Anorexia nervosa differs from most psychiatric disorders because of its ego-syntonic nature, which leads to treatment refusal and poor insight. Weight restoration opposes patients’ pervasive drive to diet, making treatment inherently paternalistic. Ambivalence toward treatment has been labeled part of anorexia nervosa’s core psychopathology
(1), and the clinician’s ethical challenge is to treat patients effectively while respecting their autonomy
(2,
3) . Discrepancy between patient and provider goals results in a conflict of wills, typical of behavioral disorders
(4) and evident in the earliest historical accounts of treatment: as Gull reported of a patient in 1874, “every step of the way had to be fought; she was most loquacious and obstinate”
(5) . Although bulimia nervosa is less ego-syntonic, it has in common with anorexia nervosa a compelling drive to engage in unhealthy dieting behavior and fear of weight gain.
Most experts agree that, with the exception of outpatient family therapy as a first-line treatment for adolescents whose duration of illness has been brief
(6,
7), severe anorexia nervosa often requires refeeding during a stay on an inpatient behavioral specialty unit
(8) . In most of such admissions, some degree of coercive pressure, whether subtle or direct, has been applied by clinicians, family, friends, employers, or educators, including persuasion, bargaining, begging, enticing, and threatening involuntary commitment
(9) . To be effective, the treating team must win patients’ cooperation over time and persuade them to change their behavior.
Involuntary admission for anorexia nervosa, which lies at one end of the spectrum of coercive treatment, remains controversial and is used rarely, by few treatment centers, and only in life-threatening cases
(10,
11) . Although long-term prospective outcome studies are lacking, involuntary treatment has been shown to result in equivalent weight gain compared with voluntary hospitalization for eating disorders
(12 –
14) . Moreover, in a study of 64 inpatients admitted involuntarily for treatment of eating disorders, none complained formally or informally about being committed against their will
(14) .
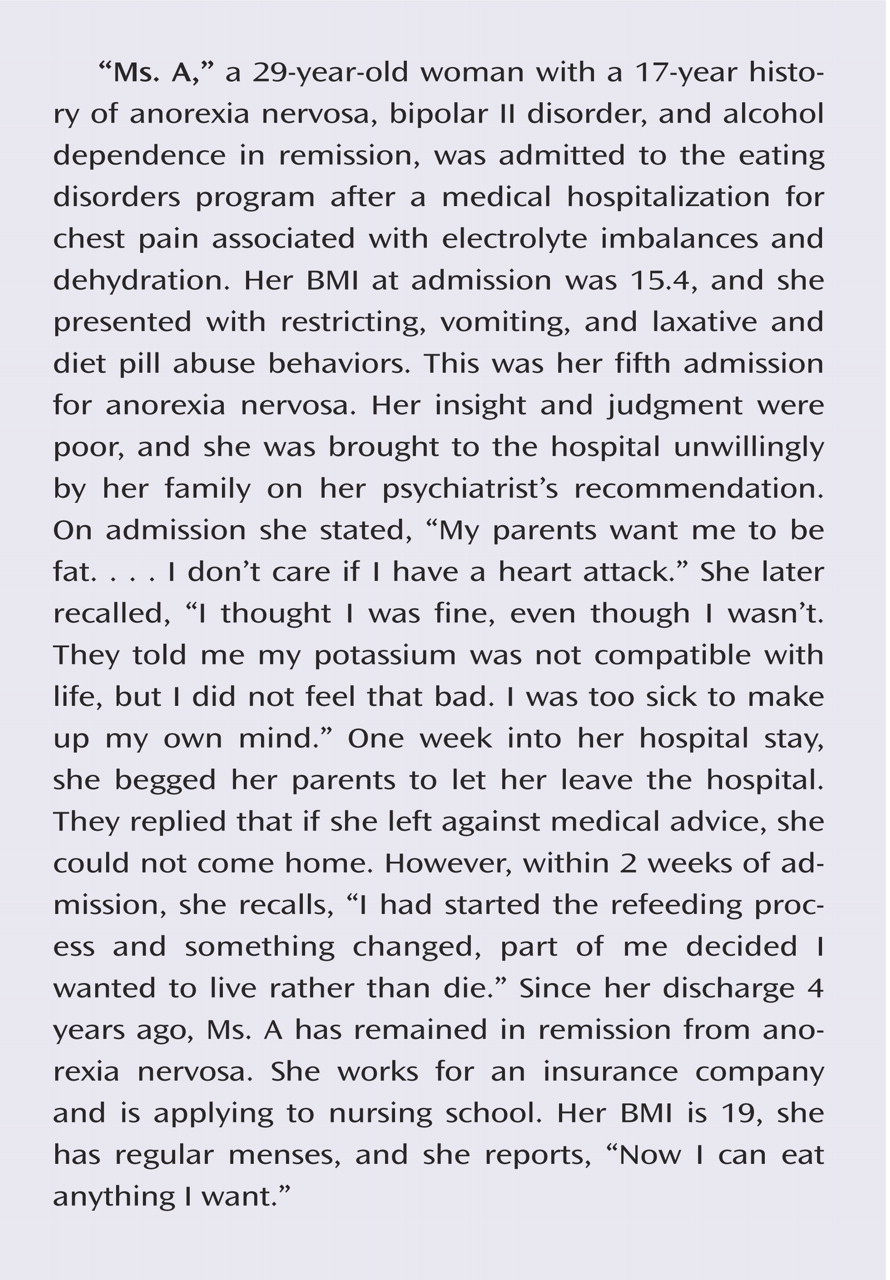
There are two views on the potential effectiveness of pressuring eating disorder patients into hospital admission. One view is that coerced treatment is ineffective because it alienates patients and makes them noncompliant or superficially compliant in order to “eat their way out” of the hospital
