The origin of the concept of bipolar disorder is commonly traced back to the mid-1800 contributions by Falret on
la folie circulaire (“circular insanity”)
(1) and Baillarger on
la folie à double-forme (“dual-form insanity”)
(2). The continuity between these contributions and Kraepelin’s description of manic-depressive insanity
(3) has been correctly identified. One aspect, however, is usually overlooked: both Falret and Baillarger, contrary to Kraepelin, described a specific variety of bipolar disorder, i.e., the form characterized by the direct, regular transition from mania to depression or vice versa. Both of them regarded this “circular” form as distinct from those cases in which manic and depressive episodes occur separately (although Baillarger accused Falret to have originally missed, and then to have borrowed, this differentiation). Both considered this distinction as significant. Falret
(1) reported that “circular insanity is very hereditary” and “infinitely more frequent in females than in males” and stated that “mania and melancholia, when they occur in isolation, are more treatable than when they occur together in circular insanity.”
Modern generations of psychiatrists have not completely ignored Falret and Baillarger’s teaching. In fact, some scholars of manic-depressive illness have explicitly distinguished a “circular” form of the disease as having a poor prognosis
(4), whereas others have reported that the tendency to switch is a predictor of a worse outcome
(5,
6). Koukopoulos et al.
(7) found that a circular course in which depression regularly precedes mania, as well as a circular course without free intervals (“continuous circular course”), is associated with a poorer response to lithium prophylaxis. Turvey et al.
(8) reported that “polyphasic episodes” (i.e., episodes including at least two mood polarity switches) are associated with a poor prognosis, concluding that “it is more likely that patients who switch have a more severe form of bipolar disorder which manifests as affective instability.”
The literature on rapid cycling is only partially relevant to the present issue. In fact, the current definition of rapid cycling (i.e., the one proposed in DSM-IV) does not require “switching” (i.e., the direct transition from mania to depression or vice versa) as a prerequisite. Indeed, the term “cycling” is currently used in a very equivocal manner in this research area. Consider, for instance, the statement “cycling, and cycling with hypomania in particular, seemed to predispose to subsequent rapid cycling”
(9) in which the term “cycling” is first used as a synonym for “switching” and then, in the same sentence, without such a meaning. However, the tendency to switch may have significant implications for the prognosis and treatment response of patients with rapid cycling as defined by DSM-IV. In fact, rapid cyclers with a history of switching manifest a poorer response to lithium and a higher stability of the rapid-cycling pattern reported at a follow-up evaluation
(10,
11).
Thus, currently available research provides some evidence that Falret and Baillarger were actually right, i.e., that the regular switch from one mood polarity to the other may identify a variety of bipolar disorder with a characteristic prognosis, treatment response, and, perhaps, pathophysiology.
The present study approached this issue by exploring five areas. First, we sought to determine whether bipolar patients who experience at least one direct transition from one mood polarity to the other in their first prospectively observed episode (“switchers”) are different from other bipolar disorder patients (“nonswitchers”) with respect to any demographic or historical variable (including sex ratio and family history of bipolar disorder). Second, we evaluated whether the periods of abnormal mood within the first prospectively observed episode of switchers differ from those of nonswitchers with respect to any symptomatic feature. Third, we assessed whether the direct transition from one mood polarity to the other would turn out to be an occasional or a regular feature in patients initially classified as switchers after a prospective prolonged follow-up period. Fourth, we sought to determine whether the percentage of time spent in an affective episode during a prospective observation period would be significantly higher, and the long-term psychopathological and psychosocial outcome significantly worse, in switchers relative to nonswitchers. Last, we assessed among switchers whether the polarity sequence (depression followed by mania/hypomania or vice versa) and the number of switches within the first prospectively observed episode (i.e., one mood polarity switch versus more than one) have long-term prognostic implications.
