Studies of community-based
(1) and clinical
(2) populations consistently show high rates of substance use disorders among those with bipolar disorder. Bipolar disorder patients with substance use disorder are at greater risk for medication nonadherence
(3) and suicidality
(4), recover more slowly from mood episodes
(5), and are hospitalized more often
(2) .
Despite the frequent comorbidity and poor prognostic implications, little research has focused on treatments designed specifically for this population, and most have studied pharmacotherapy
(6 –
8) . Indeed, we know of no comparative trials of psychotherapy for this population. Although recent bipolar disorder psychotherapy studies have generated promising results
(9 –
12), these trials have not focused specifically on patients with co-occurring substance use disorders. Moreover, the two largest recent substance use disorder psychotherapy trials
(13,
14) excluded patients with bipolar disorder. Thus, while integrated psychosocial treatment has been advocated for patients with substance use disorder and psychiatric illness
(15), treatment that simultaneously addresses bipolar disorder and substance use disorder has not previously been studied.
We have developed a new, manual-based therapy, “integrated group therapy,” for patients with substance use disorder and bipolar disorder
(16) . Integrated group therapy emphasizes the relationship between the disorders, focusing on similarities in thought and behavior patterns involved in recovery from bipolar disorder and substance use disorder. In our pilot study
(16), patients receiving integrated group therapy had significantly fewer days of drug use than those not receiving integrated group therapy. However, it was unclear whether integrated group therapy patients fared better because of integrated group therapy-specific content or whether they benefited from sharing experiences with similar patients. Moreover, patients were not randomly assigned in the pilot study. Rather, we recruited cohorts of patients consecutively for integrated group therapy or for monthly assessments; all patients also received treatment-as-usual.
We therefore undertook a randomized controlled study to compare the efficacy of integrated group therapy with an active treatment, group drug counseling
(17), designed to approximate the treatment patients might receive in a substance abuse treatment program. Unlike integrated group therapy, which addresses bipolar disorder and substance use disorder simultaneously, group drug counseling concentrates primarily on substance use. We hypothesized that integrated group therapy patients would have better substance use and mood outcomes than group drug counseling patients.
Method
Procedures
Patients with current bipolar disorder and substance dependence were recruited from McLean Hospital programs, advertisements, fliers, and clinician referrals. The protocol was approved by the McLean Hospital Institutional Review Board. Written informed consent was obtained after study procedures were fully explained. Inclusion criteria were 1) current diagnoses of bipolar disorder and substance dependence other than nicotine, per the Structured Clinical Interview for DSM–IV
(18) ; 2) substance use within 60 days; 3) a mood stabilizer regimen for ≥2 weeks; and 4) age ≥18. Exclusion criteria were 1) current psychosis, 2) current danger to self or others, 3) concurrent group treatment, or 4) residential treatment restricting substance use. Individual therapy was permitted; most patients in our integrated group therapy pilot study attended individual psychotherapy
(19) . Excluding them would have created an unrepresentative cohort.
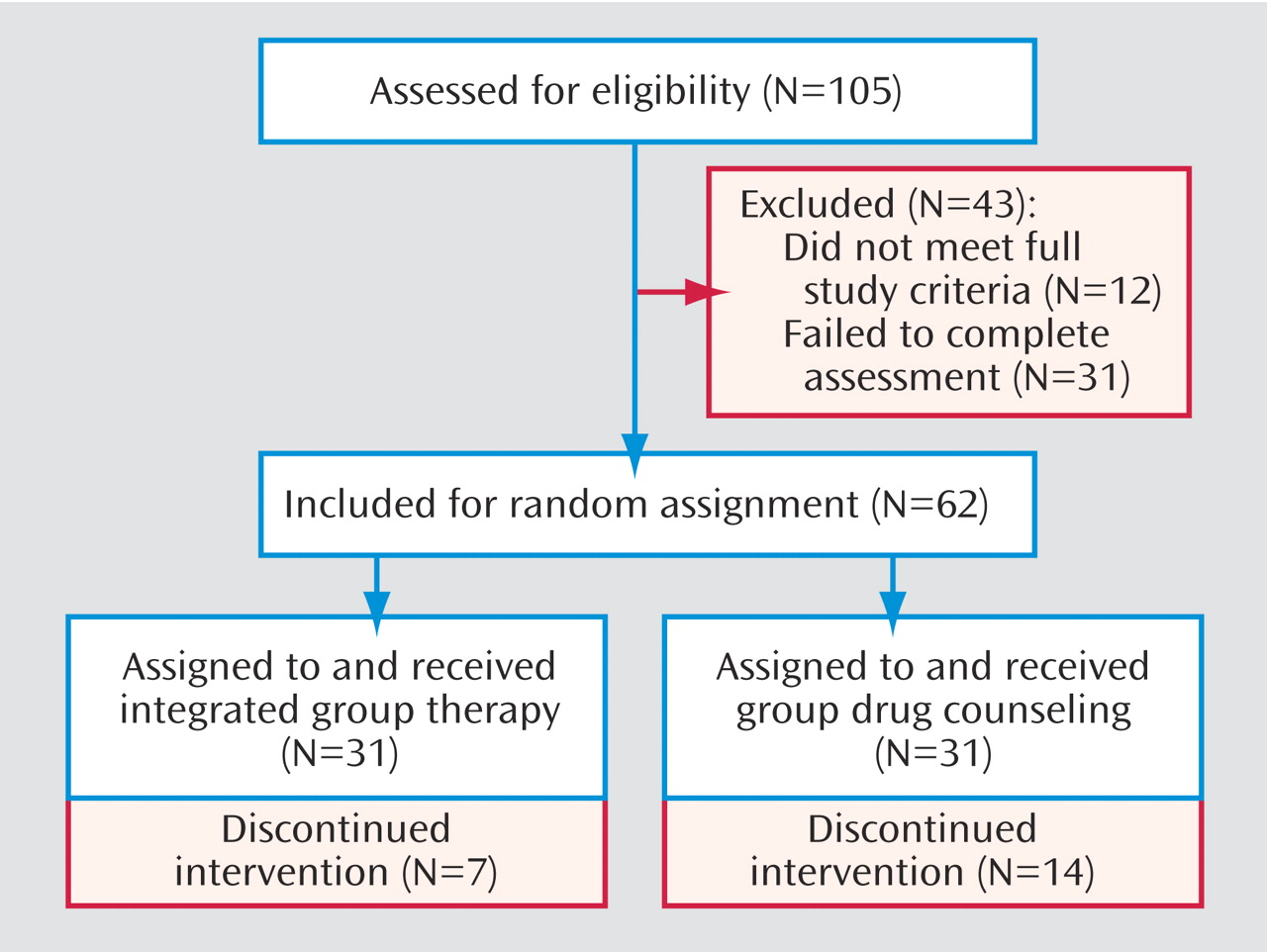
Among the 105 potential participants who met initial screening criteria of clinical diagnoses of bipolar disorder and substance dependence, 62 were randomly assigned, 31 failed to complete the assessment process, and 12 did not meet full study criteria. Eligible patients were randomly assigned to integrated group therapy or group drug counseling (
Figure 1 ); groups began within 2 weeks of each other. Five cohorts of group treatment were conducted for each modality, with five to eight patients per group.
Assessments
Substance use data were obtained by trained, supervised research assistants with the Addiction Severity Index