(15) . The opposing argument is that patients’ judgment and choices are impaired by their disorder, rendering their actions substantially unfree or involuntary, and that their views often change after they have received care
(1,
14,
16) . The psychiatric literature suggests that although most involuntarily admitted general psychiatry patients do not express gratitude for being admitted against their will, they do retroactively judge being compulsorily detained as justified and agree that it helped them
(17,
18) .
The perceptions of eating disorder patients about being coerced into admission have received little attention in the literature. However, the MacArthur Foundation’s Research Network on Mental Health and the Law developed a method and instruments to measure perceived coercion in other psychiatric populations
(17,
19,
20) . Gardner and colleagues
(17) administered the MacArthur Admission Experience Interview to 267 involuntary and voluntary general psychiatric patients at admission and again 4–8 weeks after discharge. Perceptions of procedural justice—that is, how fair patients felt the admission process was—and perceived coercion—how much they felt forced, pushed, or intimidated into treatment—were stable over time. Patients who did not believe that they needed hospitalization reported more perceived coercion, felt greater pressure by others to be admitted, and complained of being treated with less procedural justice. At follow-up, however, 52% of this group had converted to believing that they did need hospitalization at the time of admission. Furthermore, several subsequent studies found no relationship between perceived coercion at admission and later adherence to treatment
(21,
22) .
In the present study, we examined perceptions among eating disorder patients about their need for hospitalization and the coerciveness of the admission process, and we assessed whether their beliefs about their need for admission changed or remained stable in the short term. We hypothesized that patients under age 18 would score higher than adults on measures of perceived coercion and lower on perceived need for admission, since most are admitted by their parents, often against their will. Because patients with anorexia nervosa have greater ambivalence toward treatment, and because of the ego-syntonicity of the disorder, we expected patients with anorexia to report more perceived coercion and less need for hospitalization than patients with bulimia. We also predicted that a significant proportion of patients who reported at admission that they did not need hospitalization would change their minds within 2 weeks and agree that their admission was justified.