Method
Subjects
The study group included all patients seen at the Centre for Affective Disorders of the First Psychiatric Department of Naples University between January 1, 1978, and December 31, 1990, who 1) fulfilled Research Diagnostic Criteria (RDC)
(12) for bipolar I or bipolar II disorder, as ascertained through use of the Schedule for Affective Disorders and Schizophrenia (SADS)
(13), administered by trained psychiatrists whose interrater reliability had been formally tested and found to be satisfactory
(14); and 2) had a first prospectively observed episode consisting of at least two periods of abnormal mood, one fulfilling criteria for mania or hypomania and the other meeting criteria for major depression (as per RDC), with an intervening period of no more than 1 month. We decided to focus on the first prospectively observed episode rather than on the episode during which each patient first came to our attention because we felt, as have other authors
(15), that the classification of a patient as a switcher or nonswitcher requires the direct observation of the entire episode. For this same reason, we gave up any attempt to identify retrospectively the presence or absence of the switching pattern in the patient’s first episode of illness.
For each enrolled switcher, we randomly recruited from the same center, during the same year (to avoid the effects of changes in treatment habits), a patient with RDC bipolar I or bipolar II disorder (as confirmed by the SADS) whose first prospectively observed episode was monophasic (i.e., consisted of a period fulfilling criteria for mania, hypomania, or major depression that was not followed within 1 month by a period of abnormal mood of the opposite polarity). This was the comparison group (“nonswitchers”).
After complete description of the study to the patients, written informed consent was obtained.
Procedures
At the time of recruitment, the following demographic and historical variables were recorded for each patient: sex, age, age at first psychiatric contact, number of prior hospitalizations in a psychiatric ward, and history of bipolar disorder in first-degree relatives (as ascertained by the Family History Research Diagnostic Criteria
[16]). In switchers, the index episode was classified by the number of mood polarity switches (one or more than one), and the polarity sequence (mania/hypomania followed by depression or vice versa) was recorded. The symptomatic features of the index episode at its peak (or of each period of abnormal mood at its peak in patients with a polyphasic index episode) were assessed by the Comprehensive Psychopathological Rating Scale
(17), administered by trained psychiatrists whose interrater reliability had been formally tested and found to be satisfactory
(14). The Comprehensive Psychopathological Rating Scale includes 28 items for depression and 10 for mania.
Starting from the time of recruitment, each patient was evaluated every second month with the Montgomery-Åsberg Depression Rating Scale and the measuring change version of the SADS. Treatment was not under the control of the researchers but was carefully recorded at each visit. New affective episodes (diagnosed as per RDC) were recorded and classified as monophasic or polyphasic (with either one or more than one mood polarity switch). In polyphasic episodes, the polarity sequence was recorded. Ten years after recruitment, all patients, whether or not they were still attending the center, were contacted for a brief interview during which the Strauss-Carpenter Outcome Scale
(18) was administered by a trained psychiatrist
(19) who was unaware of the group to which each patient belonged.
Data Analysis
Switchers and nonswitchers were compared with respect to demographic, historical, and clinical variables by using analysis of variance or the chi-square test with Yates’s correction, as appropriate.
Kaplan-Meier survival analysis was used to estimate the probability of recovery from the index episode for all patients and for 1) switchers whose index episode started with depression versus those whose index episode started with mania or hypomania and 2) switchers with a diagnosis of bipolar I versus bipolar II disorder. Differences among the above groups were explored by the log-rank test. Recovery was defined as a period of at least 8 consecutive weeks in which the mood disturbance required by criterion A for RDC mania, hypomania, or major depression was not fulfilled.
In the group of switchers, the Cohen’s kappa coefficient was used to explore the consistency between the index episode and each of the episodes recorded during the observation period with regard to the presence of the switching pattern and the polarity at the onset of the episode (depression or mania/hypomania).
Analysis of variance with arcsine transformation and Tukey’s honestly significant difference test for post hoc comparisons
(20) was used to compare the percentage of time spent in an affective episode during the observation period (whatever its duration) and among 1) switchers whose index episode started with depression versus those whose index episode started with mania or hypomania and 2) switchers with a diagnosis of bipolar I versus bipolar II disorder. Analysis of variance with Tukey’s test was also used to compare the above patient groups with respect to the mean Strauss-Carpenter Outcome Scale global score at the 10-year follow-up interview.
