That delusions can evoke violent actions by persons with psychotic disorders is evidenced on the pages of the daily newspapers and the evening television news
(1,
2). More sober confirmation of these lay accounts comes from numerous case reports in the psychiatric literature that detail the link between delusions and violence
(3). As greater attention has been paid to this issue, anecdotal accounts have been supplemented by systematic studies of forensic and civil patient populations
(4–
8), which have yielded the general conclusion that although most acts of violence perpetrated by psychotic persons are not motivated by delusions, a substantial minority of their violent acts appears to be delusionally driven.
To demonstrate that delusions can precipitate violence, however, is not to say that delusional persons are necessarily more violent than persons with other mental illnesses, or even than their neighbors in the general population. For example, violent acts committed for other reasons (e.g., instrumental violence) may be less likely for persons with delusions. Moreover, it may be that only some types of delusions are associated with violence, while others may lack such an association or even constitute protective factors. Thus, the role of delusions as predictors of violent behavior among persons with mental disorders remains unclear. Two recent series of studies, however, have addressed exactly these issues.
Link and colleagues
(9), in an epidemiologic study of community residents and current and former patients, found that patients and former patients were significantly more likely to have a history of violence than nonpatients. The difference between the groups was accounted for entirely by the patients’ psychotic symptoms. Subsequent analyses
(10) showed that only a subset of psychotic symptoms—denominated threat/control override delusions—accounted for this difference. Subjects were scored as having threat/control override delusions if they reported ever having beliefs that there were people seeking to harm them (threat) or that outside forces were in control of their minds (control override). As the number and intensity of threat/control override delusions increased, so did the risk of violent behavior. Confirmatory results were obtained by Link and his collaborators in a similar study of an epidemiologic sample in Israel
(11,
12).
Reanalyses of a portion of the data from the Epidemiologic Catchment Area (ECA) study by Swanson and colleagues
(13) have generally supported these findings. Drawing on interviews with more than 10,000 subjects in three communities, this group first established that the presence of delusions per se elevated the rate of reported violence almost fourfold. Although the authors used a different measure of threat/control override delusions than Link’s group, they also showed that subjects with these particular delusions were significantly more likely to be violent than other subjects
(14). (In some analyses, however, this effect was rendered nonsignificant by controlling for the presence of substance abuse disorders.) A second study that used an ECA patient subsample and a group of chronic patients from the Triangle Mental Health Survey found that threat/control override delusions were related to violence but only when the effects of treatment noncompliance were controlled
(15).
If true, these findings about delusions in general and threat/control override delusions in particular have important implications for the prediction and management of violent behavior in delusional patients. Not every study, however, has confirmed a higher risk of violence associated with the presence of delusions
(16,
17). The existing threat/control override data themselves, moreover, are less than ideal, being retrospective, having been gathered for other purposes, and having weak measures of delusions and violence (e.g., data often based exclusively on self-report). The data are, in addition, internally contradictory, with some analyses having suggested that threat/control override delusions account entirely for the effects of patient status on rates of violence
(10), while others have not
(14). Uncertainty also exists over whether the threat/control override effect is maintained in the presence of substance abuse and in the absence of psychiatric treatment
(14,
15).
Data from the MacArthur Violence Risk Assessment Study, a prospective, multisite study of violent behavior in persons recently discharged from psychiatric hospitals, offer another opportunity to examine the relationship between delusions and violence, including the threat/control override hypothesis. The study’s prospective approach and primary focus on violence avoid some of the methodological limitations of the earlier studies.
METHOD
Subject Recruitment and Interviewing
Methods of the study have been reported in detail elsewhere
(18,
19). In brief, subjects were approached soon after acute psychiatric hospitalization at three study sites (Worcester, Mass.; Pittsburgh; and Kansas City, Mo.) and asked to give written informed consent to participate in the study. Eligibility was limited to English-speaking white, African American, or Hispanic patients 18–40 years of age who were civilly admitted and had a medical record diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, depression, mania, brief reactive psychosis, delusional disorder, alcohol or other drug abuse/dependence, or a personality disorder. Of 1,695 potential subjects approached in a stratified random sampling design, 71.0% (N=1,203) agreed to participate, and 1,136 (67.0%) completed the interview after admission and formed the baseline sample.
Baseline data were collected in the hospital during 4–6 hours of interviewing by a research interviewer and a research clinician. The latter made a research diagnosis by using the DSM-III-R Checklist
(20). Subjects were then recontacted in the community after discharge by the research interviewers and were reinterviewed five times (every 10 weeks) over the subsequent year. At least one follow-up interview was obtained for 83.7% (N=951) of the subjects; three or more interviews were obtained for 72.0% (N=818). A collateral informant nominated by the subject as the person most familiar with his or her behavior in the community was also interviewed on the same schedule after having given written informed consent to participate. Three or more collateral interviews were obtained for 77.3% (N=878) of the collateral informants. Supplementary data were obtained from subjects’ hospital and arrest records.