Method
Participants
The study was approved by a Johns Hopkins Medicine institutional review board, and data were collected as part of a larger longitudinal study on the efficacy of inpatient treatment for eating disorders. Patients were given a complete description of the study, and written informed consent was obtained; those under age 18 provided verbal assent, and written informed consent was obtained from a parent or guardian.
Participants were recruited from all admissions to a behavioral inpatient and partial hospital program for eating disorders between January 2000 and February 2003. All adults were voluntary admissions. Adolescent patients were admitted by a parent. For patients admitted more than once within the study period, only data from the initial admission were analyzed. Of 299 potential participants, 139 completed a self-report scale derived from the MacArthur Admission Experience Interview (described below) at admission and again 2 weeks into their hospital stay. Another 74 patients completed the self-report scale at only one time point and were excluded from analyses. On average, these patients had a greater body mass index (BMI) at admission than study participants (mean=20.6 [SD=6.2] versus mean=18.7 [SD=4.6]; F=6.36, df=1, 207, p=0.012) and a shorter length of inpatient stay (mean=12.5 [SD=9.4] versus mean=22.0 [SD=18.8]; F=16.40, df=1, 207, p<0.001); the two groups did not differ in age, years of self-reported dieting, eating disorder diagnosis, eating disorder symptoms as measured by the Eating Disorder Inventory–2
(23) (subscales for bulimia, drive for thinness, body dissatisfaction), subscales of the admission experience self-report scale we used, or perceived need for hospitalization. Another 86 patients either refused to participate (N=44) in the longitudinal outcome research study or consented but did not complete self-report measures (N=42). On average, these patients had a shorter inpatient stay than participants (mean=16.1 [SD=15.9] versus mean=22.0 [SD=18.8]; F=5.83, df=1, 220, p=0.017) but did not differ significantly by age, BMI at admission, or eating disorder diagnosis.