(20) at baseline and monthly throughout treatment and follow-up. The Addiction Severity Index is a widely employed, multidimensional assessment of substance-related problems. The Timeline Follow-Back technique
(21), which uses a calendar to assist recall, supplemented the drug and alcohol sections of the Addiction Severity Index. Urine toxicology screens to validate self-reports were obtained at group sessions and monthly assessments. We previously reported the high degree of validity of substance use self-report data in this population
(22) .
Mood was assessed with the Longitudinal Interval Follow-Up Evaluation
(23) : a combination of the Hamilton Rating Scale for Depression (HAM-D)
(24), the Young Mania Rating Scale
(25), and the Structured Clinical Interview for DSM–IV, utilizing calendar methodology to review mood weekly. The HAM-D and Young Mania Rating Scale were administered monthly by the research assistants; the Structured Clinical Interview for DSM–IV was completed by the study psychologist at baseline and at months 3, 5 (end-of-treatment), and 8. Our primary measure of mood was weeks ill, i.e., the number of weeks in which criteria were met for a depressive, manic, hypomanic, or mixed mood episode. The Longitudinal Interval Follow-Up Evaluation also generates an overall weekly course rating, ranging from 1 (usual self) to 6 (full episode, severe).
The research assistants and study psychologist received standardized training on the assessments, using videotapes and written materials developed by the instrument’s authors (for the Addiction Severity Index and Structured Clinical Interview for DSM–IV) or by experts in the field (for the Longitudinal Interval Follow-Up Evaluation, HAM-D, and Young Mania Rating Scale). Research assistants conducted practice interviews in front of the study psychologist before interviewing study participants and were observed monthly thereafter (with independent ratings and discussion after each interview) to ensure continued proper administration and to avoid drift. The psychologist was blind to participants’ treatment condition; the research assistants, because of their involvement in all aspects of the study, were not blinded to treatment condition after baseline.
Treatments
Integrated group therapy
(16) consists of 20 weekly hour-long meetings; it employs a cognitive behavioral relapse prevention model that integrates treatment by focusing on similarities between recovery and relapse processes in bipolar disorder and substance use disorder. A foundation of integrated group therapy is that the same types of thoughts and behaviors that facilitate recovery from one disorder will enhance the likelihood of recovery from the other disorder. Conversely, similar types of thoughts and behaviors can impede recovery from both disorders. Most sessions deal with topics relevant to both disorders (e.g., “Dealing With Depression Without Using Alcohol or Drugs”). The interaction of the two disorders is emphasized, for example, by focusing on the adverse impact of substance abuse on the course of bipolar disorder. A “check-in,” during which patients report their week’s substance use, mood, medication adherence, and high-risk situations, is followed by the session topic, combining didactic presentation and discussion.
Group drug counseling
(17) is an adaptation of the treatment delivered in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study
(14) . Group drug counseling, designed to approximate the treatment delivered in community substance abuse treatment programs, also consists of 20 weekly hour-long sessions, each focusing on a specific topic. The goals of group drug counseling are to 1) facilitate abstinence, 2) encourage mutual support, and 3) teach new ways to cope with substance-related problems. Sessions begin with a check-in on substance use and craving, followed by substance use disorder-related session topics that do not address mood issues. Group drug counseling is thus distinguishable from integrated group therapy by its focus on substance use, rather than the dual focus of integrated group therapy on substance use disorder and bipolar disorder. Group drug counseling counselors respond to mood-related issues by discussing them briefly, then referring patients to their prescribing physician. Counselors attend to emergencies, however, until they are resolved.