Assessment of Delusions
To determine whether subjects were delusional, a set of questions taken mostly from the Diagnostic Interview Schedule
(21) was administered at baseline and at each follow-up interview. Interviewers were then asked to judge, according to DSM criteria and all information available to them, whether the subjects were possibly or definitely delusional or whether subject responses reflected reality or some other nondelusional perception (e.g., drug dealers on the subject’s front steps really were watching [“spying on”] him; subject’s expressed belief that someone was trying to “control” her was based on ex-husband’s withholding of child support payments). Delusions that appeared to be related to substance use were not excluded. At the baseline interview, assessment of delusions was performed by research clinicians (one Ph.D. and two with master’s degrees), with consultation from an experienced psychiatrist available at each site. Delusions were classified by using a DSM-based typology, and additional note was made of whether the delusions involved other people or contained violent ideation; these determinations were reviewed for consistency by the first author.
For subjects rated as definitely or possibly delusional, a more detailed assessment of the delusion identified as having the greatest recent impact on the subjects’ lives was conducted. (In some cases, the interviewer had to make this choice when the subject could not.) The assessment was conducted by using the MacArthur-Maudsley Delusions Assessment Schedule, an adaptation of the Maudsley Assessment of Delusions Schedule
(22), which generates scores on six non-content-related dimensions: conviction, negative affect, acting on belief, refraining from acting because of belief, preoccupation, and pervasiveness. Further details and psychometric data on the MacArthur-Maudsley Delusions Assessment Schedule have been presented elsewhere
(23).
Assessment of Violence
Incidents of violence were ascertained by interviewing subjects and collateral informants about the subjects’ behavior in the previous 10 weeks and by a review of subjects’ hospitalization and arrest records. Actions were considered to constitute violence if they were 1) batteries that resulted in physical injury or involved the use of a weapon, 2) sexual assaults, or 3) threats made with a weapon in hand. Acts judged to be in self-defense were not counted as violence. Batteries that did not result in injury or involve weapon use were coded separately as “other aggressive acts.” Violent acts reported by any information source were reviewed by two independent coders to obtain a single reconciled report of violence. A hierarchy of coding rules is available from the authors.