Of the 139 patients included in the study, 136 (98%) were female and 128 (92%) were Caucasian. The participants’ mean age was 25.2 years (SD=10.1), and 25% (N=35) were under 18 years of age.
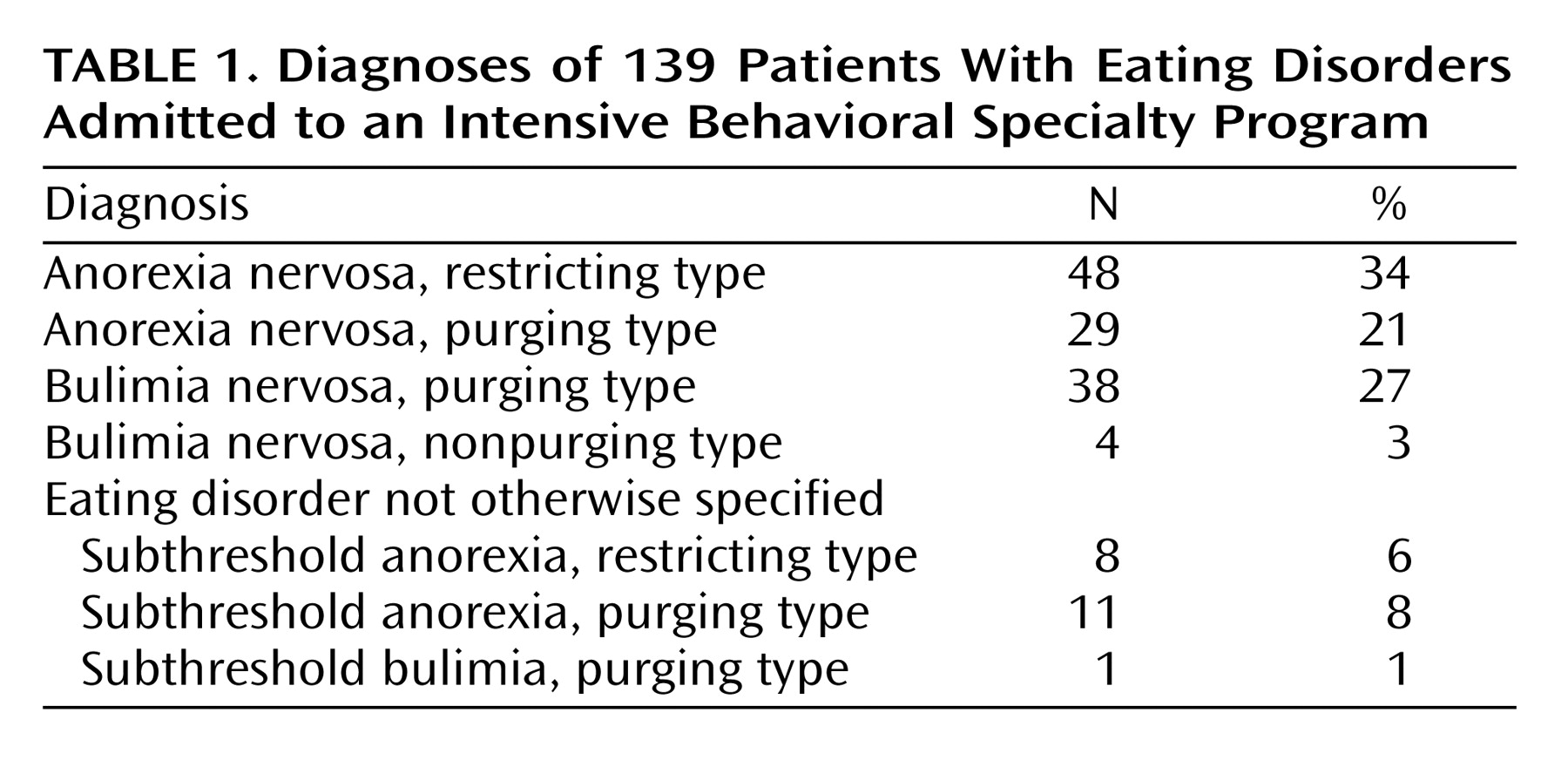
Table 1 presents the diagnostic breakdown of the sample; 55% of participants had a diagnosis of anorexia nervosa, 30% bulimia nervosa, and the remaining 15% received subthreshold eating disorder diagnoses (eating disorder not otherwise specified). Patients with binge eating disorder were excluded.
Participants were classified in two ways for comparisons across diagnostic subgroups: 1) broadly defined anorexia nervosa (which included the restricting and purging types as well as diagnoses of eating disorder not otherwise specified with subthreshold anorexia of both types) compared with broadly defined bulimia nervosa (which included the purging and nonpurging types as well as eating disorder not otherwise specified with subthreshold bulimia); and 2) broadly defined anorexia nervosa, restricting type (that is, diagnoses and subthreshold cases) compared with broadly defined anorexia nervosa, purging type (diagnoses and subthreshold cases). The eating disorder not otherwise specified cases were included because recent data suggest that, in anorexia, they are clinically indistinguishable from those that meet full DSM-IV criteria in terms of severity, functional impairment, and short-term treatment outcome
(24) . Moreover, all of these cases were severe enough to warrant inpatient treatment. Participants were also classified as minors (12–17 years of age) versus adults (≥18 years of age) for age comparison analyses.
Measures
Basic demographic information was collected for each participant, including age, gender, race, and years of dieting history. Eating disorder diagnoses were made by trained clinicians using the eating disorders module of the Structured Clinical Interview for DSM-IV
(25) . For patients who refused to participate in the study, diagnoses were made by retrospective chart review by an experienced clinician using DSM-IV criteria. Clinical indices, including admission and discharge BMI and length of hospital stay, were obtained from participants’ hospital charts.