In the group of switchers, a regression analysis was performed to measure the simultaneous effect on the 10-year outcome (Strauss-Carpenter Outcome Scale global score) of the following variables: the polarity sequence in the index episode (depression followed by mania/hypomania or vice versa), the number of mood polarity switches within the index episode (one or more than one), and those clinical variables that in univariate analyses distinguished significantly between switchers and nonswitchers.
Results
Demographic and Historical Data and Characteristics of the Index Episode
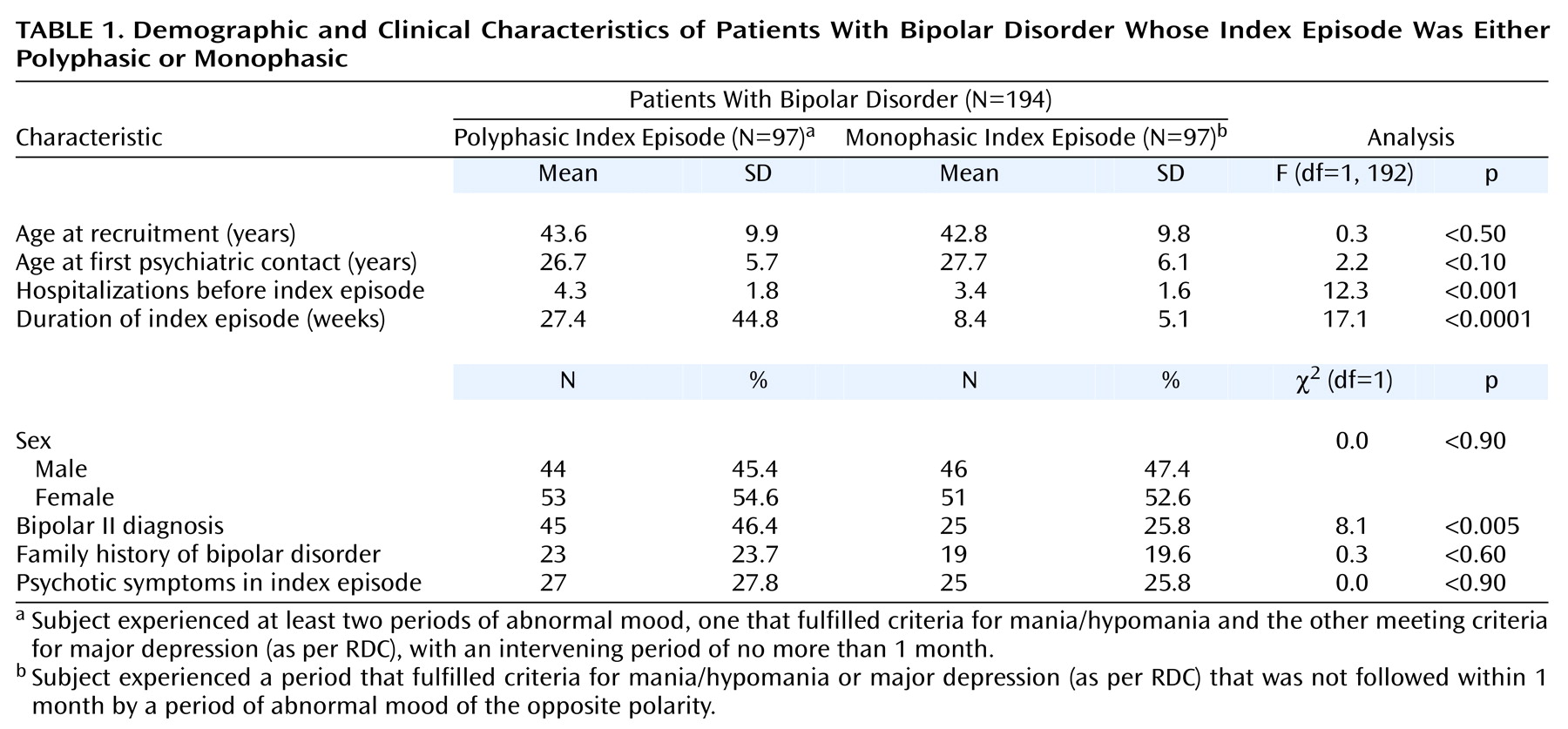
The group of switchers consisted of 97 patients (44 men and 53 women). Their mean age at the time of recruitment was 43.6 years (SD=9.9, range=19–67). Seventy-four patients (76.3%) had only one mood polarity switch, and 23 (23.7%) experienced more than one. The percentage of women was 51.4% (N=38) among patients with only one mood polarity switch and 65.2% (N=15) among those with more than one. Among patients with one mood polarity switch, the first period of abnormal mood was depressive in 33 cases (44.6%) and manic/hypomanic in 41 (55.4%). Among patients with more than one mood polarity switch, the first period of abnormal mood was depressive in 17 cases (73.9%) and manic/hypomanic in six (26.1%). Overall, the percentage of switchers whose index episode started with depression was 51.5% (N=50; 54.7% in women [N=29] and 47.7% in men [N=21]). Forty-five switchers (46.4%) had a diagnosis of bipolar