Therapists
Integrated group therapy leaders were doctoral or master’s-level therapists with ≥3 years of substance use disorder and psychiatric treatment experience. Group drug counseling leaders were master’s-level therapists or counselors with ≥3 years of experience treating substance-dependent and dually diagnosed patients. The 10 group cohorts (five per treatment) were led by four integrated group therapy and four group drug counseling therapists: two men and two women in each treatment; one therapist for each treatment conducted two groups. Therapists led groups for only one treatment.
To encourage fidelity to the manuals, group sessions were videotaped, and leaders were supervised weekly by the senior author of the respective manuals (Dr. Weiss for integrated group therapy, Dr. Daley for group drug counseling). Adherence/competence rating scales were completed by the supervisor after each session. For the integrated group therapy pilot study, we developed a 20-item therapist adherence and competence scale, covering skills related to group therapy (e.g., “attended to cues”), substance use disorder groups (e.g., “stressed the importance of abstinence”), and integrated group therapy-specific items (e.g., “focused on the effects of bipolar disorder and substance use disorder on each other”).
A 20-item group drug counseling adherence/competence scale was originally developed for the National Institute on Drug Abuse Collaborative Cocaine Treatment Study, with items on supporting recovery, encouraging 12-step participation, and facilitating group participation. Previous research
(14) established this scale as psychometrically sound, with good interrater reliability.
In the current study, two master’s-level raters, blind to treatment, completed both group drug counseling and integrated group therapy adherence/competence scales after viewing 34 complete integrated group therapy and group drug counseling session tapes. Both raters could distinguish between conditions on all tapes. The integrated group therapy scale was evaluated for interrater reliability, using intraclass correlations, with intraclass correlations ≥0.70 designated as acceptable. Fifteen of 20 integrated group therapy adherence items met this criterion; the remaining five were deleted. We tested the fidelity of the scales to the treatments by comparing adherence scores. We found that all five “integrated group therapy-specific” adherence items scored significantly higher in integrated group therapy sessions than in group drug counseling sessions; all “group drug counseling-specific” adherence items scored significantly higher in group drug counseling sessions. As expected, other items (e.g., advocating abstinence) scored similarly for both treatments.
Each therapist showed good treatment adherence and competence; all therapists achieved mean adherence and competence ratings ≥3.0 (designated as acceptable) on a 0–4 scale.
Statistical Analysis
Background characteristics of integrated group therapy and group drug counseling participants were compared, using chi square tests for categorical variables and t tests for continuous variables. Our primary outcome was the number of days of substance use during treatment. Secondary outcomes were the number of days using any alcohol, days using alcohol to intoxication, days of drug use, and Addiction Severity Index Drug Use and Alcohol Use composite scores. Our primary mood outcome was the number of weeks ill with a mood episode. An intention-to-treat outcome analysis included data from all randomly assigned participants. Time-series random-effects regression modeling methods assessed integrated group therapy versus group drug counseling differences longitudinally during treatment and follow-up, with one-tailed significance tests, using Stata V8.2 for Windows
(26) . Generalized estimating equation methods were followed by generalized least squares methods, adjusted for heteroscedasticity, as appropriate. Each model included factors adjusting for time and corresponding baseline values. Time was treated as a linear predictor, which is supported by the figures. Treatment-by-time interaction terms were included in the models when significant. For analyses of secondary outcomes separating substance use into drug use and alcohol use, patients (N=14) with no lifetime drug use disorder and no drug use throughout the study were excluded from drug outcomes. Using an analogous procedure, one patient was excluded from analyses of alcohol outcomes.
Results
Baseline Characteristics
The patient cohort (31 integrated group therapy, 31 group drug counseling) was 51.6% female (N=32) and 93.5% white (N=58). Mean age was 41.9 (SD=10.9) years. Most participants were single (N=39, 62.9%), college graduates (N=36, 58.1%), and employed (N=33, 53.2%). The treatment groups were similar on these characteristics.
Fifty patients (80.6%) were diagnosed with bipolar I disorder, 10 (16.1%) had bipolar II disorder, and two (3.2%) had bipolar disorder not otherwise specified. Most patients (N=39, 62.9%) had both drug and alcohol use disorders, 17 (27.4%) had alcohol dependence only, and six (9.7%) had drug dependence only. Among those with drug use disorders, the most common primary drugs of abuse were marijuana (N=16), cocaine (N=10), sedative/hypnotics (N=9), and opioids (N=8), followed by amphetamines (N=1) and more than one drug (N=1). Neither bipolar disorder nor substance use disorder diagnoses varied by treatment group.
During the intake month, patients reported a mean of 11.7 (SD=11.0) days of substance use: 8.3 (SD=11.6) days of drug use and 8.5 (SD=10.0) days of alcohol use. The mean Addiction Severity Index Drug Composite score was 0.11 (SD=0.12), and the mean Addiction Severity Index Alcohol Composite score was 0.39 (SD=0.27). The mean baseline HAM-D score was 13.5 (SD=8.8), and the mean Young Mania Rating Scale score was 10.5 (SD=7.6). At intake, the median course severity rating on the Longitudinal Interval Follow-Up Evaluation was 4 on a 1–6 scale. A score of 4 corresponds to ≥1 DSM–IV criterion score greater than mild but less than episode criteria. The median score for the week with the most severe mood disorder symptoms during the 4 weeks at baseline was 5, corresponding to a full DSM–IV episode, mild to moderate. The treatment groups were similar on these baseline measures.