The self-report scale we used is a 13-item questionnaire derived from the MacArthur Admission Experience Interview
(17,
20), a 30-minute structured interview assessing patients’ perceptions of the hospital admission process on three subscales: perceived coercion regarding the decision to be admitted, pressure to be hospitalized placed on the patient by others, and procedural justice, reflecting the patient’s assessment of how he or she was treated during the admission process. The MacArthur Admission Experience Interview also includes a question addressing belief in need for hospitalization. The self-report scale incorporates items in the MacArthur Admission Experience Interview to create three four-item subscales. These 12 items are scored on a 5-point scale from 1 to 5 and summed within each subscale for a total subscale score. Higher scores indicate more perceived coercion, more pressure, and greater sense of procedural justice. The final item assesses the patient’s perceived need for hospitalization (“Do you believe that you need to be in the hospital?”); it is scored on a 5-point scale from 1 (definitely no) to 5 (definitely yes).
The internal consistency reliability of the self-report scale in this sample was good, with Cronbach alpha coefficients for perceived coercion, pressure, and procedural justice estimated at 0.91, 0.65, and 0.82, respectively.
Procedure
Of the 139 study participants, 98% (N=136) were initially admitted to the inpatient unit and then transitioned to partial hospitalization; 2% (N=3) were admitted directly to partial hospitalization. Each participant completed the admission experience self-report scale at admission and again 2 weeks later. BMI at admission and at discharge and length of hospital stay were recorded. The treatment team determined step-down to partial hospitalization on the basis of the patient’s progress in blocking eating disordered behaviors, normalizing food choices, and rate of weight gain if underweight. Treatment was behaviorally based, with a focus on intensive group therapy utilizing principles of both cognitive behavior therapy and dialectical behavior therapy
(26) . Family therapy and parent training were important components of treatment for adolescent patients.
Data Analysis
SPSS version 13.0 (SPSS, Chicago) was used for data analysis. All tests of significance were based on an alpha set at 0.05, two-tailed. Group differences on continuous and categorical variables were evaluated using univariate analyses of variance (ANOVAs) and chi-square tests, respectively. Multivariate analyses of variance (MANOVAs), followed by univariate tests, were used to assess differences in self-report subscale scores across groups. Repeated-measures ANOVAs were used to evaluate differences in self-report subscale scores over time. Specific data analytic strategies are discussed below prior to reporting each finding.
