The neurotransmitter γ-aminobutyric acid (GABA) exerts a prominent effect on central adrenergic stress responses in times of severe stress
(1), and low levels have been associated with alcohol addiction, depression, and sleep problems, all of which are also seen in individuals with posttraumatic stress disorder (PTSD)
(2) . We previously showed
(3) that road traffic accident victims with low plasma GABA levels on arrival at the hospital were more likely than those with normal GABA levels to have developed acute PTSD when assessed 6 weeks later. Patients from the same cohort were included in a 1-year follow-up study to test the hypothesis that there is a link between low posttrauma plasma GABA levels and long-term PTSD.
Method
Subjects
Study subjects were road traffic accident victims who were consecutively admitted to a trauma department and were hospitalized at least 3 days. The same analgesics and anesthetic protocols were used with all patients. To ensure the validity of GABA measurements, exclusion criteria included a history of alcohol abuse, alcohol use at the time of the accident, and use of a benzodiazepine or an anticonvulsant. The study was approved by the hospital ethics committee. After the study protocol had been fully explained, patients gave written informed consent to participate.
Procedure
The day after admission to the trauma department, two 10 ml blood samples were drawn. Plasma GABA levels were measured by mass spectrometry, using an ion-trap technique with isotopic dilution
(3) . Six weeks and again 1 year after the accident, participants were contacted by a trained psychologist who administered a modified version of the Clinician-Administered PTSD Scale
(4) over the telephone. At the 1-year follow-up, the mood disorders section of the Mini International Neuropsychiatric Interview was also administered
(5) .
Statistical Analyses
Analyses were performed with SAS, version 8.0 (SAS Institute, Cary, N.C.). The Shapiro-Wilk test of normality, applied to the natural logarithm of GABA plasma levels, assessed the log-normality of this parameter. Various nonparametric tests were used for comparisons, depending on group sizes. After conducting bivariate analyses, we proceeded with multivariate tests using independent variables that approached significance (p<0.15 and N>10) in a multivariate logistic regression analysis, with alpha set at 0.05 (two-sided tests).
Participants were considered to have PTSD if they met DSM-IV criteria for diagnosis, and partial PTSD if they met all criteria except an item from criterion C or D. In the analyses, cases of PTSD and partial PTSD were both counted as PTSD. No difference in mean GABA levels was observed between these groups at any time point. Participants were categorized into four outcome groups. Those who met criteria at both the 6-week and 1-year follow-up assessments were categorized as having chronic PTSD; those who met criteria at the 6-week follow-up but not at the 1-year follow-up were categorized as having remitting PTSD; those did not meet criteria at the 6-week follow-up but did at the 1-year follow-up were categorized as having delayed-onset PTSD; and those who did not meet criteria at either follow-up assessment were categorized as never having had PTSD.
Results
Of 157 road traffic accident victims consecutively hospitalized, 86 met DSM-IV criteria A1 and A2 for PTSD as well as the other criteria for inclusion in the study. Of these, 78 (91%) completed the 1-year assessment. The subjects lost to follow-up were more often men (Fisher’s exact test, p=0.001), and their initial PTSD symptoms tended to be lower (Clinician-Administered PTSD Scale score, mean=25.3, SD=11, compared with mean=39.2, SD=13, p=0.003).
Patient Characteristics
Participants ranged in age from 18 to 74 years (mean=31.3, SD=13.1). The mean revised Injury Severity Score
(6), in which possible scores range from 0 to 5, was fairly high at 2.86 (SD=0.7). The mean length of hospital stay was 57 days (median=32), and the mean duration of rehabilitation was 6.8 months (median=2.7). As expected, Injury Severity Score and length of stay were not correlated with GABA levels, PTSD, or depression.
At the 6-week assessment, 44 participants (56%) met criteria for PTSD or partial PTSD. At the 1-year assessment, 22 participants met criteria; of these, 15 met criteria at the 6-week assessment as well (categorized as having chronic PTSD) and seven did not (delayed-onset PTSD). Of the 56 who did not meet criteria at the 1-year assessment, 29 met criteria at the 6-week assessment (remitted PTSD) and 27 did not (never had PTSD).