RESULTS
At baseline, the cohort was predominantly male (58.7%), white (69.7%; 29% were African American, and 1.8% were Hispanic), voluntarily admitted (58.1%), and between the ages of 25 and 40 years (75.3%; 24.7% were 18–24 years old). Primary research diagnoses for the subjects were depression or dysthymia (40.3%), schizophrenia or schizoaffective disorder (17.2%), bipolar disorder (13.3%), other psychiatric disorder (3.5%), alcohol or drug abuse/ dependence (23.9%), and personality disorder only (1.8%). The proportions of patients who committed acts of violence across the five follow-up evaluations were 13.5%, 10.3%, 6.9%, 7.6%, and 6.3%, respectively, with a 1-year aggregate violence rate of 27.5%. The frequency of delusions (definite or possible) across the baseline and five follow-up interviews was 28.9% (N=328); 16.7% (N=190); 16.1% (N=183); 14.0% (N=159); 12.1% (N=138); and 12.0% (N=136). Further details regarding the composition of the sample and the nature of the violence that was committed can be found elsewhere
(19).
Relationship Between Violence and Delusions
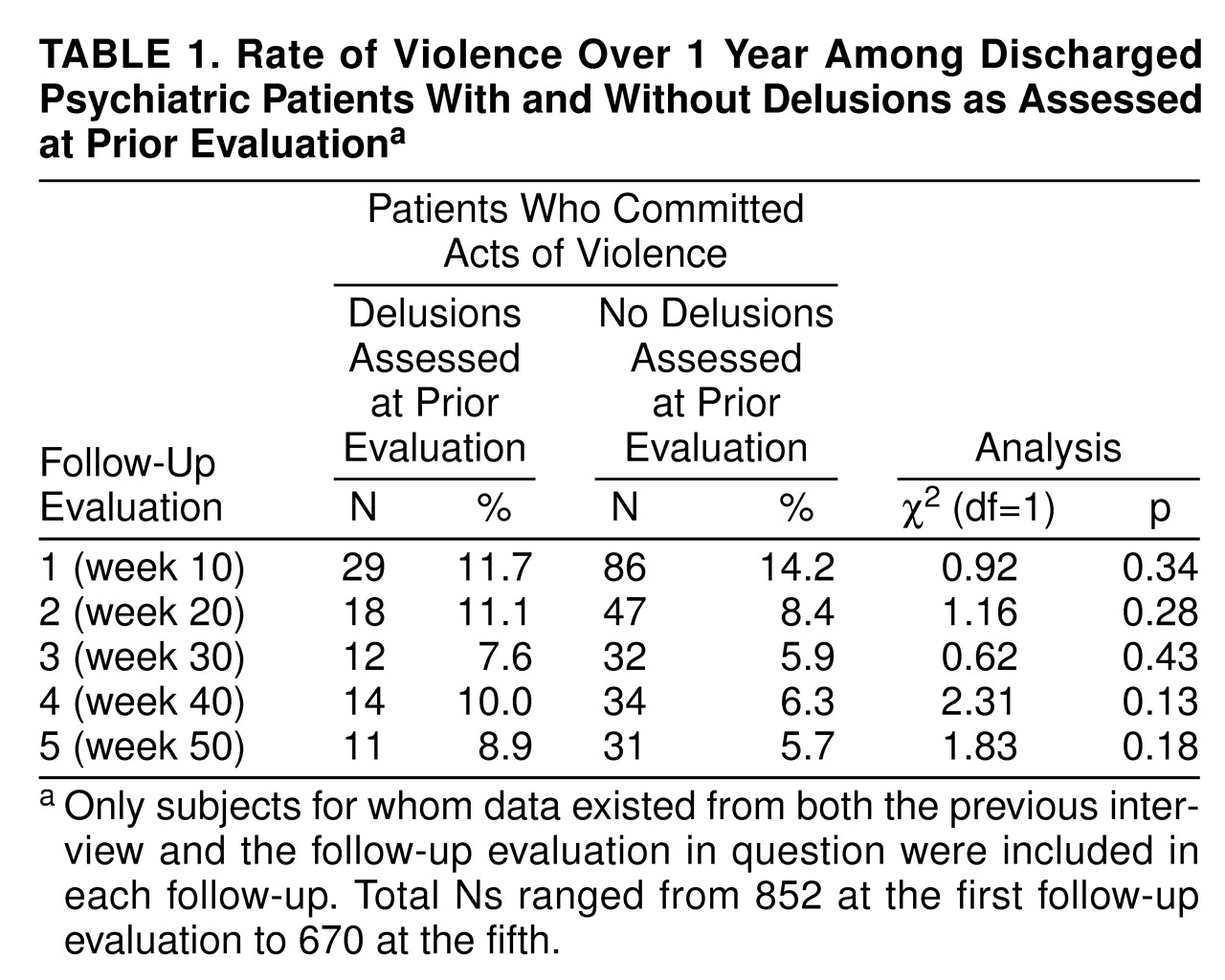
Table 1 compares the rate of violent acts reported at each follow-up evaluation for subjects who were and those who were not assessed as delusional at the previous interview. There were no significant differences in rates of violence between the two groups at any follow-up evaluation.
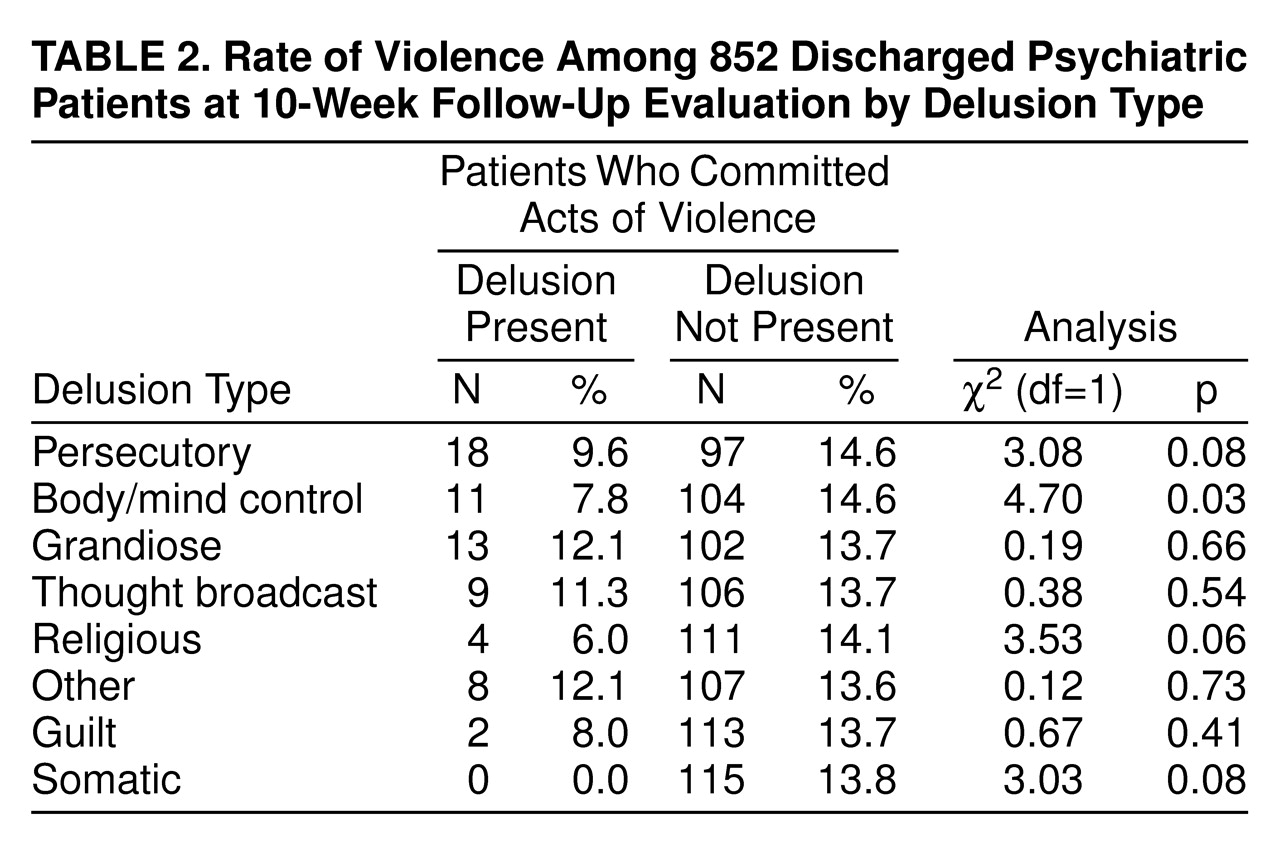
Next, we examined whether particular types of delusions might be associated with a higher likelihood of violent behavior. Here and in subsequent analyses we set the level of statistical significance at p<0.05 (two-tailed). Although an argument could be made that a more conservative value should have been employed because of the large number of comparisons made, we selected this significance threshold to provide the greatest opportunity for a possible relationship between violence and delusions to be demonstrated. The only significant findings came at the first two follow-up assessments (
table 2 displays the findings from the first), at which body/mind control delusions—contrary to what might be predicted by previous research on threat/control override delusions—displayed a negative relationship to the incidence of violence. In other words, subjects with body/mind control delusions were significantly less likely to commit violent acts during the subsequent 10 weeks than were subjects without such delusions. Because of the multiple comparisons made, the significance of even these relationships is questionable.
