Postpartum major depressive disorder is a common illness with a high degree of morbidity, especially among low-income women
(1) . Several experts on this disorder have advocated for preventive interventions beginning in pregnancy
(2,
3) . In an earlier pilot study
(4), we found that an intervention based primarily on the principles of interpersonal therapy appeared to be successful in preventing the occurrence of postpartum depression within 3 months after delivery among pregnant women on public assistance with at least one risk factor for postpartum depression. To date, ours is the only study on interventions aiming to reduce postpartum depression in at-risk pregnant women that has reported empirical support for an intervention. The lack of effect in other intervention studies is difficult to interpret because of methodological limitations, such as high attrition rate, lack of a standardized intervention, and an insufficiently high risk of postpartum depression among study subjects
(5) .
The primary aim of this study was to examine whether participation in a program based primarily on interpersonal therapy could reduce the risk of postpartum depression during the first 3 months after delivery in a larger sample of pregnant women who were on public assistance and were at risk for postpartum depression. The ROSE Program (Reach Out, Stand strong, Essentials for new mothers) was designed to help mothers-to-be in an ethnically diverse population improve their close interpersonal relationships and change their expectations about them, build and use their social support networks, and master their role transition to motherhood. An emphasis on social relationships is especially relevant for low-income women who have recently delivered; research with this population suggests that social support can limit the negative effects of chronic stress
(6) and that social support is inversely associated with perinatal symptoms of depression
(7) .
Method
The study protocol and informed consent procedure were approved by the institutional ethics board of the hospital that houses the clinic where the study took place. Pregnant women at 23–32 weeks’ gestation who were on public assistance and who attended a prenatal medical clinic in Providence, R.I., were approached about participating in the study. Of 512 women approached, 442 (86%) provided informed consent and completed a 17-item risk survey developed and validated by Cooper et al. (8) as a predictive index for postpartum depression. Possible scores on the index range from 0 to 63, with higher scores indicating higher risk; women were eligible for the study if they had a score 27, the empirically derived threshold for high-risk status. Of the 201 (45%) women who met the risk criterion, those who were currently receiving mental health treatment (N=29) or who met criteria for a current depressive disorder or substance use disorder (N=3) as indicated by the Structured Clinical Interview for DSM-IV Axis I Disorders-Non-Patient Edition (9) were excluded from the study. In addition, 70 of the women who met the risk criterion were unavailable to be assessed for depression or substance use (e.g., their phone was disconnected, they did not return calls, or they relocated), which left us with a sample of 99 women, or 22% of those originally recruited for the study.
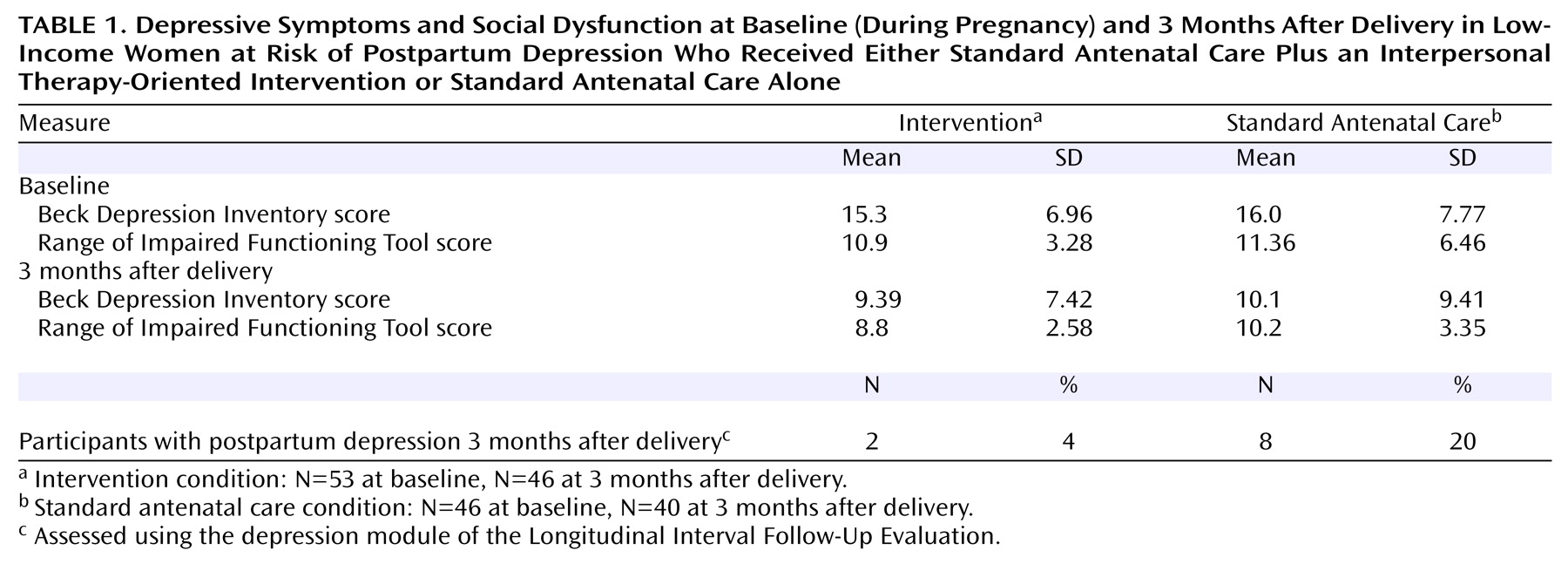
At baseline and again 3 months after delivery, depressive symptoms were assessed with the Beck Depression Inventory (BDI)
(10), and level of social adjustment was measured with the Range of Impaired Functioning Tool
(11) . To determine whether participants developed postpartum depression within 3 months after delivery, we used the depression module of the Longitudinal Interval Follow-Up Evaluation
(12), an interviewer-based assessment in which detailed information about the onset of the illness is collected.
