One of two community surveys of body dysmorphic disorder
(1,
2) was in a city renowned for its art (Florence, Italy)
(1). A cognitive behavior model of body dysmorphic disorder has proposed that these patients have idealized values about the importance of appearance and that some may also value perfectionism
(3). The aim of the current preliminary study was to investigate whether the interest of patients with body dysmorphic disorder in aesthetics would be manifested in their occupation, training, or higher education. We hypothesized that patients with body dysmorphic disorder are more likely to have an occupation or education in art and design than patients with other psychiatric disorders.
Method
The occupation and education of 100 consecutive patients at first presentation with the diagnosis of body dysmorphic disorder were compared with the occupation and education of 100 consecutive patients with a major depressive episode, 100 consecutive patients with a diagnosis of posttraumatic stress disorder (PTSD), and 100 consecutive patients with obsessive-compulsive disorder (OCD). All participants were outpatients in a private psychiatric hospital from 1996 onward.
Most of the patients were funded privately; a minority were funded by the National Health Service or had research assessments. The primary diagnosis was used to select the patient groups and the main focus of treatment. The most common comorbid diagnoses among patients with body dysmorphic disorder were delusional disorder (52%), major depressive episode (26%), and social phobia (20%). All of these patients were being treated primarily for body dysmorphic disorder. Comorbid diagnoses among the patients with major depressive episode were dysthymia (7%) and generalized anxiety disorder (6%). The one comorbid diagnosis among the patients with OCD was major depressive episode (16%). Comorbid diagnoses among the patients with PTSD were major depressive episode (15%) and dysthymia (3%). The diagnoses were made according to DSM-IV but without a structured diagnostic interview schedule.
The comparison groups represent the most common diagnoses seen for routine psychiatric assessment. The case notes were examined retrospectively, and there was no test of diagnostic reliability. Information on the individual’s occupation, higher education, and training was extracted from a questionnaire that was completed by all patients. Patients were asked details regarding their occupational history as well as any higher education or training received.
An individual was defined as an artist if he or she had, at any time, either education or training in art, fine art, art history, or design or an occupation as an artist, an art teacher, an architect, or a graphics, fashion, or textile designer. Both current and past occupation, training, or higher education in art and design were used to classify a patient. For example, a patient who had a degree in fine art but was working as a waiter was classified as an artist.
Results
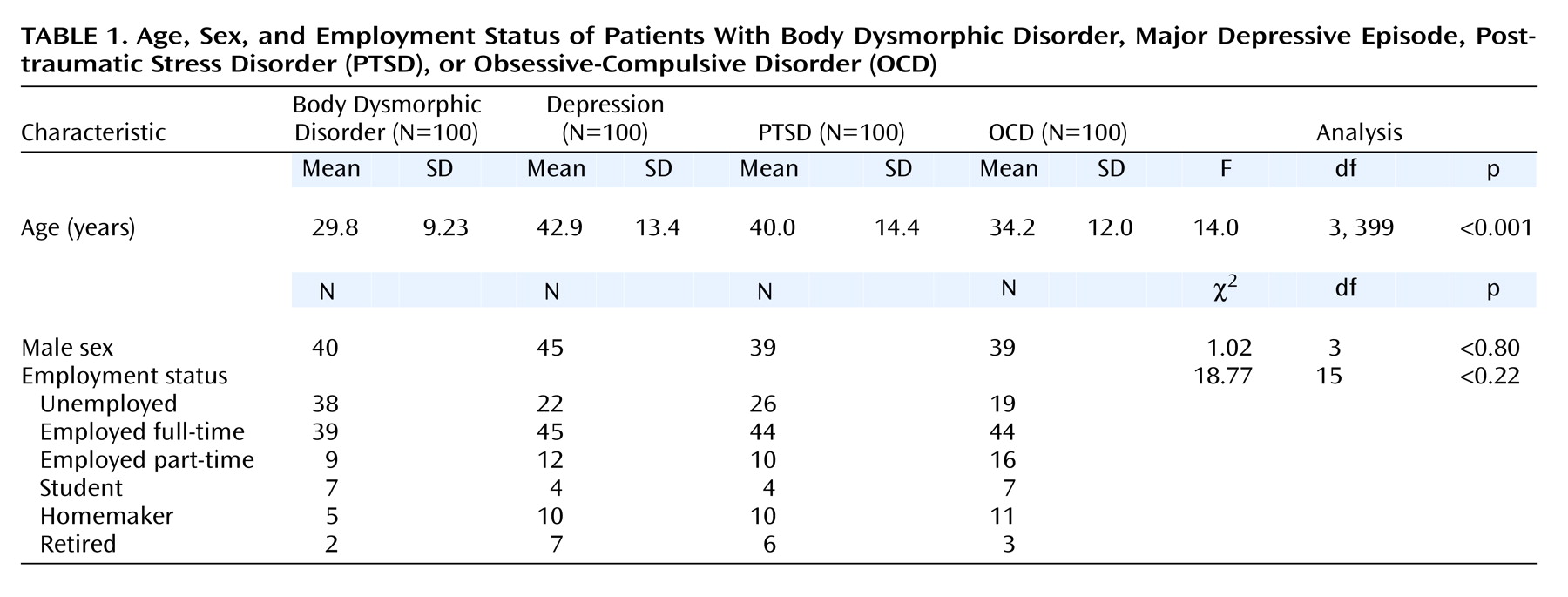
Data on the age, sex, and employment status of patients in the four groups are given in
Table 1. The groups were matched according to sex but not according to age. The patients with body dysmorphic disorder were significantly younger than the patients in all three comparison groups, and the patients with OCD were significantly younger than those with PTSD and those with major depressive episode.