During the study, 38 participants were taking medication at least part of the time, mostly anxiolytics (benzodiazepines, hydroxyzine, and the like). There was no statistical difference in age, sex, or diagnosis of PTSD or major depressive disorder between those who were taking medications and those who were not.
Posttrauma Plasma GABA Levels
The mean posttrauma GABA level was significantly lower among subjects who met criteria for PTSD or partial PTSD 6 weeks after trauma exposure (mean=0.20 mmol/ml, SD=0.08) than among those who did not (mean=0.26 mmol/ml, SD=0.09; z=3.10, df=78, p=0.002).
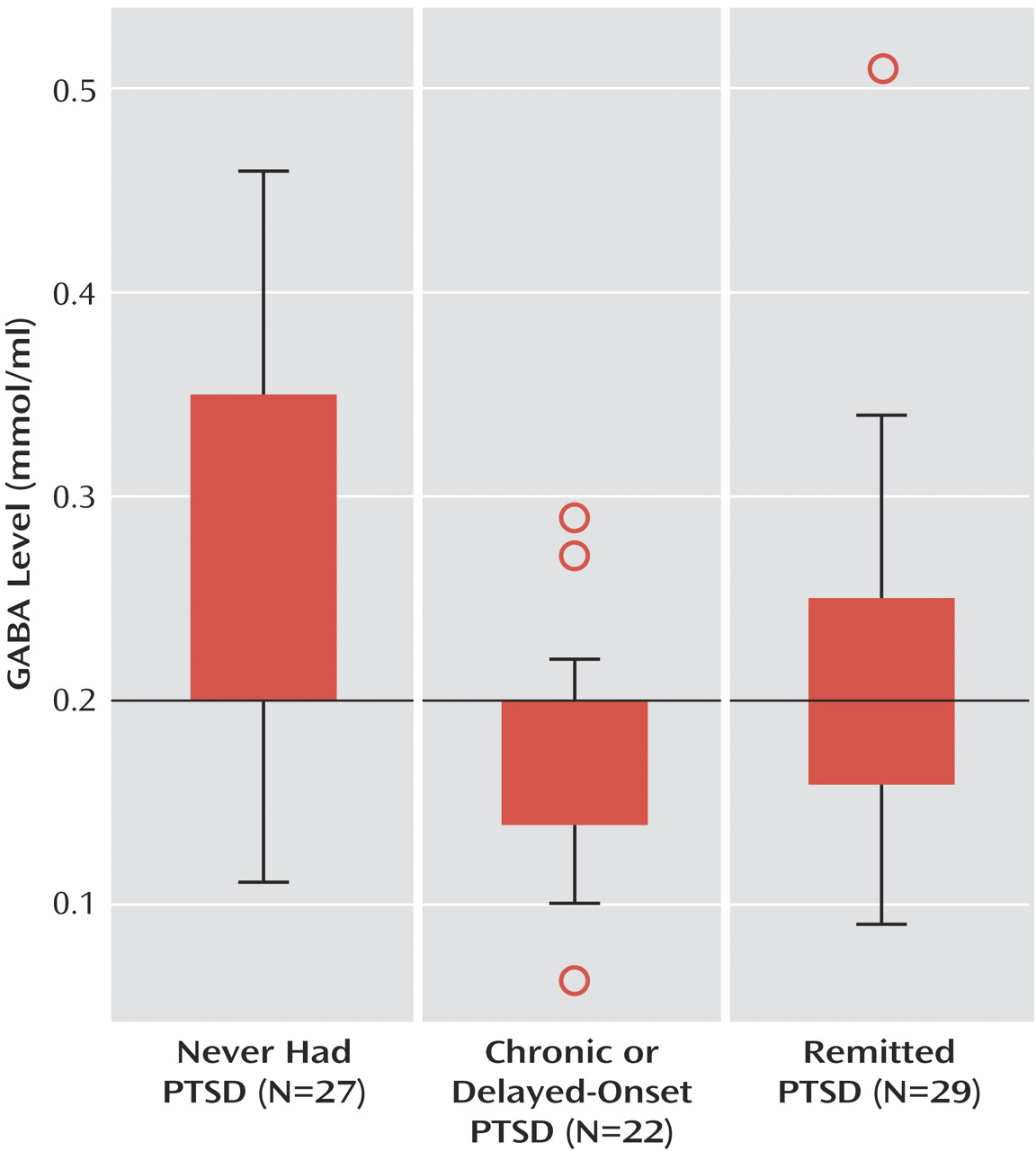
For the four outcome groups, the mean posttrauma GABA levels were as follows: the chronic PTSD group, 0.18 mmol/ml (SD=0.05); the delayed-onset PTSD group, 0.15 mmol/ml (SD=0.05); the remitted PTSD group, 0.21 mmol/ml (SD=0.08); and the never had PTSD group, 0.28 mmol/ml (SD=0.09) (see
Figure 1 ). Posttrauma GABA levels were significantly lower among participants who met all or nearly all criteria for PTSD at the 1-year follow-up (the chronic and delayed-onset PTSD groups) than among those who did not (the remitted PTSD group and the never had PTSD group) (z=–3.13, df=78, p=0.0018). Moreover, a statistically significant difference was noted between the remitted PTSD and chronic PTSD groups (z=2.9, df=44, p=0.004).
Among subjects whose posttrauma GABA level was less than 0.20 mmol/ml and who did not meet full or partial criteria for PTSD 6 weeks after their accident, 80% met criteria at the 1-year follow-up (delayed-onset PTSD, N=7). By contrast, among those whose GABA levels exceeded 0.20 mmol/ml and who met criteria at 6 weeks, 75% no longer did so at 1 year (remitted PTSD, N=29). No correlation was observed between GABA level and age or sex.
The multivariate logistic regression analyses yielded only two statistically significant factors linked to the presence of PTSD at the 1-year follow-up: posttrauma GABA level below 0.20 mmol/ml (odds ratio=16.4, 95% confidence interval [CI]=4.1–65.9, p<0.0001), and PTSD at 6 weeks (odds ratio=8.2, 95% CI=1.5–44.7, p=0.016).