Pharmacotherapy
Valproate was the most commonly prescribed mood stabilizer at baseline (N=19, 30.6%), followed by lithium (N=15, 24.2%); nearly one-half (N=29, 46.8%) of patients were receiving more than one mood stabilizer. Mood stabilizer regimens did not differ significantly between treatment groups. The number of changes in mood stabilizers was examined to consider potential differences in medication management or effectiveness. Changes during treatment (mean=1.1 [SD=1.0]) and throughout the study period (mean=1.6 [SD=1.6]) did not vary by treatment group.
Other Treatment
Most participants (N=46, 74.2%) received individual psychotherapy, and one-half (N=32, 51.6%) attended 12-step self-help groups for substance use during the baseline month; neither attendance pattern differed by treatment group.
Substance Use Outcomes
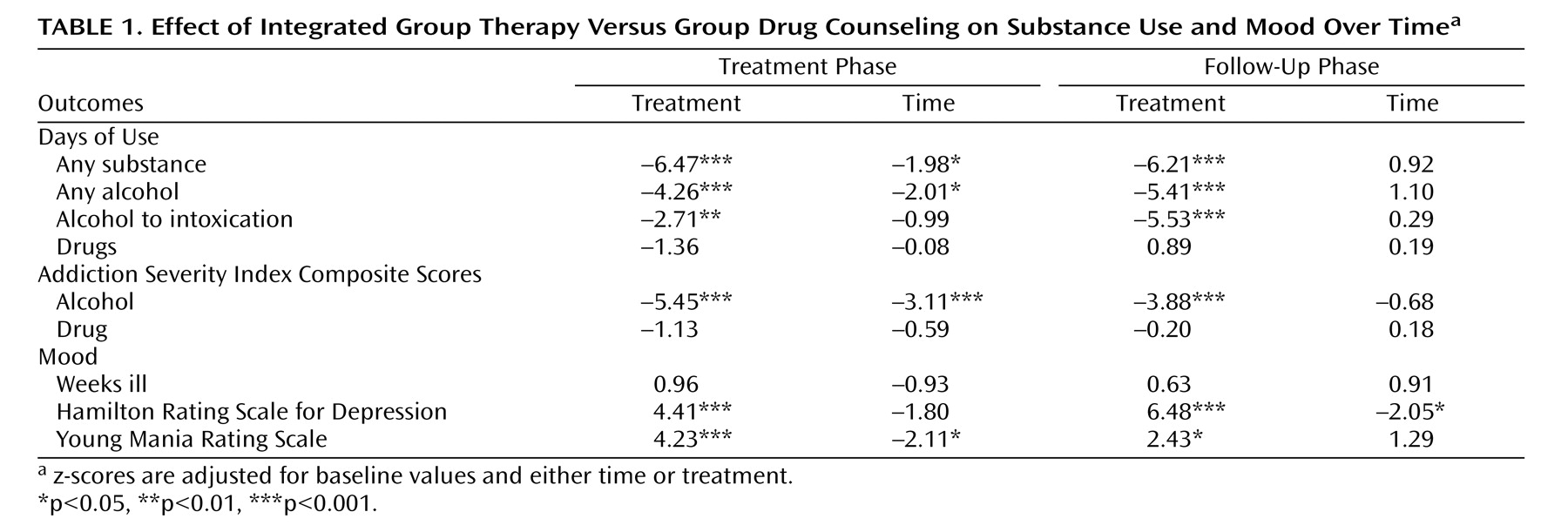
Overall, substance use decreased during treatment (
Table 1 ;
Figure 2 ). Integrated group therapy patients had fewer days of substance use than group drug counseling patients during treatment, adjusted for baseline levels and time; integrated group therapy patients reported approximately one-half as many days of substance use as group drug counseling patients during both treatment (5.3 [SD=6.6] versus 10.0 [SD=9.1] days/month) and follow-up (6.0 [SD=9.1] versus 12.0 [SD=10.8] days/month). During follow-up, substance use remained lower in integrated group therapy; the treatment-by-time interaction was also significant, showing that substance use fluctuated more in group drug counseling (z=2.00, p<0.03).
When drug and alcohol use were separated, integrated group therapy patients had fewer days per month of any alcohol use (treatment: 4.4 [SD=5.4] versus 6.5 [SD=7.4]; follow-up: 4.5 [SD=7.2] versus 7.8 [SD=9.3]) and alcohol use to intoxication (treatment: 2.8 [SD=4.1] versus 4.9 [SD=7.4]; follow-up: 3.1 [SD=5.5] versus 6.4 [SD=9.3]), both during treatment and follow-up (
Table 1 ;
Figure 2 ). Days of any alcohol use decreased for the entire cohort during treatment only. During treatment, for days using alcohol to intoxication, group drug counseling patients changed very little from baseline, whereas integrated group therapy patients improved considerably (z=–2.34, p<0.01). Days of drug use, conversely, did not improve over time or vary by treatment (
Table 1 ).
Similar improvement for integrated group therapy over group drug counseling was seen in Addiction Severity Index Alcohol Composite scores, during both treatment (0.20 [SD=0.18] versus 0.27 [SD=0.17]) and follow-up (0.18 [SD=0.18] versus 0.24 [SD=0.23] [
Table 1 ;
Figure 2 ]). Addiction Severity Index Drug Composite scores, however, did not decrease over time or vary by treatment (
Table 1 ).
