In 1968 Grinker et al.
(1) conducted a factor analytic study of the symptoms of 53 patients who were thought to conform to the borderline personality disorder patient type and defined 14 factors that were used to cluster the patients into four different groups ranging from neurotic to psychotic. Their effort was the first to bring an empirical order to the constellation of symptoms belonging to a diverse group of patients who were perhaps most singularly known for being difficult to treat. Since that time much work has gone into refining the borderline personality disorder construct. Among the more notable revisions, an attempt was made to cleave the psychotic end from the category with the introduction of schizotypal personality disorder into DSM-III in 1980. Despite the narrowing of the definition, however, the borderline personality disorder category applies to a relatively heterogeneous population.
As is the case with the criteria for many of the axis II disorders
(2), the criteria for borderline personality disorder are themselves heterogeneous, consisting of an admixture of personality traits, symptomatic behaviors, and symptoms
(3). This may in part reflect the varying conceptualizations of the disorder. For instance, some have argued that it is a variant of affective disorder
(4), while others maintain that the disorder centers around developmental insults to personality formation
(5). It may be the case that borderline personality disorder is a complex disorder with various manifestations and multiple etiologies.
High rates of co-occurring axis I and axis II disorders found in those with borderline personality disorder are well documented
(6) and illustrate the heterogeneity among those with the diagnosis. Consideration of the DSM-IV diagnostic decision rules for borderline personality disorder underscores this point. Given that meeting any five of the nine criteria qualifies a person for the borderline personality disorder diagnosis, there are 151 different combinations of criteria from which it is possible to achieve borderline personality disorder status.
In light of these complexities, a better understanding of the components of the disorder is one way to develop treatment formulations, gauge change, and study its etiology. Factor analysis provides an empirical method for identifying latent variables or constructs implied by the psychiatric diagnosis. We are aware of four factor analytic studies of borderline personality disorder that have appeared since the introduction of DSM-III. One study
(7) examined DSM-III criteria, two
(8,
9) examined DSM-III-R criteria, and one
(10) looked at DSM-IV criteria for borderline personality disorder.
Rosenberger and Miller
(7) studied the DSM-III criteria for borderline personality disorder in a group of 106 college undergraduates. In their study, clinicians rated patients on the criteria on the basis of a review of information from the Structured Interview for DSM-III Personality Disorders
(11), the Diagnostic Interview for Borderline Patients
(12), and a modified version of the Schedule for Affective Disorders and Schizophrenia—Lifetime Version
(13). Factor analyses of these ratings suggested one factor that consisted primarily of interpersonal and identity criteria and a second factor that consisted of the regulation of behavior and affect. Although the subjects in the study by Rosenberger and Miller
(7) were selected on the basis of extreme scores on several screening instruments for psychiatric symptoms, the study group was nonclinical, only in moderate distress, and of limited age range.
Clarkin and colleagues
(8) conducted a factor analysis of the DSM-III-R criteria for borderline personality disorder that were assessed by using an expanded version of the Structured Clinical Interview for Axis II Personality Disorders (SCID-II)
(14) in a group of 75 inpatient women. They identified three factors: problematic interpersonal relationships and identity, an affective dimension including suicidality, and impulsivity. However, there was some overlap in these factors. Labile affect (from the second factor) also loaded on the first factor, and unstable relationships (from the first factor) also loaded on the second factor. The impulsivity criterion stood alone as the third factor (although labile affect negatively loaded on this factor). The lack of clarity in these results may have been due partly to the small group size, its acuity, or possibly the homogeneity of the study group (i.e., all subjects were inpatient women, and all met the criteria for borderline personality disorder, thus limiting variation in the distribution of positive criteria).
We recently reported a three-factor solution for the DSM-III-R criteria for borderline personality disorder
(9), using ratings obtained from the Personality Disorder Examination
(15) in an acutely ill impatient study group. The first factor, labeled “disturbed relatedness,” consisted of the following criteria: unstable relationships (DSM-III-R criterion number 1), identity disturbance (number 6), and chronic feelings of emptiness (number 7). This factor, reflecting a disturbed sense of self and relatedness to others, might be viewed as a key aspect of borderline personality disorder in that these features might be seen as underpinning much of the symptomatic interpersonal behavior common in patients with borderline personality disorder. The second factor, “behavioral dysregulation,” consisted of criteria for impulsivity (number 2) and suicidality or self-mutilative behavior (number 5). It captured the most treatment-relevant symptomatic behavior of an individual with borderline personality disorder and differed from the other factors in the sense that the criteria that it comprised were behaviors as opposed to symptoms, character traits, or temperaments. The third factor, “affective dysregulation,” consisted of criteria for affective instability (number 3), inappropriate anger (number 4), and avoidance of abandonment (number 8). It is suggestive of the physiological temperament of persons with borderline personality disorder
(16,
17) and might be seen as a diathesis for the disorder by compromising an individual’s ability to moderate his or her response to stress. One limitation of our prior report was the acuity of our study group, thus those results may not be generalizable to less disturbed populations.