After baseline assessments were conducted, urn randomization was performed to stratify our sample for any previous episode of depression, and then participants were randomly assigned to receive either the ROSE Program intervention in addition to standard antenatal care or standard antenatal care alone.
The intervention is made up of four 60-minute group sessions with three to five women assigned to the group over a 4-week period and a 50-minute individual booster session after delivery (the four group sessions are described in our earlier report
[4] ). The booster session aims to reinforce skills learned in the group sessions and to address any current or anticipated mood changes associated with interpersonal difficulties now that the newborn has arrived. Therapists for the study were two nurses who had received intensive training and supervision in delivery of the intervention.
Results
Of the 99 women who underwent random assignment, 66 were single, and 66 had completed high school; 44 were Hispanic, 28 Caucasian, 17 African American, two Asian, and eight “other”; this ethnic distribution was fairly representative of the prenatal clinic’s patient population. The participants’ mean age was 22.4 years (SD=4.72). The mean score on the risk index was 32.8 (SD=4.81). Thirty-one women had had previous major depressive episodes, and 23 of these had just one such episode. There were no significant differences between the two conditions on any of the demographic or clinical variables measured.
Of the five sessions of the intervention, the mean number of sessions attended was 3.3 (SD=1.97), and the mode was 5. Seven (13%) women in the intervention condition and six (13%) in the standard antenatal care condition dropped out of the study before the postpartum assessment; six of these women dropped out because they moved out of state.
Forty-six women in the intervention condition and 40 in the standard care condition were assessed 3 months after delivery. Two (4%) of those in the intervention condition and eight (20%) in the standard antenatal care condition developed postpartum depression (Fisher’s exact test, p=0.04) (
Table 1 ). A history of depression had been noted in three of these women, two of whom were in the standard care condition.
For the secondary outcome measures—depression severity and social adjustment—a multivariate analysis of covariance found no significant differences between the two conditions in scores on the BDI or the Range of Impaired Functioning Tool 3 months after delivery, controlling for baseline scores. None of the outcomes was significantly related to ethnicity.
Discussion
In a sample of financially disadvantaged women who were assessed to be at risk for postpartum depression, those assigned to receive a brief interpersonal therapy-oriented intervention in addition to standard antenatal care were significantly less likely than those receiving standard antenatal care alone to develop postpartum depression within 3 months after delivery. There were no significant differences between the two conditions in depression severity ratings or degree of social impairment 3 months after delivery. This may be because the intervention had no effect on these clinical outcome measures or because the cross-sectional measurements were not sensitive to changes within the 3-month time frame.
These findings, along with the preliminary findings we reported previously
(4) on use of this intervention with a similar group of pregnant women at risk of postpartum depression, provide additional evidence supporting efficacy for the intervention. Additional research is needed to determine whether using additional sessions farther into the postpartum period would improve outcomes and whether the intervention is applicable in other settings.