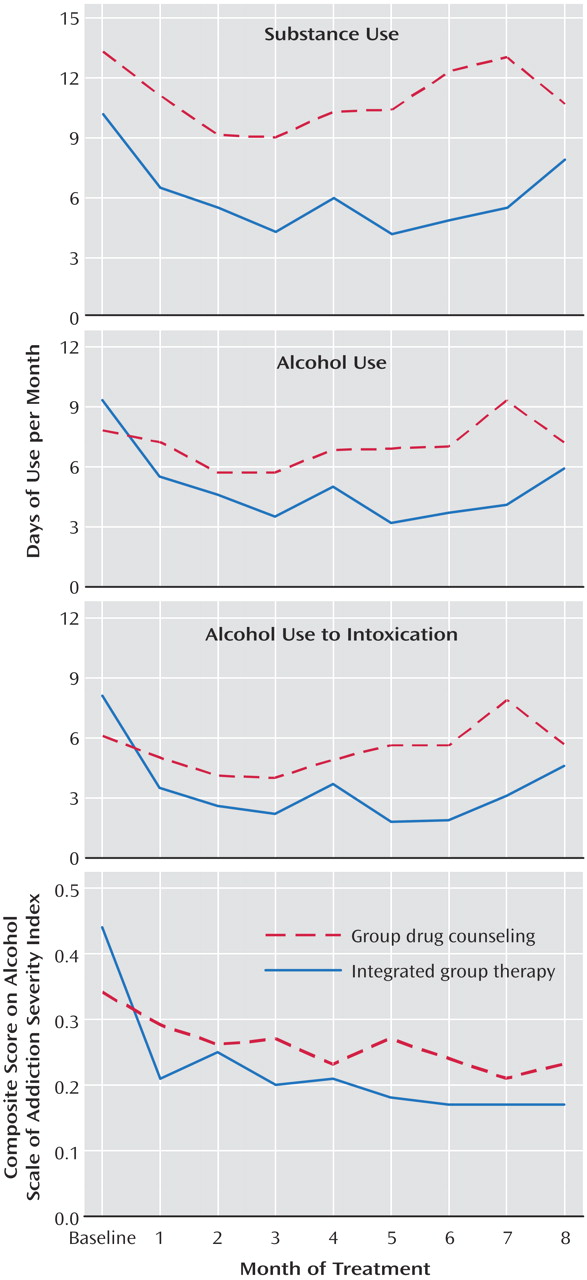
Examining abstinence from both alcohol and drugs again showed better outcomes for integrated group therapy, with a shorter time from treatment initiation to the first abstinent month (Hazard ratio=2.12; z=2.23, p<0.03 [
Figure 3 ]).
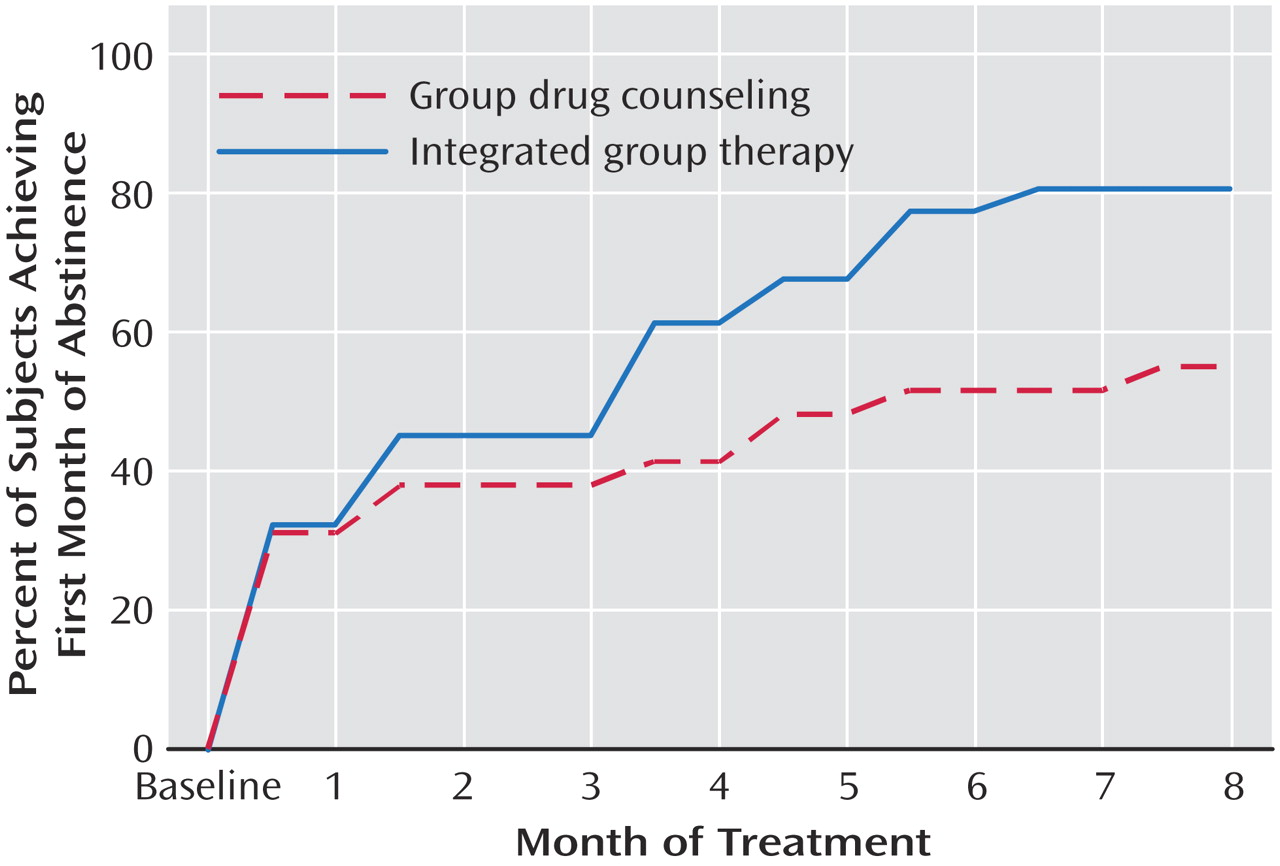
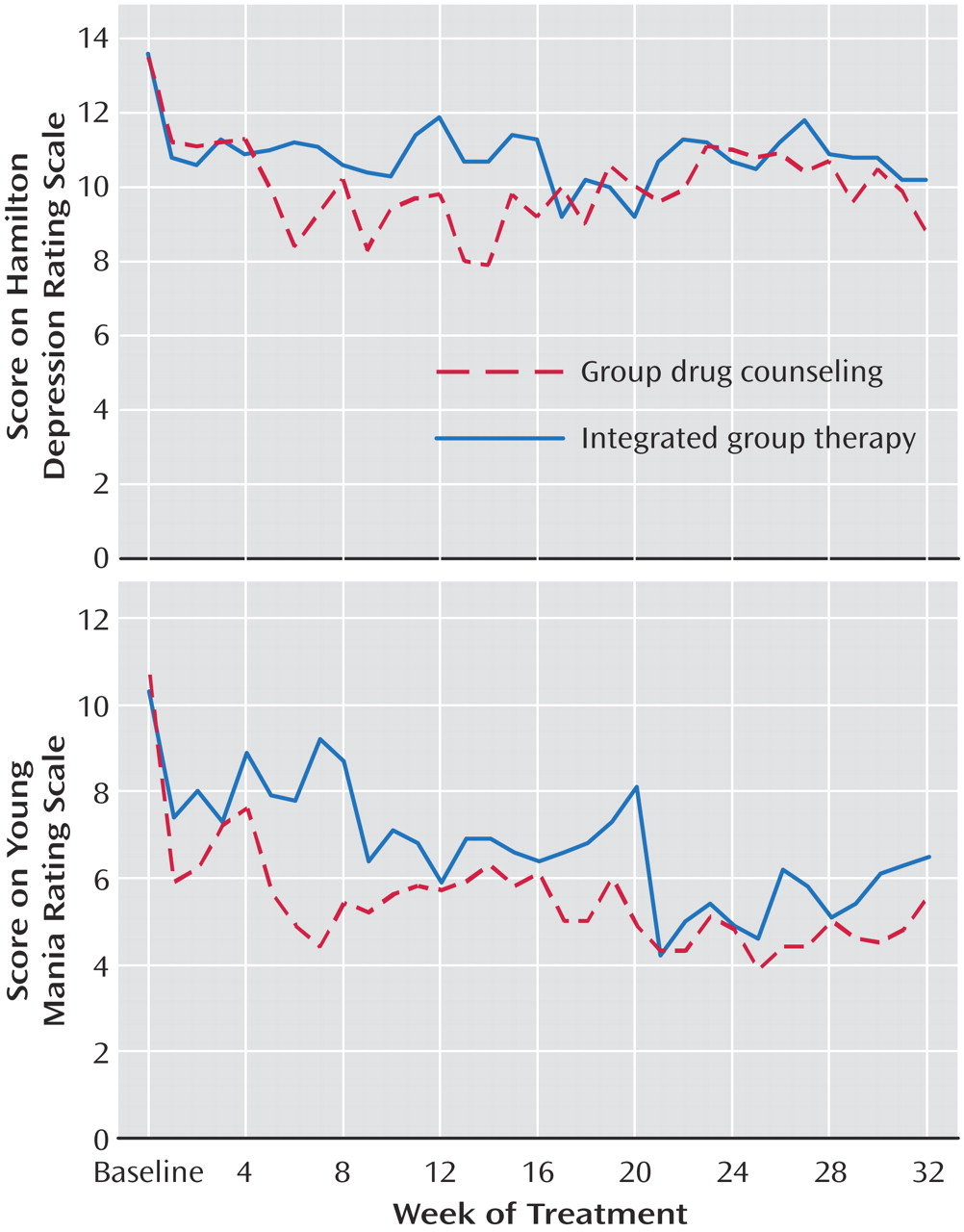
Mood Outcomes
Episodes of bipolar disorder were assessed as present or absent each week, as described previously. No differences were found between groups or over time during treatment or follow-up (
Table 1 ). However, analysis of HAM-D (
Figure 4 [top]) and Young Mania Rating Scale (
Figure 4 [bottom]) scores showed more depressive and manic symptoms for integrated group therapy patients during treatment and during follow-up. Unlike bipolar disorder episodes, Young Mania Rating Scale scores improved over time during treatment only. HAM-D scores, conversely, improved during follow-up only.
Cohort Effect
To test the possibility of a cohort effect, we conducted a deviance test, adjusted for treatment group and baseline substance use. No cohort effect was found for days of substance use, the primary outcome measure, during either treatment or last month of treatment.