A limitation of all of the studies cited is that exploratory factor analysis was used. Methodological advances have made confirmatory tests of covariance structures possible by using structural equation modeling techniques to perform confirmatory factor analysis
(18). In contrast to exploratory factor analysis, confirmatory factor analysis offers the advantage of statistical tests for goodness of fit for the resulting factor structures, thus providing a more definitive evaluation of latent variables, or constructs. Confirmatory factor analysis mathematically specifies predictions about the relationships among observed variables on the basis of the hypothetical constructs they are purported to measure. If model-implied covariances correspond with observed covariances, then hypothetical constructs are supported
(19).
Fossati and colleagues’ study
(10) was the only work that we could locate that used confirmatory factor analysis to examine the construct of borderline personality disorder. Their study group of 564 outpatients was diagnosed by means of version 2.0 of the SCID-II. In contrast to the exploratory factor-analytic studies already reviewed
(7–
9), the Fossati et al.
(10) findings, obtained by using the SCID-II, were generally consistent with the concept of borderline personality disorder reflecting a unidimensional or singular construct, thus supporting the DSM-IV borderline personality disorder diagnosis. Fossati et al.
(10), however, noted that such homogeneity does not rule out natural subgroups and that their results suggested a possible dimensional gradient involving impulsivity and anger dyscontrol that stood apart from the overall construct of borderline personality disorder.
How best to conceptualize the construct may also depend on the nature of the study group. For instance, in less disturbed study groups, such as psychiatric outpatients, borderline personality disorder as a unitary construct may be most parsimonious. In more acutely disturbed populations, there may be greater utility in clarifying the components of the disorder (e.g., to provide a framework for treatment planning
[3]). More generally, identifying robust components of the disorder and understanding how they may vary in different populations (or individuals) is important for taxonomic and clinical reasons. How is it that the admixture of criteria fit together within this complex diagnosis? How can the heterogeneity of borderline personality disorder (i.e., with varying levels of co-occurrence with other psychiatric disorders) be explained? Are certain components more responsive to treatment, while others more stable and seemingly less so? Factor analytic studies provide a base from which to attempt to answer these questions by breaking out empirically and evaluating the validity of components.
We sought to test two models on the basis of the criteria for DSM-IV borderline personality disorder. First, we were interested in testing the construct of borderline personality disorder as a unitary construct. Second, we sought to replicate the three-factor model (of disturbed relatedness, behavioral dysregulation, and affective dysregulation) that we had previously identified
(9). To accomplish these goals, we analyzed the DSM-IV criteria for borderline personality disorder that we had obtained from a semistructured clinical interview, the Diagnostic Interview for DSM-IV Personality Disorders
(20). This diagnostic information was obtained from baseline assessments and blind reassessments after 2 years in a group of primarily treatment-seeking personality-disordered subjects who were recruited as part of a multisite longitudinal study of personality disorders
(21).
Method
Subjects
Study subjects aged 18–45 years were evaluated as part of a prospective, repeated measures project to examine the longitudinal course of personality disorders
(21). To obtain a full range of personality pathology, primarily treatment-seeking subjects at both inpatient and outpatient facilities were recruited for studies of four representative personality disorders (borderline, schizotypal, avoidant, and obsessive-compulsive), along with a comparison group that met criteria for major depressive disorder but not personality disorder. The study group was supplemented by subjects responding to postings or media advertising for an interview study of personality who were currently seeking or receiving psychiatric treatment or psychotherapy or who had recently been in psychiatric treatment or psychotherapy. Potential subjects were prescreened to determine age eligibility and treatment status and to assist in excluding subjects with active psychosis, acute substance intoxication or withdrawal, a history of schizophrenia spectrum psychosis (i.e., schizophrenia, schizophreniform, or schizoaffective disorders), or organicity. All eligible subjects who began the assessment signed written informed consent after the research procedures had been fully explained. The final study group was composed of 668 subjects. A total of 64% were women; 76% were Caucasian, 11% were African American, 9% were Hispanic, and the remaining were of other ethnic backgrounds
(21).
