Of the medical specialties, psychiatry will ultimately be most called upon to deal with the aftermath of the September 11 World Trade Center tragedy. In the wake of the bombing, innumerable organizations and individuals have declared their readiness to apply a variety of therapeutic techniques to assist those exposed to the traumatic events. Some of these interventions have been established as effective treatments by rigorously conducted clinical trials. Others are merely sensible intuitively. Still others, although never disproved, appear to lack credence. The key question is “What can psychiatrists reasonably recommend to those suffering from the emotional disturbances that follow exposure to a life-threatening traumatic event?”
Many people are complaining of nightmares, flashbacks, insomnia, traumatic grief, emotional numbing, depression, and avoidance. Unfortunately, experience with previous disasters may not be informative in the present context for at least two reasons. First, the magnitude of this tragedy dwarfs all others in American history. Second, the trauma is not time limited but is persisting long after the initial incident as a result of continued threats by terrorist groups, military action, and by the availability—in fact unavoidability—of information about the events (past, present, and possible) from the media.
Most medical interventions are based on an understanding of the basic anatomy and physiology of the organ involved in the particular disease. For example, treatments of cardiac rhythm disturbances now mainly stem from a thorough understanding of the normal electrical conduction system of the heart provided by basic and clinical science. Similarly, although originally based on fortuitous discoveries, current therapeutic discoveries for infectious diseases are grounded in molecular and cell biology. These types of insights have been difficult to derive for psychiatric illnesses but when available should be heeded. In the case of responding to a fear-arousing event, much is already understood about the basic anatomy and physiology from pre-clinical research, and it is this information that might be profitably turned to for a scientifically grounded idea about fear and its control.
It is well known that stimuli previously associated with physical harm come to elicit protective reactions in anticipation of the arrival of the harmful stimulus. In laboratory studies this is called classical or Pavlovian conditioning, a procedure in which an experimental animal is exposed to a meaningless conditioned stimulus, such as a tone, together with a harmful unconditioned stimulus, often an electric shock to the feet. After a single or at most a few pairings, presentation of the conditioned stimulus alone is capable of producing a characteristic pattern of behavioral and physiological responses: blood is redistributed from the skin and gut to the skeletal muscles, and stress hormones (cortisol and catecholamines) surge as the animal freezes, anticipating the shock. The animal has come to fear a stimulus that was, just moments before, meaningless.
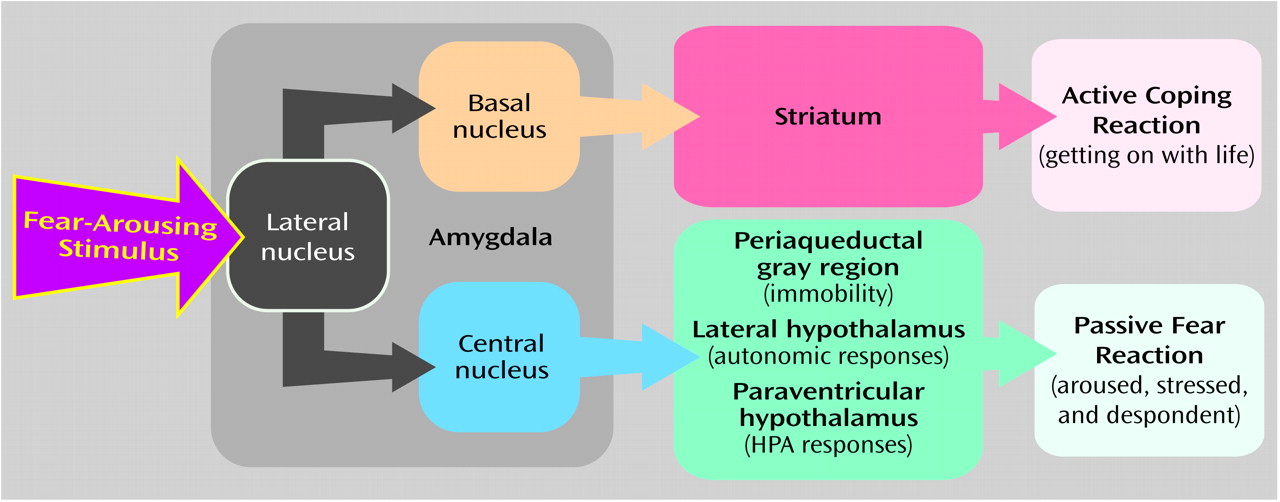
The anatomical pathways necessary for the development of conditioned fear have been mapped in detail (
Figure 1). The conditioned stimulus is first relayed from the external environment through the sensory pathways to the thalamus and cortex, and from each of these stations to the lateral nucleus of the amygdala. The lateral nucleus is responsible for the linking of the conditioned stimulus and unconditioned stimulus and thus the formation of the memory of the experience. This memory then serves, in future episodes, as the means by which the conditioned stimulus gains access to the emotional response circuits. To do this, the lateral nucleus has to communicate with the central nucleus of the amygdala, which then distributes its output to a variety of sites in the brain that mediate the various behavioral and physiological components of the fear response. Thus, lesions of the lateral or central nuclei block all fear responses elicited by the tone conditioned stimulus, but lesions of brainstem areas connected to the central nucleus only eliminate individual responses. For example, lesions of the periaqueductal gray region abolish freezing responses to the conditioned stimulus but not the increases in heart rate, blood pressure, or respiration or the adrenal steroid responses.