Results
Perceived Coercion, Pressure, and Procedural Justice Across Diagnoses and Age
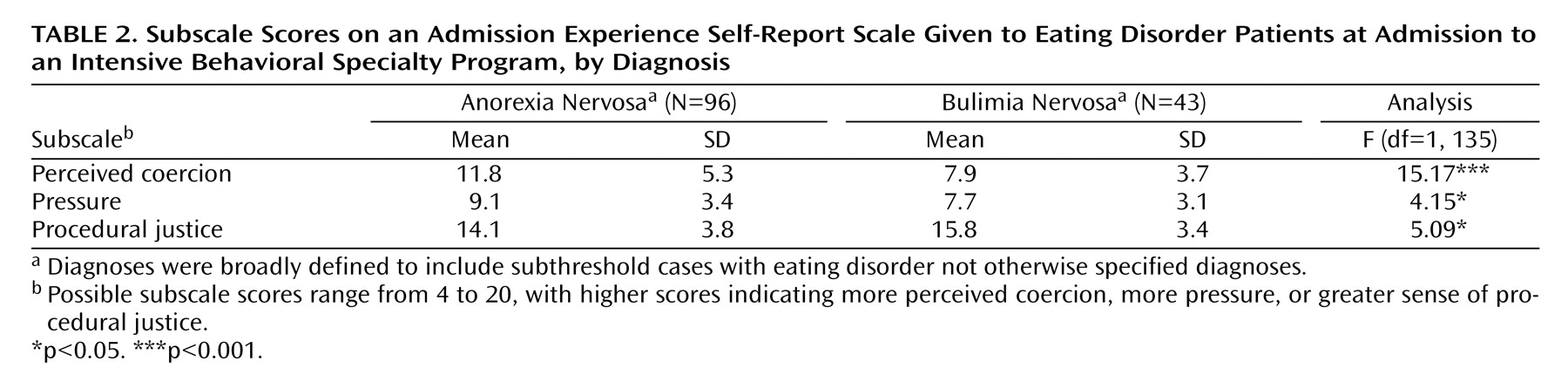
A factorial MANOVA was conducted to evaluate differences in subscale scores on the admission experience self-report scale across diagnostic categories and age at admission. Diagnosis (broadly defined anorexia versus bulimia) and age (minor versus adult) were included as independent variables, and the three subscales (perceived coercion, pressure, and procedural justice) were entered as dependent variables. Results yielded a multivariate main effect for diagnosis (F=5.62, df=3, 133, p=0.001) and for age (F=9.82, df=3, 133, p<0.001) but no significant interaction. Univariate tests of main effects for diagnosis revealed that anorexia patients reported more perceived coercion and pressure and less procedural justice than bulimia patients (
Table 2 ). Univariate tests of main effects for age revealed a significant finding only for perceived coercion, with minors (mean=14.2, SD=4.8) reporting greater feelings of coercion compared with adults (mean=9.4, SD=4.7; F=15.29, df=1, 135, p<0.001). In order to discern differences between broadly defined anorexia subgroups, a second MANOVA was conducted using anorexia subtype (restricting versus purging) and age (minor versus adult) as independent variables and subscale scores as dependent variables. Results showed a significant multivariate main effect only for age (F=8.23, df=3, 90, p<0.001) and no significant interaction. Univariate tests revealed that among anorexia patients, minors reported more perceived coercion than adults (mean=15.3, SD=4.3, versus mean=10.4, SD=5.0; F=16.19, df=1, 92, p<0.001). No significant differences between minors and adults were found on pressure or procedural justice scores.
Perceived Coercion, Pressure, and Procedural Justice at Admission in Relation to Belief in Need for Hospitalization
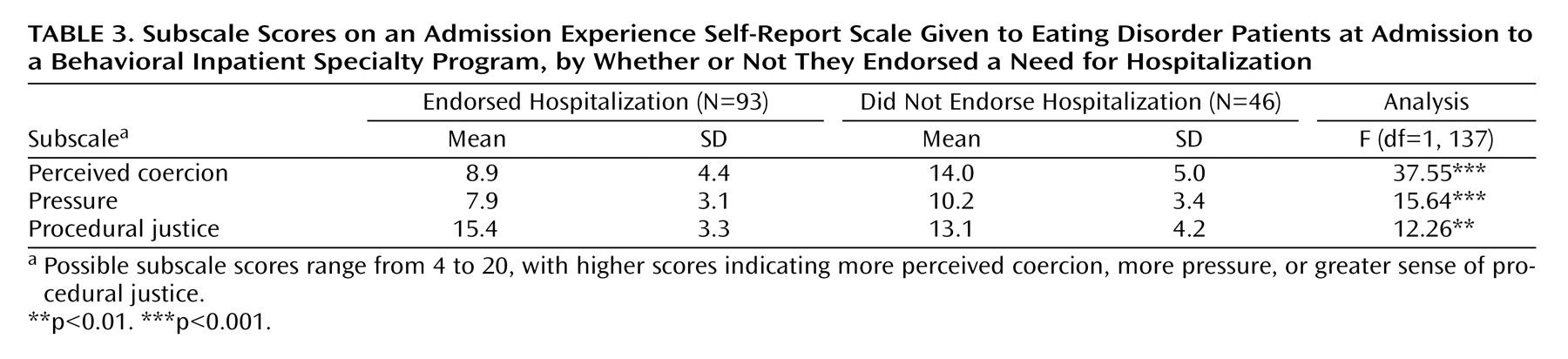
A one-way MANOVA was conducted to evaluate potential differences in the three subscale scores between patients who endorsed a need for hospitalization at admission and those who did not. Scores on item 13 on the admission experience self-report scale (“Do you believe that you need to be in the hospital?”) were dichotomized such that scores of 3 and below (anchors were definitely no=1 and definitely yes=5) were classified as not endorsing a need for hospitalization and scores of 4 and 5 were classified as endorsing a need for hospitalization. The MANOVA yielded a significant multivariate effect (F=12.68, df=3, 135, p<0.001) with differences on all three subscales. Patients who believed they needed hospitalization reported less perceived coercion and pressure and greater procedural justice compared with those who did not think they needed hospitalization.