Quality Assurance
Data Completeness
We designated two tiers of data, similar to the National Institute on Drug Abuse Collaborative Cocaine Treatment Study
(14) . “First-tier” data were collected in person. “Second-tier” data were collected via telephone interviews and mailed questionnaires. We collected substance use data on all eight study months for 59/62 participants. We collected exclusively first-tier data from 46 participants (74.2%) and a combination of first- and second-tier data from the rest; this did not vary by treatment group. There were no significant differences between first- and second-tier data in the frequency of reported substance use or mood episodes.
Self-Report Validity
We compared urine screens obtained at weekly group sessions with the corresponding monthly Addiction Severity Index data. Four participants failed to report drug use that was positive on their urine screens. Hence, only 2.0% of self-reports showed underreporting of drug use compared with urine data. In these situations, discrepancies were resolved at the next visit.
Group Session Attendance
Integrated group therapy patients attended more group sessions than group drug counseling patients (integrated group therapy: mean=69.6% [SD=25.2] versus group drug therapy: mean=54.3% [SD=33.4]; t=–2.03, df=55.8, p<0.05). Hence, we controlled for group attendance in the regression analysis; integrated group therapy patients continued to have fewer days of substance use during treatment than group drug counseling patients (z=–5.68, p<0.001).
Discussion
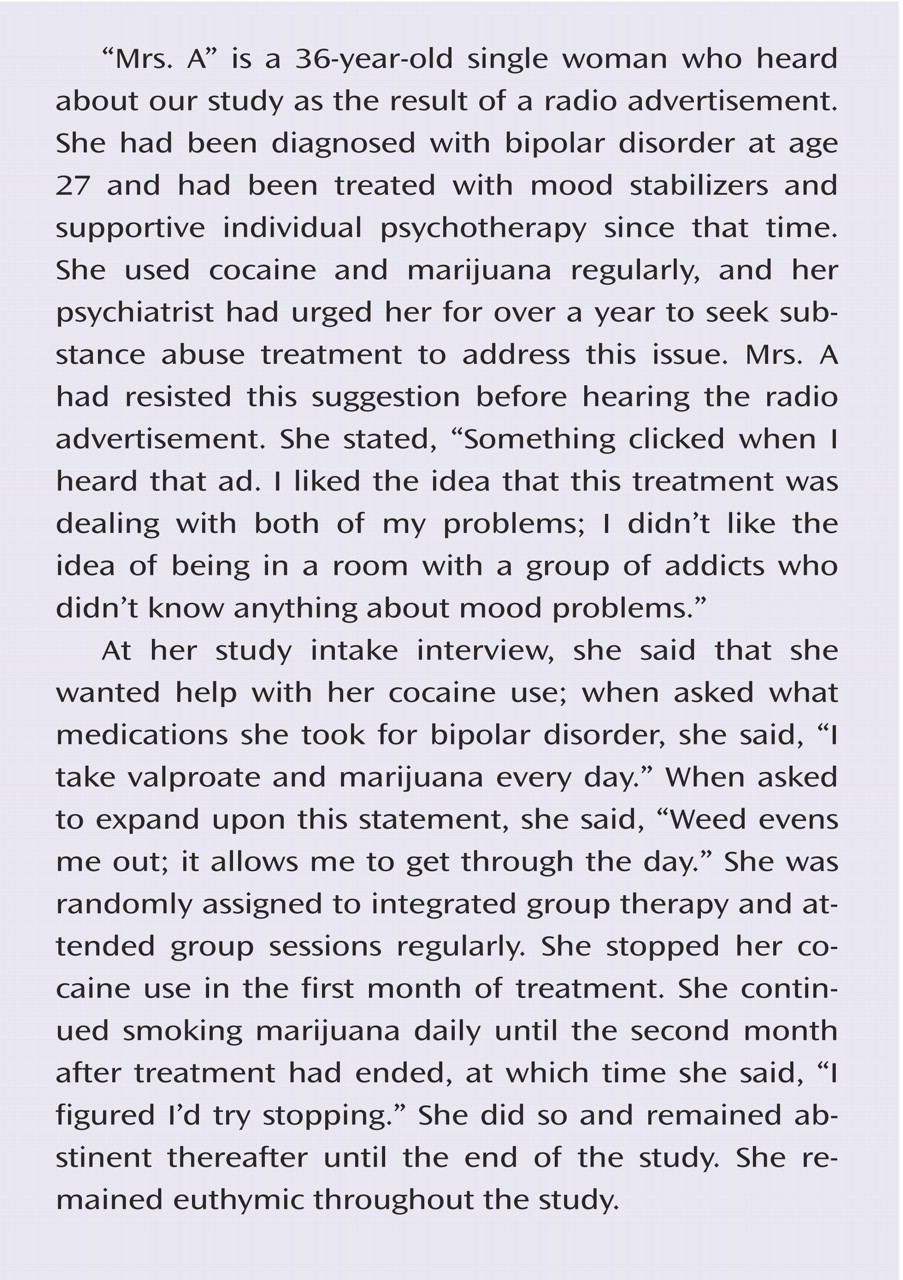
In this randomized controlled trial, a new group therapy integrating the treatment of substance use and bipolar disorders was more successful at reducing substance use than a group treatment concentrating on substance use. To our knowledge, this is the first controlled trial of a psychosocial treatment for this prevalent and difficult-to-treat population.