Delusions were also categorized according to whether the delusional content involved other people in general, violence in general, or violence that was specifically directed toward other people. None of these categories was significantly related to violence at any follow-up evaluation. Moreover, none of the non-content-related dimensions of delusions assessed by the MacArthur-Maudsley Delusions Assessment Schedule was significantly related to violence at any follow-up evaluation. Self-reported duration of delusions similarly had no relationship to subsequent violence at any follow-up assessment.
Possible Potentiating Variables
Given that neither the presence of delusions per se nor any of the content-related or non-content-related descriptors of delusions was positively associated with the occurrence of violence, we explored the possibility that the presence of selected concomitant variables—generally believed to potentiate violence—might influence the likelihood of violent behavior. Delusional subjects with command hallucinations at baseline (N=145), a group thought by some to be at higher risk of violence
(24), showed no greater rate of violence in the subsequent 10 weeks or at any follow-up evaluation than delusional subjects without such hallucinations (e.g., at the first follow-up assessment: χ
2=2.30, df=1, p=0.13; N=843). As shown in
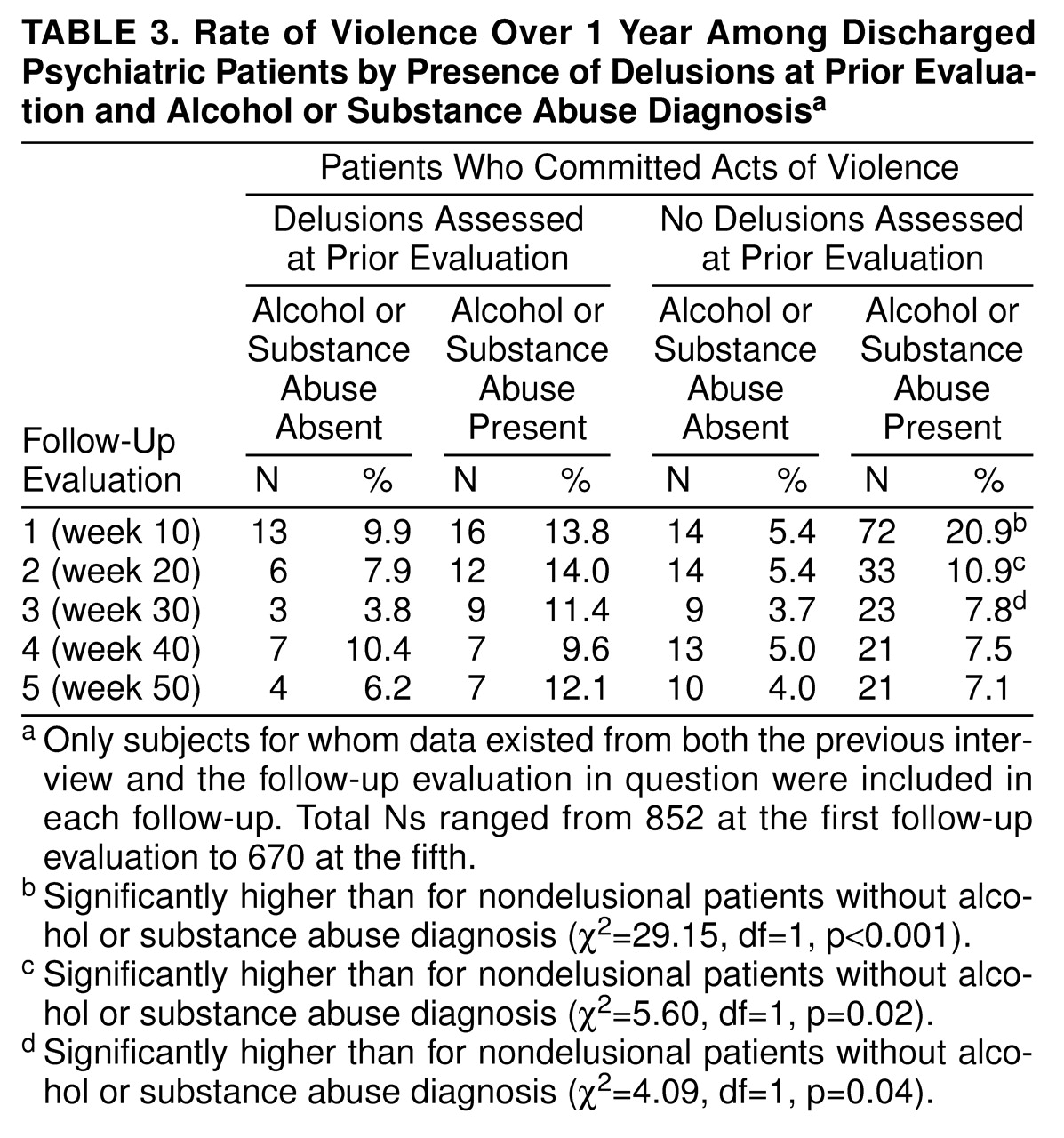
table 3, the same was true for subjects with research diagnoses of alcohol or drug abuse/dependence, although a significant potentiating effect of substance abuse was seen across the first three follow-up evaluations in the nondelusional group. A Mantel-Haenszel summary odds ratio analysis showed that there was no significant difference at any follow-up evaluation in the likelihood of violent behavior for subjects with and without a substance abuse diagnosis, in the presence or absence of delusions (e.g., at the first follow-up evaluation: χ
2=0.15, df=1, p=0.70).