Table 3 presents the means and univariate statistics for this analysis.
Belief in Need for Hospitalization
Differences by Diagnosis at Admission
Patients’ belief in need for hospitalization (did not endorse versus endorsed) by diagnostic category (broadly defined anorexia versus bulimia) was evaluated using a 2×2 chi-square analysis. While proportionally more anorexia patients (34 of 96, or 35%) than bulimia patients (12 of 43, or 28%) did not endorse the need for hospitalization when assessed at admission to treatment, this finding was not significant. A chi-square analysis performed on data for anorexia subtypes (restricting versus purging) revealed no significant differences between groups on perceived need for hospitalization at admission.
Differences by Age at Admission
A chi-square analysis performed on data for minors and adults revealed that more minors (16 of 35, or 46%) than adults (30 of 104, or 29%) did not endorse need for hospitalization at admission, although this result did not reach statistical significance (χ 2 =3.36, df=1, p=0.067).
Changes in Belief in Need for Hospitalization After 2 Weeks
Of the 139 study participants, 46 (33%) did not endorse need for hospitalization at admission. Of these, 20 (43%) converted to believing that they did need to be hospitalized 2 weeks later. The majority of participants who converted were adults (N=17, 85%) rather than minors (N=3, 15%) (χ 2 =6.10, df=1, p=0.013). There were no significant differences in conversion status across diagnostic categories. At the 2-week follow-up, 41% (14 of 34) of anorexia patients and 50% (6 of 12) of bulimia patients who did not endorse need for hospitalization at admission converted to believing that they did need to be hospitalized. A repeated-measures ANOVA revealed a main effect of time, with patients endorsing the need for hospitalization more strongly 2 weeks after admission than at admission (score on self-report scale item 13, mean=4.1 [SD=1.1] versus mean=3.9 [SD=1.2]; F=7.35, df=1, 138, p=0.008). Additional repeated-measures ANOVAs conducted on subscales of the admission experience self-report scale demonstrated no differences between admission and follow-up on perceived coercion, pressure, or procedural justice.
Discussion
Anorexia nervosa and bulimia nervosa are characterized by a driven preoccupation with dieting and an overvalued fear of fatness
(8) . As a result, treatment aimed at interrupting dieting behaviors or increasing weight is usually met with ambivalence or frank resistance by patients. As with substance abuse, patients most often agree to enter treatment voluntarily, but only in a setting of significant coercive pressure from others.
In findings consistent with previous results in a general psychiatric population
(17), perceived need for admission was associated with less perceived coercion and pressure and with a greater sense of procedural justice. Perceived coercion was greater in adolescents than in adults, which is consistent with reports in the alcohol treatment literature of more coercive ultimatums issued to younger patients
(27) .
Being underweight, rather than the presence of purging behavior, may explain the higher perceived coercion, greater pressure by others to be admitted, and lower sense of procedural justice reported by patients with anorexia nervosa compared with those with bulimia, since no differences were found between anorexia subtypes (purging versus restricting). The lack of a diagnostic difference in perceived need for hospitalization at admission between patients with anorexia nervosa and those with bulimia may have been due to our limited sample size. Future studies using larger samples should clarify this issue.