II disorder. Switchers with bipolar II disorder were significantly more likely than those diagnosed with bipolar I disorder (N=52) to have an index episode starting with depression (χ2=4.7, df=1, p<0.03) but not to have an index episode with more than one mood polarity switch (χ2=0.8, df=1, p<0.40).
The group of nonswitchers consisted of 46 men and 51 women whose mean age at the time of recruitment was 42.8 years (SD=9.8, range=20–65). The index episode was depressive in 58 patients (59.8%) and manic/hypomanic in 39 (40.2%). For 32 women (62.7%) and 26 men (56.5%), the index episode was depressive. Twenty-five nonswitchers (25.8%) had a diagnosis of bipolar II disorder, a percentage that was significantly lower than that of switchers (χ2=8.1, df=1, p<0.005).
Switchers did not differ significantly from nonswitchers with respect to sex ratio, mean age at recruitment, mean age at the time of first psychiatric contact, or history of bipolar disorder in first-degree relatives. However, the mean number of hospitalizations in a psychiatric ward before the index episode was significantly higher among switchers (
Table 1). Switchers whose index episode started with depression (N=50) differed significantly from nonswitchers whose index episode was depressive (N=58) with respect to the frequency of a score of at least 2 on the Comprehensive Psychopathological Rating Scale items “slowness of movements” (54% versus 29%, respectively) (χ
2=5.8, df=1, p<0.02) and “reduced speech” (38% versus 17%) (χ