Notably, integrated group therapy had better substance use outcomes than group drug counseling despite more mood symptoms. Since the number of weeks ill was similar for treatment groups, it is likely that the differences in HAM-D and Young Mania Rating Scale scores represent subsyndromal mood symptoms. It is unclear, however, whether this finding reflects true mood differences or an increased level of awareness of subsyndromal mood symptoms among integrated group therapy participants. Since integrated group therapy stresses the importance of early recognition of mood symptoms, its participants may conceivably have endorsed these symptoms more readily. Another possibility is that integrated group therapy is particularly useful in helping patients cope with mood symptoms without using substances. Alternatively, reduced substance use may temporarily worsen mood symptoms in some patients with bipolar disorder.
The positive finding for integrated group therapy in substance use and not mood could be viewed as paradoxical, since the major difference between the treatments was the integrated group therapy focus on mood. However, patients who believed that their mood problems were being addressed may have been more willing to accept the group’s concurrent emphasis on substance use. This explanation would be consistent with findings from our pilot study of integrated group therapy versus no group therapy
(17) ; patients who initially believed that their substance use had improved their bipolar disorder symptoms were most likely to benefit from integrated group therapy
(27) . Integrated group therapy explicitly addresses the notion that patients perceive their substance use as “self-medication” and discusses the hazards of self-treatment. This emphasis may have facilitated the reduction in substance use among the integrated group therapy patients in the current study.
Integrated treatment, which addresses both disorders simultaneously, has long been recommended for patients with substance use disorder and psychiatric illness
(28), although data supporting its superiority to standard substance use disorder treatment have not been uniformly positive
(29) . Integrated treatments have been tested for patients with other psychiatric disorders, including schizophrenia
(30 –
32) and posttraumatic stress disorder
(33,
34) . To our knowledge, ours is the first study to compare an integrated approach directly with standard substance use disorder treatment for patients with co-occurring bipolar disorder. Drake et al.
(35) reported improvement in both disorders among 51 patients with bipolar disorder and substance use disorder receiving 3 years of integrated dual diagnosis treatment designed for patients with severe and persistent mental illness (not exclusively bipolar disorder). However, the absence of a comparison group makes it unclear how these patients would have fared with a nonintegrated treatment model. “Integrated treatment” is variously defined, depending in part on the nature of the treatment setting as well as the specific disorder(s) being treated. Perhaps other models of integrated treatment, including more general “dual diagnosis” approaches, may also outperform standard substance abuse treatment for bipolar disorder patients. A group treatment focused on bipolar disorder might also perform well; a comparison of integrated group therapy with a bipolar disorder treatment group such as that developed by Colom et al.
(12) would be informative. We chose a substance use disorder-focused group as a comparison in this trial because substance use disorder is more common among patients with bipolar disorder than vice versa. Thus, clinicians treating patients for bipolar disorder are more likely to refer their patients for a substance use disorder-based intervention than the reverse.
Decreased alcohol use, not drug use, accounted for most of the differences in substance use between the groups. This could be related to our finding, similar to that of Drake et al.
(35), of reduced alcohol use, but not drug use, in the overall cohort. This result may have reflected a greater severity of alcohol problems (as evidenced by higher baseline Addiction Severity Index Alcohol Composite scores than drug severity scores) and thus more room for improvement and perhaps greater motivation among patients to address their drinking.
While most patients had both drug and alcohol use disorders, the participants had a variety of substance use disorders, and both treatments targeted substance use overall rather than specific substances. The superior outcome of integrated group therapy in facilitating abstinence corroborates its benefit in addressing substance use in this mixed population. The inclusion of patients with different substance use disorders increases the generalizability of our results, since homogeneity of substance use disorder within a population of patients with bipolar disorder would have yielded a highly restricted cohort. However, this heterogeneity of substance use disorders presents a methodological challenge
(36) ; we thus selected the number of days of any substance use as our primary outcome measure, one recommended strategy for behavioral treatment studies of patients with heterogeneous substance use disorders
(36) .
The greater frequency of group attendance by integrated group therapy patients may have contributed to better outcomes. However, when we controlled for group attendance, integrated group therapy patients still had fewer days of substance use than those receiving group drug counseling. Treatment attendance does not always correlate with outcome; in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study
(14), the most successful individual treatment had the lowest attendance rate
(14) . The high integrated group therapy attendance rate points to patient receptiveness to this treatment and thus its feasibility in clinical settings.
Study limitations include the exclusion of patients not motivated for the treatment of both disorders and those not taking a mood stabilizer. Thus, this cohort did not include some of the most difficult patients with these disorders. Moreover, the quality of pharmacotherapy may have varied between the two groups, although this is unlikely; corroborating evidence for this includes the lack of difference between the groups in type of mood stabilizer or frequency of mood stabilizer changes. Managing medication regimens in behavioral therapy trials of dually diagnosed patients is complex, and all approaches involve some compromise
(37) . Since there is no evidence that any specific mood stabilizer regimen is uniquely effective for patients with bipolar disorder and substance use disorder, we followed one recommended strategy
(37) by including patients taking different mood stabilizers. The lack of difference in individual psychotherapy or self-help group attendance suggests that differences in these interventions were also unlikely to account for the better outcomes in integrated group therapy.
Study strengths included our unusually high degree of data completeness and the use of manual-based treatments and videotaped sessions with ongoing supervision to help ensure treatment quality and adherence. Our study results suggest that integrated group therapy can be conducted with excellent fidelity, has substantial patient acceptability, and has promising results for patients with both bipolar and substance use disorders. Since most patients with both disorders receive psychosocial treatment focused on one disorder or neither disorder
(19), integrated group therapy appears to fill a gap for this population, which has traditionally had poor outcomes.