase the number of follow-ups in future studies, assessments could be conducted at the child’s home with portable equipment, or the cost of transportation might be reimbursed so that the mother and child could travel to the laboratory.
The retention of follow-up subjects may also have resulted in variability in the follow-up assessment. Although it is possible that families with children of a specific temperament were more likely to complete the follow-up, there is no evidence of this. Because of the small group of follow-up subjects, differences in developmental or behavioral outcomes with regard to age or gender are unknown.
Our results are based on young children hospitalized with burn injuries, mostly white children whose burns were of small to moderate size, but the results may apply to young children of other ethnicities or those with other injuries or trauma.
Conclusions
Preschool children admitted to a burn unit were physiologically reactive, and their PTSD symptoms were related to later developmental outcomes. Behavioral and developmental observations, social smiling, and vocalizations were found to be associated with important physiological reactivity and psychosocial functioning. Furthermore, an elevated heart rate during hospitalization was associated with decreased social smiling and decreased vocalizations at the 1-month follow-up. Behavioral and developmental observations were found to be associated with posttraumatic stress symptoms.