2=4.9, df=1, p<0.03). There were no further significant differences between switchers and nonswitchers with respect to the symptomatic features of the index episode.
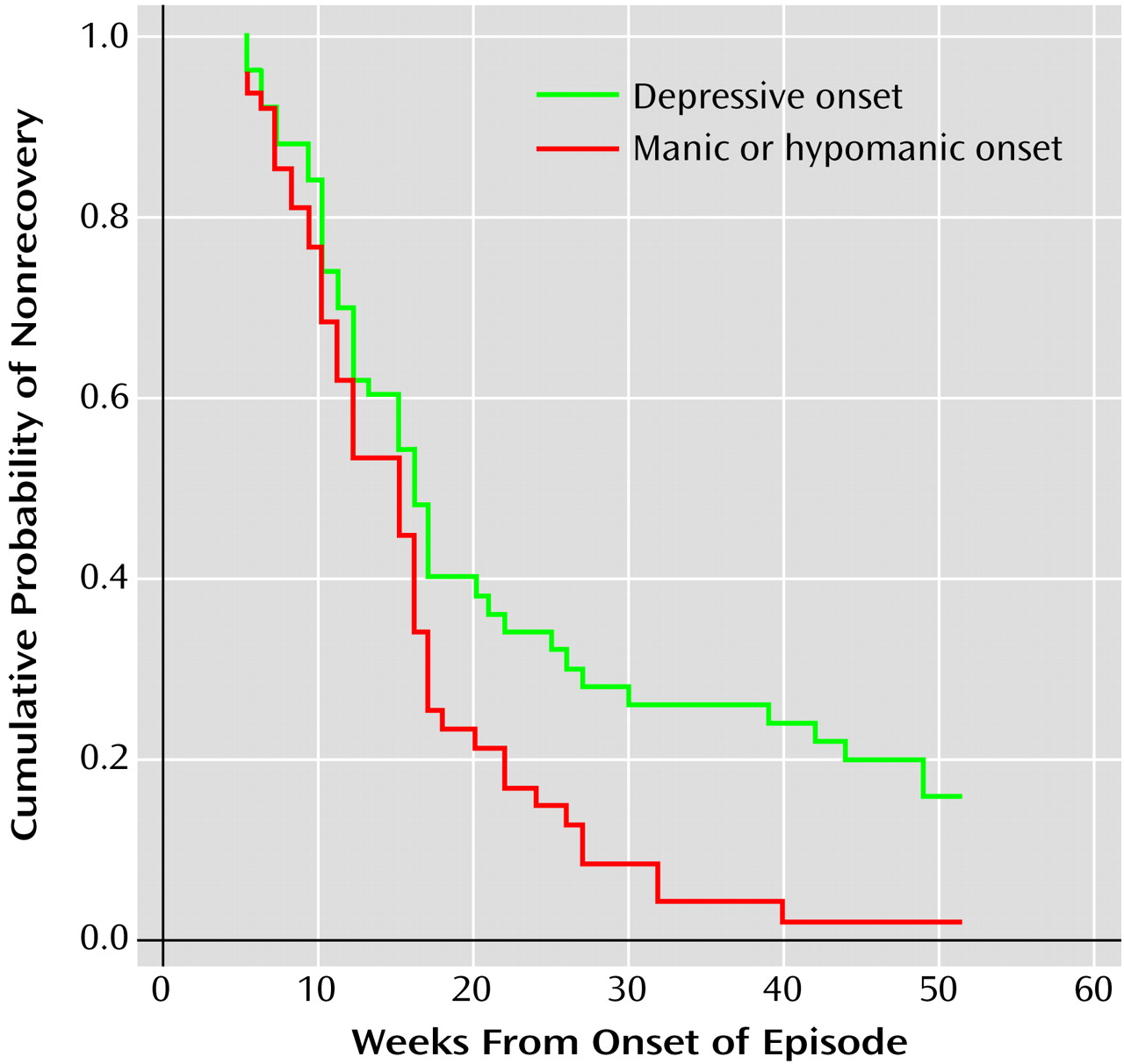
The time to 50% probability of recovery from the index episode was significantly longer in the 23 switchers with more than one mood polarity switch (44 weeks, 95% CI=33.4–54.6) than in the 74 patients who experienced only one mood polarity switch (12 weeks, 95% CI=9.8–14.2) and the 97 patients with a monophasic index episode (7 weeks, 95% CI=6.3–7.7) (log-rank=95.2, df=2, p<0.0001). The time to 50% probability of recovery from the index episode was not significantly different in switchers whose index episode started with depression (N=50) than in those whose index episode started with mania or hypomania (N=47): 16 weeks (95% CI=13.2–18.8) and 15 weeks (95% CI=11.7–18.3), respectively (log-rank=3.3, df=1, p<0.07). However, the cumulative probability of recovery at 1 year was 84% in switchers whose index episode started with depression and 98% in those whose index episode started with mania or hypomania (log-rank=6.1, df=1, p<0.01) (
Figure 1). Two patients whose polyphasic index episode started with depression recovered from that episode after 227 and 340 weeks. Among switchers, there was no significant difference between bipolar I (N=52) and bipolar II (N=45) patients with respect to the time to 50% probability of recovery (log-rank=0.01, df=1, p<0.90) or the cumulative probability of recovery at 1 year (log-rank=0, df=1, p<0.10).