Twenty percent of the patients with body dysmorphic disorder had an occupation or education in art or design (four graphic design, two architecture, two fine art degree, five art history degree, six art and design degree, one artist). In contrast, 4% of the depressed patients (one fine art degree, one art history degree, one artist, one art teacher), 0% of the PTSD patients, and 3% of the OCD patients (one graphic design, one architecture, one fine art degree) had such occupations or training (χ2=38.6, df=3, p<0.001).
The patients with body dysmorphic disorder were significantly more likely to have an occupation or education in art and design than patients with major depressive episode (χ2=12.12, df=1, p<0.001), patients with PTSD (χ2=22.22, df=1, p<0.001), and patients with OCD (χ2=14.20, df=1, p<0.001). There were no significant differences among the three comparison groups except that patients with major depressive episode were significantly more likely to have an occupation or education in art and design than those with PTSD (4% versus 0%). (χ2=4.08, df=1, p<0.04).
Discussion
To our knowledge, no occupational or educational association has been identified previously in patients with body dysmorphic disorder. Our findings reveal a possible association between body dysmorphic disorder and an interest in art or design. The differences between the body dysmorphic disorder group and the three comparison groups were relatively large, and the rates in the three comparison groups were similar, suggesting that the association is worth investigating further.
Individuals in certain occupations are at a greater risk of developing a psychiatric disorder; for example, firefighters are more likely to develop PTSD and ballet dancers are more likely to have eating disorders. However, we know of no psychiatric disorder that has an association with a particular occupation except one study
(4), which found that patients with schizophrenia were more likely to select occupations with a low potential for arousal (e.g., janitors).
We do not have any evidence for a causal relationship between body dysmorphic disorder and interest in art and design. Nor are we able with these data to determine whether the interest was acquired before or after the onset of body dysmorphic disorder. The onset of this disorder is usually gradual during adolescence, and an interest in art may be a contributory factor to its development in some patients. Patients might develop a more critical eye and appreciation of aesthetics, which are then applied to their own appearance. An equally plausible explanation is that patients with body dysmorphic disorder tend to have an interest in aesthetics.
The association raises an interesting question about the definition of body dysmorphic disorder as a preoccupation with an imagined defect. Patients with body dysmorphic disorder might have higher aesthetic standards than the mental health professionals who diagnose them, who may not appreciate beauty to the same degree. Harris
(5) has proposed that individuals seeking cosmetic surgery are more aesthetically sensitive (an attribute like being musical, which varies in different individuals). Another explanation is that patients with body dysmorphic disorder have idealized values about the importance of appearance and aesthetics, which have become overidentified with the “self”
(3).
A significant limitation of the present study was the relatively small number of subjects in the study groups, which may have led to a selection bias. A larger prospective study is required in a community sample matched according to age, sex, and parental social class to confirm our findings and to determine whether the interest in art occurred before the onset of body dysmorphic disorder. It would also be interesting to know if art or design is associated with specific areas of “imagined” defects. However, it will also be necessary to disconfirm our findings with other broad groupings of occupation (e.g., health care professionals).
If the association between body dysmorphic disorder and an interest in art and design is truly positive, then it raises an intriguing question—if we encouraged our patients with body dysmorphic disorder who do not have an education in art and design to take up such an interest, would it help focus their attention away from their appearance or would it make their preoccupation worse? Alternatively, should we be discouraging patients with body dysmorphic disorder with an interest in art from such pursuits?