Relationship Between PTSD and Major Depression at 1 Year
The mean posttrauma GABA level among participants who were found at the 1-year follow-up to be suffering from major depressive disorder (mean=0.20, SD=0.07) was lower than the level among those who were not (mean=0.24, SD=0.09; z=–1.93, df=73, p=0.053). A statistically significant relationship was observed between the development of full or partial PTSD and major depressive disorder during the 1 year of follow-up (χ 2 =8.5, df=1, p=0.0036). The two disorders were often found to be comorbid at the 1-year assessment, with 15 of the 22 patients (68%) who met all or nearly all criteria for PTSD also meeting criteria for major depressive disorder.
Discussion
In this study, most of the patients whose posttrauma GABA level was below 0.20 mmol/ml were found to have chronic, delayed-onset, or partial PTSD at follow-up 1 year after their accident.
In a given individual, plasma GABA levels seem to be stable over time; they are probably genetically controlled through autosomal recessive transmission
(2) . In individuals with genetically low GABA reserves, regulation of the hyperadrenergic response may be rapidly overloaded. According to Nutt’s hypothesis
(7), this may enhance emotional memory encoding.
One limitation of this study is that it remains unclear whether serum GABA truly reflects brain GABA activity. Another limitation is that the generalizability of the findings is weakened by the exclusion of patients who had a history of alcohol abuse or were under the influence of alcohol at the time of the accident (N=36).
Spontaneous recovery from PTSD often occurs during the year following the precipitating trauma; among our study subjects, 35%–40% had PTSD at 6 weeks, and only 15%–20% did at 1 year. From a clinical perspective, it would be extremely helpful to predict with reasonable accuracy which trauma patients are at risk of having chronic PTSD. Our results, if replicated, would suggest that a plasma GABA level greater than 0.20 mmol/ml may protect against chronic PTSD and may represent a marker of recovery among patients who have suffered trauma.