Seventy-four percent (N=37 of 50) of switchers whose index episode started with depression and 81% (N=47 of 58) of nonswitchers whose index episode was depressive were treated with tricyclic antidepressants. The average peak dose of the tricyclic did not differ significantly between switchers and nonswitchers: 114.2 mg/day (SD=45.5) and 112.2 mg/day (SD=47.4) in imipramine equivalents, respectively (F=0.04, df=1, 82, p<0.80). Among the switchers whose index episode started with mania or hypomania and the nonswitchers whose index episode was manic or hypomanic, 44.7% (N=21 of 47) and 48.7% (N=19 of 39), respectively, were treated with antipsychotics. The average peak antipsychotic dose (in chlorpromazine equivalents) did not differ significantly between the two groups: 242.8 mg/day (SD=50.7) and 215.8 mg/day (SD=52.8) (F=2.7, df=1, 38, p<0.10).
Morbidity During the Observation Period
We were able to evaluate all enrolled patients every second month for at least 3 years, and 78.3% (N=76) of switchers and 80.4% (N=78) of nonswitchers for the entire period of 10 years. During the observation period, 88.6% of switchers and 85.6% of nonswitchers received at least one mood stabilizer for at least 75% of the time. Among lithium-treated patients, the serum lithium levels during the observation period were not significantly different in switchers and nonswitchers (mean=0.62 [SD=0.03] and 0.63 [SD=0.04] mmol/liter, respectively; F=0.03, df=1, 175, p<0.90).
In the group of switchers, 79 patients (81.4%) had at least one additional affective episode during the prospective observation period, 63 (64.9%) had at least two more episodes, and 41 (42.3%) had at least three more episodes. Of those patients who had at least one additional episode, 44 (55.7%) remained switchers throughout the observation period; this was true for 65.2% (30 of 46) of switchers whose index episode had started with depression and for 42.4% (N=14 of 33) of those whose index episode had started with mania or hypomania. The Cohen’s kappa coefficient measuring the consistency of the presence of the switching pattern during the observation period ranged from 0.21 to 0.35. Among patients initially classified as nonswitchers who had at least one additional affective episode, 84.9% (N=62 of 73) retained the nonswitching pattern throughout the observation period.
Of the switchers whose index episode had started with depression and who had at least one further episode during the observation period, 60.9% (N=28 of 46) had only episodes starting with depression. Of the switchers whose index episode had started with mania or hypomania, 69.7% (N=23 of 33) had only episodes starting with mania or hypomania. The Cohen’s kappa coefficient measuring the consistency of the polarity at onset of episodes ranged from 0.51 to 0.65.