Procedure
Extensively trained research interviewers with master’s or doctoral degrees conducted baseline assessments. The subjects were reassessed 2 years later by reliably trained interviewers who were blind to baseline findings and diagnoses. The Diagnostic Interview for DSM-IV Personality Disorders
(20) was among the assessments conducted at baseline and at the 2-year follow-up. The Diagnostic Interview for DSM-IV Personality Disorders is a semistructured diagnostic interview with several questions pertaining to each DSM-IV axis II criterion. Each criterion is scored as 0 for absent, 1 for present but of uncertain clinical significance, or 2 for present and clinically significant. A diagnosis is given when there are enough criteria scored at 2 (e.g., five criteria for borderline personality disorder); features for a disorder are provided in cases in which a subject falls one criterion short of a diagnosis (e.g., four criteria for borderline personality disorder). For interrater reliability, median kappa coefficients
(22) ranged from 0.58 to 1.0 for all axis II personality disorders; the median kappa for borderline personality disorder was 0.68
(23). The median kappa for 1-week test-retest reliability for all personality disorders was 0.69; the median test-retest kappa for borderline personality disorder was 0.69. In addition, the median Pearson’s r for interrater reliability for the sum total of the criteria for borderline personality disorder was 0.90 (df=83, p<0.001)
(23).
Factor Analysis
Version 4.0 of the Analysis of Moment Structures software
(24) was used to conduct confirmatory factor analysis. All subjects (i.e., with and without borderline personality disorder) were included in the analyses to maximize item variability. To evaluate for possible discontinuities in the criteria data, we examined the skewness of each of the nine symptoms of borderline personality disorder at baseline and 2 years later. At baseline the mean skewness value was 0.30 (SD=0.20), and at the 2-year assessment, the mean was 0.69 (SD=0.49), suggesting that the symptom data were not unduly skewed.
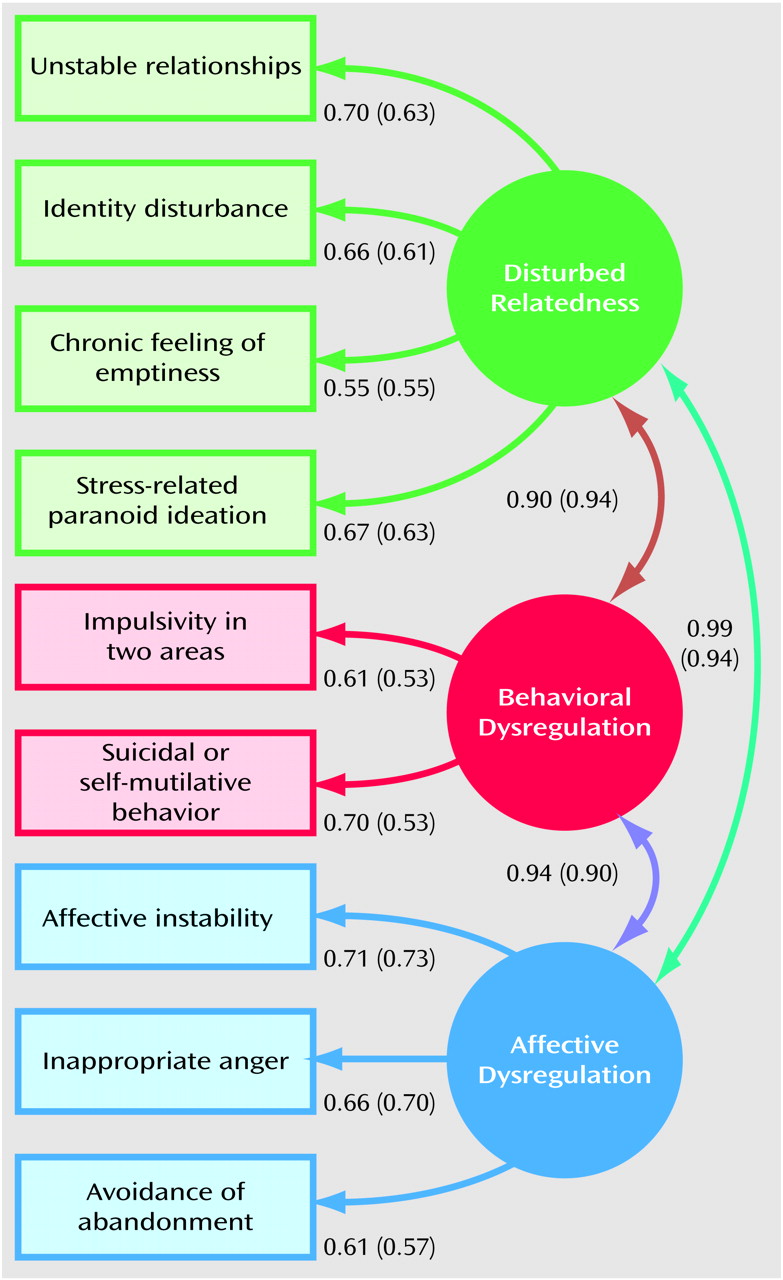
Three latent constructs—disturbed relatedness, behavioral dysregulation, and affective dysregulation—were implied by the three-factor model