The conditioned fear constellation in experimental animals, involving defensive freezing and associated autonomic and endocrine responses, bears important similarity to some of the reactions observed in humans subjected to overwhelming traumatic stress. These individuals “freeze” in their lives: they become withdrawn, avoidant, and sometimes despondent. Environmental and emotional cues remind them of the traumatic event and trigger autonomic, endocrine, and behavioral responses. Loud noises, the smell of ash, the news on television, or a letter from work are sufficient to make a person who escaped from the World Trade Center or who witnessed the towers crumbling become physiologically aroused and seized with fear. This kind of response paralyzes the individual and makes the resumption of a normal life extremely difficult.
Recently, it has been shown that the pathways leading from the central nucleus of the amygdala to the brainstem that initiate defensive freezing and associated autonomic and endocrine reactions can be redirected. After being fully conditioned, the rats can be given the option of moving to another place during the occurrence of the conditioned stimulus. If they do so, the conditioned stimulus is terminated, a condition that signals that the shock will not be coming. The learning of this response requires the diversion of the flow of information leaving the lateral nucleus of the amygdala. Rather than going to the central nucleus and engaging the passive fear response, the information is sent from the lateral nucleus to the basal nucleus of the amygdala, which does not project to the brainstem but instead to motor circuits in the ventral striatum. By engaging these alternative pathways, passive fear responding is replaced with an active coping strategy. This diversion of information flow away from the central nucleus to the basal nucleus, and the learning that takes place, does not occur if the rat remains passive. It requires that the rat take action. It is “learning by doing,” a process in which the success in terminating the conditioned stimulus reinforces the action taken. When the rat shifts from passive to active coping, it is performing the neurological equivalent of “getting on with life.” This simple paradigm in laboratory rats thus offers basic scientific validation for the advice being given by political leaders.
The results of the rat study also suggest a method that may help individuals who are symptomatic after the September 11 disaster to resume somewhat normal lives. There are many conditioned stimuli in the lives of anyone traumatized by the disaster. Some who worked in the World Trade Center towers cannot even bear the thought of going to their offices again without becoming overwhelmed with fear; others will not ride the subway, and some become glued to CNN. These thoughts and activities, we speculate, reinforce activity in the pathway that leads from the lateral to the central nucleus of the amygdala to the brainstem and thus to passive fear responses, rendering the individual seemingly helpless and ultimately despondent.
One of the hallmarks of anxiety disorders is avoidance of situations that lead to the arousal of fear and anxiety. When avoidance is passive, and leads to the disruption of normal life, it is part of the disorder. The trick is to turn avoidance into a successful coping strategy, one in which thoughts and behaviors serve to terminate exposure to the conditioned stimulus but at the same time keep the individual engaged with life.
In practice, then, the approach suggested from the laboratory studies requires that patients develop strategies that enable them to “do something” whenever they are entertaining dysphoric thoughts or are avoiding necessary or meaningful activities. This may not be the time to encourage difficult tasks, such as reading a challenging novel. Instead, the goal should simply be to successfully carry out activities, especially ones that lead to pleasure or that prevent displeasure. The rats in the experiments described above did not have to perform a difficult action—they only had to move across the chamber in order to succeed in ending their conditioned stimulus. If they had been required to perform some complex task, they might have reached a state of “helplessness” before figuring out how to succeed. Hence, an individual should be asked, “Instead of watching CNN, what other shows might you watch, or what other things do you think you could do that would engage you but not be too difficult?” Similarly, if the person is dwelling on the events of September 11, it might be helpful to “step into another place” mentally by thinking about what happened the day before, the week before, or even several months before. Finally, the individual who cannot bear to go back to work should be encouraged to do something else instead but not sit at home and brood. If going to work is too painful, the person might go shopping or visit a friend. The more involved and formal procedure of instructed desensitization to the actual fearful context can be undertaken at a later time. Obviously, however, if the individual begins to habitually miss work in order to prevent the pain, the active avoidance behavior would shift from being a way of getting on with life to being part of the pathological reaction.
While psychosocial interventions, to our mind, should be the mainstay of treatment for these trauma victims, to the extent that antidepressants relieve uncontrollable dysphoric ruminations, they should also be considered as part of the therapy. One such medication, sertraline, has already been approved by the FDA for posttraumatic stress disorder (PTSD) and a second, paroxetine, was nearing approval at the time of this writing. Studies by Davidson et al. and Marshall et al. in this issue of the Journal are indicative of antidepressant efficacy in decreasing intrusive thoughts, avoidance, and hyperarousal.
We are aware that the approach suggested by the studies of fear in rats is not dramatic and may appear to simply be one of “common sense.” After all, some of what we are suggesting just involves the use of distractions: the person is asked to turn away from dysphoric thoughts by thinking about or doing something else. But it is critical to remember that PTSD is essentially a condition in which emotional learning persists in the form of memories that seize control of mental life and behavior. The basic science experiments show that the introduction of an active coping response reroutes processing from a pathway controlling dysfunctional passivity to one controlling successful engagement with the environment. As we await the results of definitive clinical trials on effective interventions, this may be as valid and powerful a guideline as we will have.