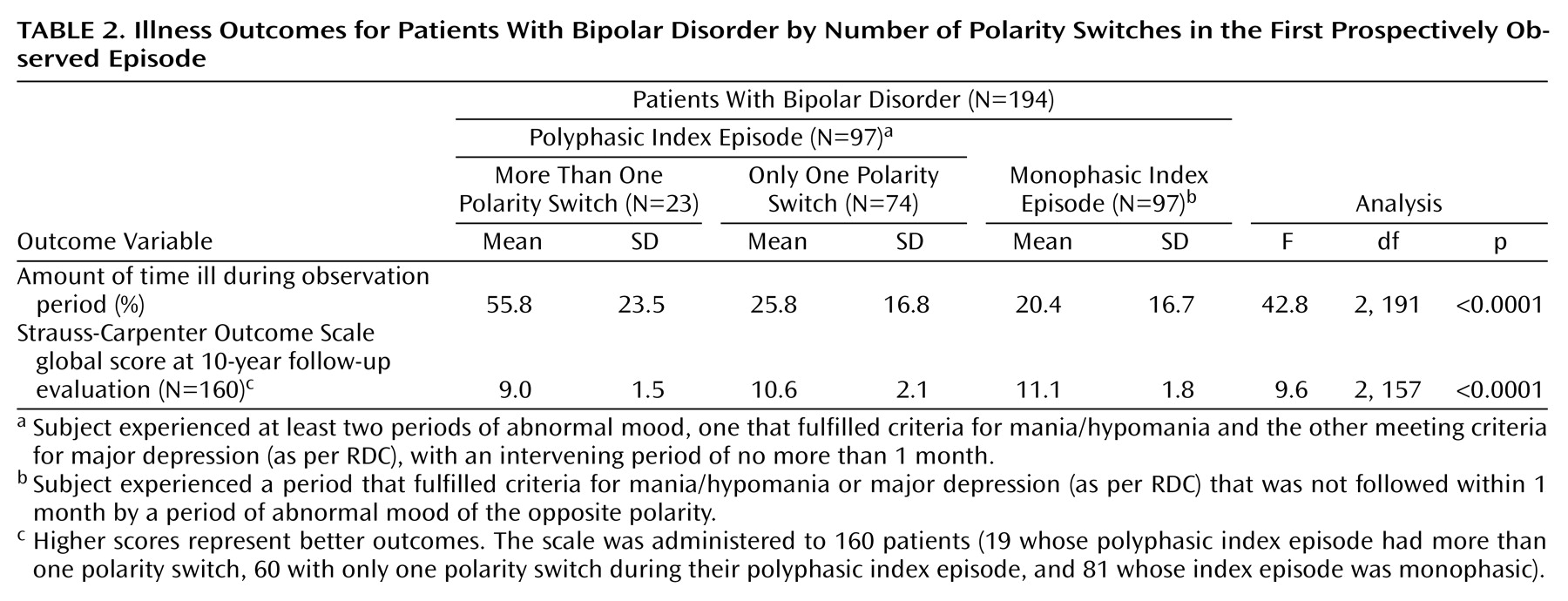
Switchers who had more than one mood polarity switch during the index episode were in an affective episode during the observation period for a significantly higher percentage of time than were switchers with only one mood polarity switch and nonswitchers (
Table 2). During the observation period, the time spent in an affective episode was significantly longer for the 50 switchers whose index episode had started with depression (41.3%, SD=23.4) than for the 47 switchers whose index episode had started with mania or hypomania (24.0%, SD=17.7) (F=16.4, df=1, 95, p<0.0001). Patients whose index episode included at least two mood polarity switches and started with depression were affectively ill for 59.6% of the observation period. Among the switchers, there was no significant difference in the percentage of time spent in an affective episode during the observation period for the 52 patients with bipolar I disorder (31.7%, SD=24.3%) and the 45 patients with bipolar II disorder (34.3%, SD=20.4%) (F=0.20, df=1, 95, p<0.60).
Follow-Up Interview Data
A 10-year follow-up interview was obtained for 79 (81.4%) of the switchers, including 81.1% (N=60 of 74) of those with only one mood polarity switch during the index episode and 82.6% (N=19 of 23) of those with more than one. Eighty-one (83.5%) of the nonswitchers were seen at the 10-year follow-up evaluation. Among both switchers and nonswitchers, patients lost to follow-up did not differ significantly from the others with respect to the percentage of time spent in an affective episode during the observation period.
The mean Strauss-Carpenter Outcome Scale global score was significantly lower (i.e., the outcome was worse) in switchers with more than one mood polarity switch than in those with only one switch and nonswitchers (
Table 2). Of note, 15 (19.0%) of the switchers had a score of 0 on the “employment” subscale, i.e., performed “no useful work” (including work as housewife or student) during the year preceding the follow-up interview. A significantly lower mean Strauss-Carpenter Outcome Scale global score was seen in the 44 switchers whose index episode had started with depression (mean=9.5, SD=1.9) than in the 35 switchers whose index episode had started with mania or hypomania (mean=11.1, SD=2.0) (F=13.5, df=1, 77, p<0.0001). Among switchers, the mean Strauss-Carpenter Outcome Scale global score was not significantly different in the 44 patients with bipolar I disorder (mean=10.4, SD=1.8) and the 35 with bipolar II disorder (mean=10.0, SD=2.3) (F=0.7, df=1, 77, p<0.40).