Delusional subjects who reported at baseline having thought about committing violence (i.e., responding affirmatively to the question, “Do you sometimes think about hurting other people?”; N=260) were significantly more likely than delusional subjects without imagined violence to be violent at the first (χ2=14.89, df=1, p=0.03; N=849) and second (χ2=7.90, df=1, p=0.005; N=722) follow-up evaluations. However, comparison with the nondelusional group revealed this to be an effect of imagined violence per se; imagined violence had a significant effect on the rate of violence in the nondelusional group across all five follow-up evaluations (χ2=5.39–8.70, df=1, p=0.02–0.003). At the first follow-up assessment, for example, entering imagined violence into a logistic regression to predict violence yielded a significant effect (χ2=9.00, df=1, p=0.003), but there was no significant improvement from adding the delusions measure or the interaction term between imagined violence and delusions; similar findings were obtained at all subsequent follow-up evaluations.
The same was true for the concomitant presence at baseline of high psychopathy (score >12 on the screening version of the Revised Psychopathy Checklist
[25]; N=174), which also had a significant effect on violence rates among delusional subjects at the first (χ
2=12.20, df=1, p<0.001; N=785), second (χ
2=9.20, df=1, p=0.002; N=688), and fifth (χ
2=9.50, df=1, p=0.002; N=648) follow-up evaluations. But similar rates of violence were found among nondelusional subjects with high psychopathy scores. Entering psychopathy scores into a logistic regression yielded significant results (e.g., first follow-up: χ