(9). Affective instability, inappropriate anger, and avoidance of abandonment were specified for affect dysregulation, and impulsivity and suicidal or self-mutilative behavior were assigned to behavioral dysregulation. The disturbed relatedness factor included unstable relationships, identity disturbance, chronic feeling of emptiness, and stress-related paranoid ideation (we hypothesized stress-related paranoid ideation to be fundamentally related to the disturbed relatedness factor). For all models we specified independence of error terms, and for the three-factor models, we allowed the factors to be correlated. We used multiple fit indices to more fully evaluate the various models. Included were the comparative fit index
(25), the normed fit index
(25), and the root mean square error of approximation
(26). The comparative fit index and the normed fit index both measure the fit of the model relative the null model, but the comparative fit index is less affected by study group size
(19). The root mean square error of approximation was included because it accounts for model parsimony (i.e., goodness of fit values can sometimes be inflated artificially as the number of parameters to the model are increased). Values for the normed fit index and the comparative fit index range from 0 (poor fit) to 1 (good fit). For the normed fit index and comparative fit index, values greater than 0.90 indicate good fit
(19), whereas for root mean square error of approximation, values less than 0.08 indicate an acceptable fit
(27). Chi-square indices of fit were also included, mainly to provide a means of testing the statistical significance between nested models.
Results
Of the 668 subjects assessed at baseline, 240 (36.0%) met the full criteria for borderline personality disorder on the Diagnostic Interview for DSM-IV Personality Disorders. Of these, 175 (72.9%) were women. There were no differences in age or other demographic variables between the group with a borderline personality disorder diagnosis and the rest of the study group.
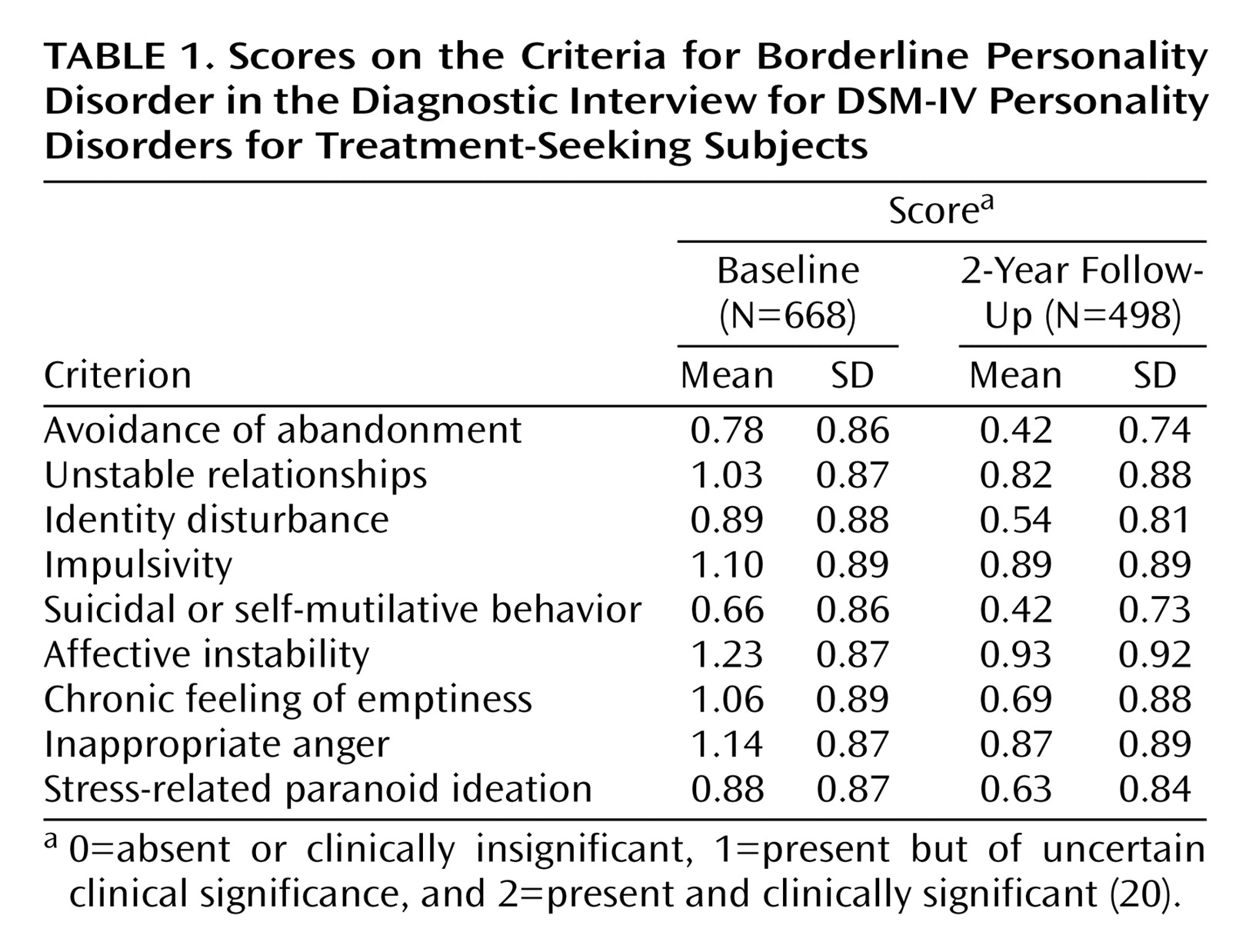
Table 1 shows the mean scores and standard deviations for each of the symptom criteria. Internal consistency was adequate, as measured by a Cronbach’s alpha of 0.86
(28), and intercriterion correlations were all significant at the p<0.01 level and ranged from 0.29 to 0.51. Certain criteria had uniformly higher correlation with the other criteria (e.g., number 8, inappropriate anger), while others (number 7, chronic feeling of emptiness) demonstrated a lower pattern of correlation with other criteria.
Fit estimates for the one-factor model were good (normed fit index=0.947, comparative fit index=0.960, root mean square error of approximation=0.066), lending further support to the diagnosis of borderline personality disorder as a unitary construct. Factor loadings were evenly distributed, ranging from 0.61 to 0.71. We next examined the three-factor model to test the fit of the previously reported model