The regression analysis performed in the group of switchers included, besides the polarity sequence and the number of switches in the index episode, the following independent variables (which in univariate analyses distinguished significantly between switchers and nonswitchers): number of hospitalizations before the index episode, duration of the index episode, and diagnosis of bipolar I versus bipolar II disorder. The analysis revealed that a worse 10-year global outcome was predicted by an index episode starting with depression (standardized beta coefficient=0.36, SE=0.46, p<0.002) and more than one mood polarity switch in the index episode (standardized beta coefficient=0.25, SE=0.51, p<0.02) (model F=6.7, df=5, 73, p<0.0001; R2=0.21).
Discussion
Although Falret
(1) and Baillarger
(2) regarded “switching” (i.e., the direct transition from one polarity of mood to the other) as the key feature of circular/dual-form insanity, this aspect has been surprisingly neglected in clinical research on bipolar disorder. In the few studies in which it has been a focus of attention, however, switching has been almost invariably found to be a predictor of poor outcome. Of note, studies in the prelithium era
(4,
21,
22) reported that a poor prognosis was associated with switching per se, whereas studies carried out after the introduction of lithium
(7,
8) specified that a poor outcome was associated with the switch from depression to mania. This may reflect the strong antimanic effect of lithium, which may have improved the outcome of those patients in whom mania preceded depression
(7), as well as the unavailability of a mood stabilizer that is able to exert its action “from below”
(23), that is, acting primarily on depression. Studies reporting the efficacy of lamotrigine in bipolar depression
(24) have emphasized that this drug is not likely to “induce” a switch to mania or hypomania but have not explored whether it is able to “prevent” a switch in patients with a history of polyphasic episodes in which depression precedes mania.
Our study confirmed that poor outcome is mainly associated with the pattern described by Koukopoulos et al.
(7) as “continuous circular course” and by Turvey et al.
(8) as “polyphasic episode,” i.e., a pattern marked by at least two mood polarity switches during the same episode, especially if the first period of abnormal mood is depressive. A patient whose first prospectively observed episode includes more than one mood polarity switch and starts with a period of depression is likely to spend more than half of his or her life in an affective episode, in spite of state-of-the-art treatment. It is clear that this subtype of bipolar disorder represents an important target for new pharmacological and psychosocial treatment strategies.
Switching is no longer the constant feature of the illness course that Falret and Baillarger described in the mid-1800s. Only 55.7% of our patients who were initially classified as switchers and had at least one additional episode during the prospective observation period remained switchers throughout that period. This is likely to be, at least in part, a consequence of prophylactic treatment. It is noteworthy, in this respect, that the switching pattern was retained throughout the observation period by 42.4% of patients whose index episode had started with mania or hypomania and 65.2% of those whose index episode had started with depression. This points again to the higher effectiveness of currently available mood stabilizers in interrupting the cycle initiated by mania than that started by depression. On the other hand, it is possible that part of the switches from depression to mania/hypomania were induced by antidepressant treatment
(7). In our study group, however, as in that studied by Turvey et al.
(15), patients with a polyphasic index episode that started with depression did not receive tricyclic antidepressants more frequently than did nonswitchers whose index episode was depressive, nor was the average peak tricyclic dose significantly higher in the former group.
Our observation that the phenomenology of depression in switchers is in some respects different from that in nonswitchers may be of interest. Slowness of movements and reduced speech were among the clinical features emphasized by Bunney et al.
(25) in their description of the depressive phase in bipolar patients who switched, and it has been hypothesized that manic-depressive illness with a circular course is predominantly a disorder of energy or activation
(26,
27). The higher frequency of the bipolar II pattern among switchers, in particular those in whom the cycle is initiated by depression, is also in line with previous reports
(7,
26).
According to Turvey et al.
(8), switching characterizes a particularly severe variety of bipolar disorder in which the mechanism of mood regulation is so impaired that it “repeatedly overshoots its mark when approaching euthymia.” On the other hand, Koukopoulos et al.
(7) maintained that a circular course is a common feature of bipolar disorder, although in several cases part of the cycle remains at a subclinical level. Further research is clearly needed to explore this issue. It is desirable that the switch process, one of the most striking clinical phenomena of the entire field of psychiatry, become again a focus of attention for biological research, as it was in the early 1970s.