Perceptions of coercion, pressure, and procedural justice were stable between admission and follow-up 2 weeks into treatment; however, perceived need for admission was not. Within 2 weeks of admission, nearly half of eating disorder patients who initially did not think they needed hospitalization converted to believing that they did need to be admitted. This proportion is similar to that reported by Gardner et al.
(17) in a general psychiatric population 4 to 8 weeks after discharge. Early conversion may reflect engagement in treatment, which may result from multiple factors, including the therapeutic milieu, peer influence, an increased sense of mastery accompanying behavioral change, and cognitive changes associated with reversal of the starved state. We hypothesize that the likelihood of conversion increases with time in hospital and predict that it would be even higher at discharge and postdischarge follow-up.
The large majority of those who converted were adults, which is surprising because adolescents with anorexia nervosa are generally believed to be easier to treat
(28) . Since family therapy is the most effective treatment for adolescent anorexia nervosa, parental involvement may be prognostically more important than conversion status in adolescent cases.
The high conversion rate in eating disorder inpatients who initially did not believe they needed hospitalization raises questions regarding the ethics of coercive pressure for treatment. Such pressure can be seen as an infringement of patients’ civil liberties. On the other hand, since anorexia nervosa is characterized by impaired judgment and treatment resistance and is associated with high morbidity and mortality
(29), pressure for admission may be justified under the medical principle of beneficence. The literature on substance abuse, another driven behavioral disorder that has many parallels with anorexia nervosa, suggests that coercion is often necessary to engage patients and that the outcome of coercive treatment is equivalent to, or superior to, that of self-referred treatment
(30) .
We conclude that although the issue is controversial, there is a role for coercive pressure in the treatment of eating disorders. Methods for increasing motivation to change
(31) are useful but may be insufficient to engage those patients with anorexia nervosa whose judgment is severely impaired by their disorder. In treatment-resistant cases, parent counseling may help family members set limits on their child’s self-destructive behavior by legitimizing interventions that parents might perceive as harsh, such as limiting financial support of college tuition to a child who is refusing treatment, involving school officials, or blocking eating disordered behavior in the home (e.g., by removing an exercise machine). Care must be taken, however, to avoid an arrogant approach and assume that all patients should be treated equally. Efforts must be made to maintain a positive therapeutic stance at all times. Coercive pressure is justified only by the likelihood that treatment will be beneficial. This likelihood should be assessed on a case-by-case basis; it may be higher for a chronically ill patient who has constantly evaded treatment than for the “professional patient” with whom numerous admissions, treatment modalities, and attempts at refeeding have failed.
There are several limitations of this study. First, it is a naturalistic study, and complete data are available for only 139 of 299 admissions. Design limitations and the constraints of real-world practice, including federal privacy regulations, limit the ability to conduct such a study with high participation rates. Although participants and nonparticipants did not differ in diagnosis, age, or BMI at admission, we cannot exclude the possibility that nonparticipants were a less compliant or more coerced group, which may have contributed to their shorter mean length of stay. Financial incentives for study participation might improve participation rates, although they would also introduce other potential biases. Second, patients completed the study measures while in treatment and may have been influenced by a concern that their responses could affect their discharge or by a desire to please the treatment team. Third, with follow-up questionnaires administered 2 weeks into treatment, subjects were assessed at varying BMIs rather than after discharge or on weight restoration. Fourth, all adults were voluntary admissions; results would likely differ with an involuntary sample. Finally, the study relied solely on self-reported patient perceptions, and we do not know how these reflect the objective events surrounding admission. What one individual perceives as coercive pressure may not be experienced in the same way by another.
To our knowledge, this is the first study to examine perceived coercion at admission to inpatient treatment for anorexia nervosa and bulimia. The results indicate that additional research in this area should be encouraged. Future studies should examine the stability of conversion status after discharge and the relationship between perceived coercion and long-term outcome. Attention to the relationship between objective measures of coercion and perceived coercion is also warranted.