2=76.80, df=1, p<0.001), but there was no significant improvement from adding delusions or the interaction term, which made it clear that the effect represents the influence of psychopathy alone. This was true for all follow-up evaluations.
Effect of Threat/Control Override Delusions
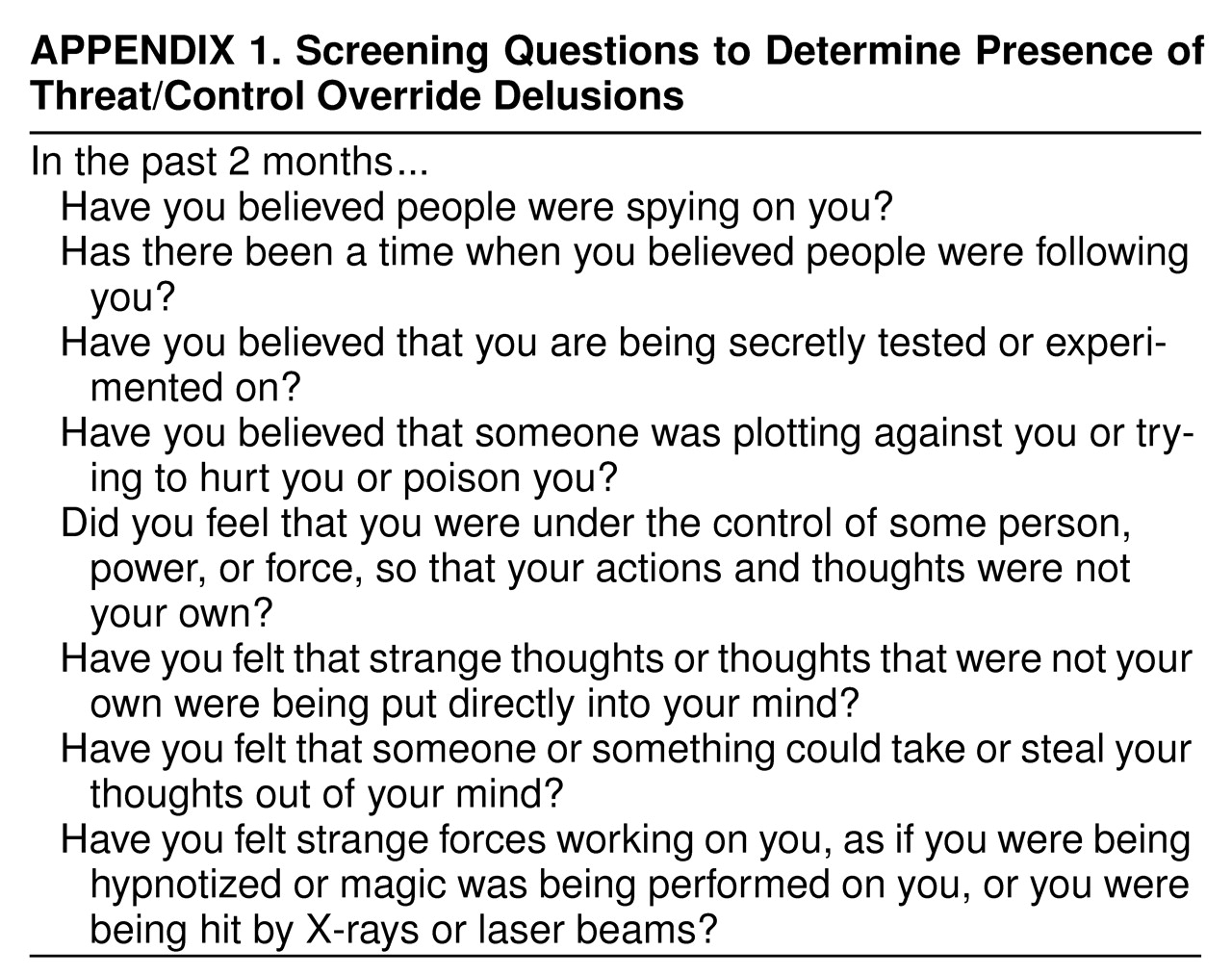
To test directly the effect of threat/control override delusions on violence in this sample, a subset of the questions used to screen for delusions was identified that best fit the threat/control override construct (
appendix 1). Four questions addressed the threat dimension, and four addressed the control override dimension. The resulting scale had high internal consistency (Cronbach’s alpha coefficient=0.82), with essentially no variation if any item was deleted. When we compared rates of violence in the subsequent 10 weeks for subjects who were and were not rated as having threat/control override delusions (
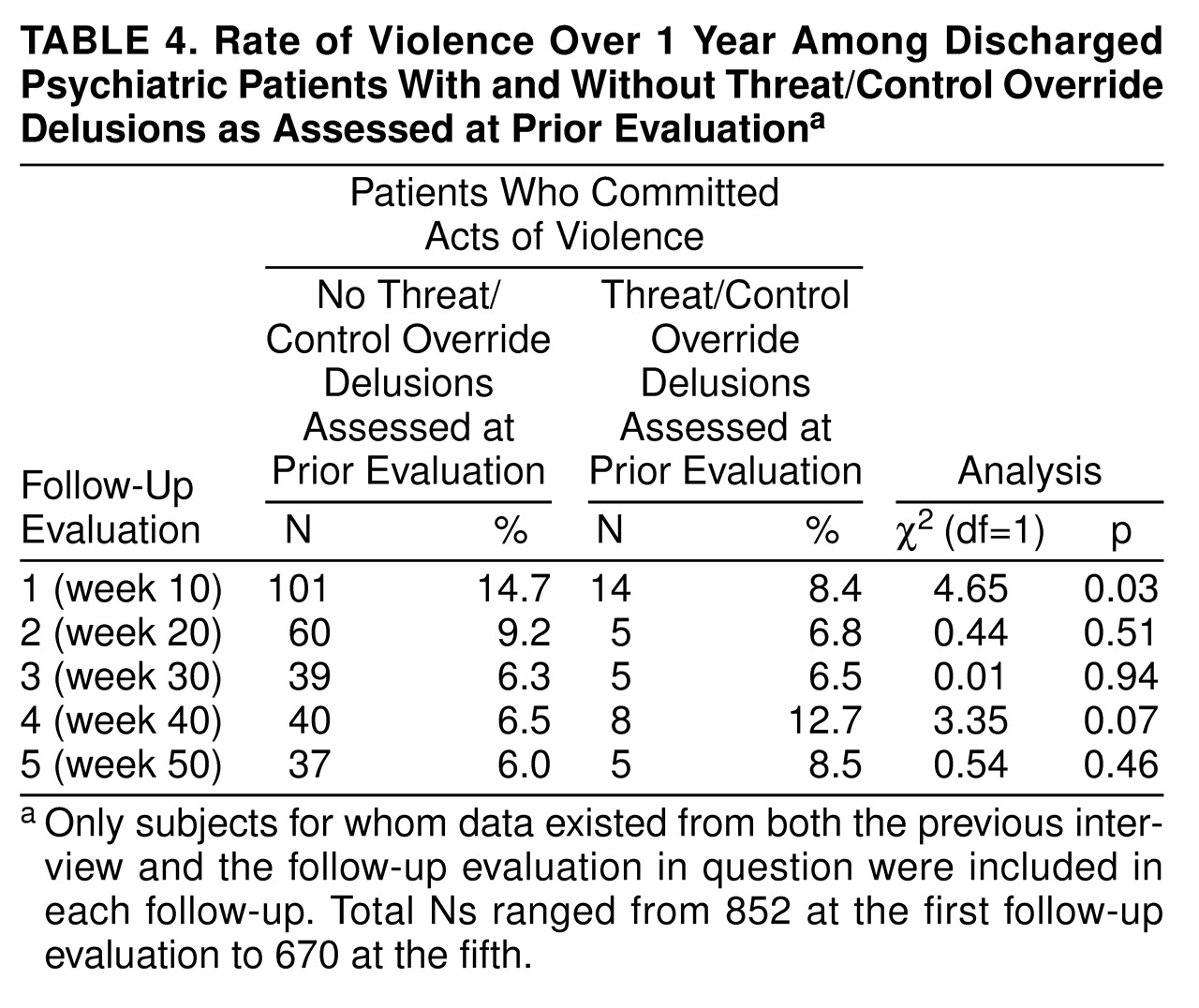
table 4), a significant difference was found between the two groups only at the first follow-up evaluation. At that point, subjects with threat/control override delusions, contrary to what was expected on the basis of previous studies, had a significantly lower rate of violence than those without such delusions. Also in contrast to previous studies, there was no significant relationship between the number of threat/control override delusions present and violent behavior at any follow-up evaluation.
Analyses were also performed separately to examine the relationship between threat/control override delusions and the four largest primary diagnostic groupings in the study: depression/dysthymia (N=355), schizophrenia/schizoaffective disorder (N=147), bipolar disorder (N=124), and alcohol or drug abuse/dependence (N=177). The only significant association occurred at the fourth follow-up visit for subjects with bipolar disorder (χ2=8.46, df=1, p=0.04; N=643). Given the number of analyses performed, this result is likely to represent a chance association.
To take advantage of data from all five follow-up evaluations to estimate the effect of threat/control override delusions on violence, the data were reanalyzed by using a discrete-time, event-history method
(26). For each follow-up period during which a subject was known to be at risk of committing a first violent act, a separate observational record was created. Individuals for whom no violent act was recorded by the end of the study (i.e., censored individuals) thus contributed a maximum of five observational records to the analysis file. Explanatory variables included threat/control override symptoms for each subject at each follow-up, as well as a series of four indicator variables that collectively represented the five follow-up periods. Logistic regression was used to estimate the probability that an individual would commit a violent act given that one had not been previously committed (i.e., the hazard rate of violence). The results of these analyses (N=3,542) confirmed the absence of a significant predictive effect (odds ratio=0.71, 95% confidence interval=0.46 –1.10) of threat/control override delusions on violence (Wald test=2.35, df=1, p=0.13).
Comparison With Earlier Studies
Because of the failure to confirm the results of earlier studies
(10–
12,
14,
15), several methodological explanations were considered. First, the possibility was examined that the different criteria used for threat/control override delusions in this study affected the outcome. Close approximations to the criteria used by Link and Stueve
(10) and by Swanson et al.
(13,
14) were constructed from our data. Our threat/control override criteria at baseline correlated moderately with those of Link and Stueve (r=0.64, N=1,136, p<0.0001) and highly with those of Swanson et al. (r=0.96, N=1,136, p<0.0001), which, in turn, correlated moderately with each other (r=0.68, N=1,136, p<0.0001). Although some of the variance between our findings and Link and Stueve’s may be accounted for by the difference in criteria, this cannot explain the failure to replicate the results of Swanson et al. Moreover, the correlation between our criteria and Link and Stueve’s was highly significant and roughly the same as the correlation between the criteria from the other two studies.
Second, we explored whether differences in measurement of the outcome variable (i.e., violence) might have accounted for the contrast in our findings. Previous studies did not restrict reports of violence, as this study did, to instances in which harm resulted, weapons were used, or sexual assaults occurred. However, even redoing the analyses in
table 4 by adding “other aggressive acts,” which included all batteries without injury, to the outcome measure yielded no significant relationship with threat/control override delusions at any follow-up evaluation. The same was true when we redid the discrete-time, event-history analysis with the expanded outcome measure.
A third methodological difference involved the use of prospective versus retrospective determinations of the relationship between threat/control override delusions and violence. Previous studies all had asked about threat/control override symptoms and violence during some previous period. Our analyses focused on the prospective predictive effect of the presence of threat/control override delusions. As with all retrospective methods, the earlier studies may have introduced unspecifiable biases into the data. When data from the current study were reanalyzed retrospectively (i.e., examining the relationship between the occurrence during the previous 10 weeks of both threat/control override delusions and violence), there were no longer significant findings in the “unexpected” direction. Overall, there were no significant differences between subjects who did and those who did not report threat/control override delusions. Thus, this methodological issue, taken by itself, may have played some small role in producing different outcomes among the studies.
The final methodological issue involved the manner of determining the presence of threat/control override delusions. Earlier studies of Link and Stueve
(10) and Swanson et al. (13, 14) relied on subjects’ answers to screening questions. (The study of Link et al. [
11,
12] from Israel, however, also used psychiatrist-rated delusion items from the Schedule for Affective Disorders and Schizophrenia.) Thus, for the most part, if subjects responded affirmatively to a question regarding, for example, whether someone was trying to do them harm, they were rated as having a threat/control override delusion. (In a Dec. 1998 personal communication, Swanson reported that the lay ECA interviewers had the option of rating responses to two of the four items incorporated into his threat/control override measure as “plausible,” i.e., presumably nondelusional. If so rated, responses were not considered indicative of threat/control override symptoms in his studies. He reported that “not many” responses were excluded on this basis.) In contrast, the interviewers in our study were instructed to probe subjects’ responses and to assess, on the basis of all data available to them (including the subjects’ medical records at baseline), whether subjects actually were delusional. This process resulted in a reduction of the number of persons who could be rated at baseline as having threat/control override delusions, from the 532 subjects who responded affirmatively to at least one threat/control override screening question to the 230 who were judged to have a threat/control override delusion. When additional reanalyses that included all subjects with self-reported threat/control override symptoms were performed, a significant difference was found at the second follow-up evaluation in the expected direction (i.e., persons reporting threat/control override symptoms were more likely to be violent) (χ
2=6.19, df=1, p=0.01; N=726). This methodological difference, therefore, may have accounted for some portion of the discrepancy between our results and those of earlier studies.
In an effort to duplicate the methods of the earlier studies as closely as possible, a set of analyses was run by using both a retrospective approach and relying on subjects’ self-report of symptoms. Persons with self-reported threat/control override symptoms had higher rates of violence in the previous 10 weeks at baseline (χ
2=11.12, df=1, p=0.001; N=1,136) and at every follow-up evaluation. This essentially replicated the results of the earlier studies. Exploring the characteristics of this group, we found that self-reported threat/control override symptoms at baseline had significantly stronger correlations with all four subscales of the Novaco Anger Scale
(27) (testing for differences between two nonindependent correlation coefficients
[28], t=4.08–6.24, df=1130, p<0.001) and with all three subscales of the Barratt Impulsiveness Scale
(29) (t=2.37–3.31, df=1121, 0.05>p<0.001) than did clinician-rated threat/control override delusions. Controlling for the effect of these anger and impulsivity measures eliminated the significant association between self-reported threat/control override symptoms and violence at every measurement point.
DISCUSSION
Contrary to popular wisdom and to the results of several other studies, the data from this study suggest that the presence of delusions does not predict higher rates of violence among recently discharged psychiatric patients. This conclusion remains accurate even when the type of delusions, their content (including violent content), and their non-content-related dimensions are taken into account. Of the variables known to correlate with violence (including substance abuse and psychopathy) among persons with delusions, few potentiating effects could be demonstrated. Indeed, the usual increase in the rate of violence among substance abusers was absent among delusional patients.
Previous studies
(10–
12,
14,
15) have suggested that a particular subgroup of delusions displaying threat and control override characteristics represents an important risk factor for violence in the general population and in several patient groups. Our data fail to support that conclusion, at least for patients recently discharged from acute psychiatric facilities. We can replicate the earlier findings only by including a large number of presumptively nondelusional symptoms under the threat/control override rubric, or by looking at the data retrospectively, with all the potential for bias that this method entails. Assuming that the relationship previously found between threat/control override symptoms (including both delusional and nondelusional symptoms) and violence is not entirely an artifact of the retrospective method, it may be accounted for by an association between a generally suspicious attitude towards others—with associated anger and impulsiveness—and violent behavior. This is in keeping with the suggestion of Estroff and colleagues (personal communication, January 1999), who similarly reported a failure to support the threat/control override hypothesis with a chronic mentally ill population (cited in
14). Our data supported this finding in that controlling for anger and impulsiveness wiped out the effect on violence found in the retrospective analyses of self-reported threat/control override symptoms.
These data, of course, should not be taken as evidence that delusions never cause violence. It is clear from clinical experience and from many other studies that they can and do. But our findings are probably in accord with those of Junginger et al.
(5), who found in a survey of 54 delusional inpatients that “delusional motivation of violence is rare.” This may be because, as previously suggested
(14), delusions are often associated with chronic psychotic conditions that are frequently attended by social withdrawal and the development of smaller social networks. Delusional subjects in the community, therefore, may have less desire and fewer opportunities to engage in the interpersonal interactions that can lead to violence compared with less severely ill patients. Although we cannot support this hypothesis from our data (controlling for social network size did not affect the relationship between threat/control override symptoms and violence), it is deserving of further exploration.
The implications of these data for clinical assessment and management of violent behavior are worth considering. Needless to say, it would be prudent to await independent verification of these findings before broadly applying them to clinical practice. Even on their face, however, they do not disprove the clinical wisdom that holds that persons who have acted violently in the past on the basis of their delusions may well do so again. Nor do they provide support for neglecting the potential threat of an acutely destabilized, delusional person in an emergency setting, in which the person’s past history of violence and community supports are unknown. However, these data do suggest that the persistence of delusions in a person who has been hospitalized and treated, and who is otherwise ready for release, by itself should not preclude the formulation of an appropriate discharge plan. Similarly, the presumed risk of violence associated with delusions per se does not justify hospitalization of a patient, in the absence of other indicators of violence risk or of other reasons for inpatient treatment.
APPENDIX 1.