(9), which was based on the following three factors: disturbed relatedness, behavioral dysregulation, and affective dysregulation. The results indicated that the three-factor model also provided acceptable fit for the data (normed fit index=0.951, comparative fit index=0.963, root mean square error of approximation=0.067) (
Figure 1). Although the fit indices were uniformly high for both models, a chi-square test for significant differences indicated that the three-factor model fit significantly better than the one-factor model (χ
2=8.1, df=3, p<0.05). Factor loadings ranged from 0.55 to 0.67 for disturbed relatedness, from 0.61 to 0.70 for behavioral dysregulation, and 0.61 to 0.71 for affective dysregulation.
We attempted to replicate the three-factor structure, this time by fitting it to follow-up data obtained for a large portion of our study group (N=498) 2 years after the baseline assessment with the Diagnostic Interview for DSM-IV Personality Disorders by interviewers who were blind to baseline diagnoses. Means and standard deviations for the criteria for borderline personality disorder from the Diagnostic Interview for DSM-IV Personality Disorders for this group are shown in
Table 1. Cronbach’s alpha for the diagnosis of borderline personality disorder was an acceptable 0.83, and the patterning of correlation coefficients was nearly identical to that obtained at the baseline assessment (r=0.29 to 0.51, all significant at p<0.01). For the test of the three-factor model, fit indices were good (normed fit index=0.926, comparative fit index=0.945, root mean square error of approximation=0.074), thus providing further support for the three-factor model (
Figure 1).
Discussion
Confirmatory factor analysis was used to examine the DSM-IV diagnosis for borderline personality disorder. We tested a one-factor (diagnosis as the latent construct) and a previously reported three-factor model on the basis of three components: disturbed relatedness, behavioral dysregulation, and affective dysregulation
(9). The three-factor model was then replicated by using data from a follow-up assessment of our study group conducted by interviewers who were blind to baseline diagnosis. In addition to testing the one-factor model corresponding to the DSM-IV diagnosis for borderline personality disorder, we also examined the reliability and intercorrelations of the criteria. These results, along with those from the test of the unitary model, statistically supported the diagnostic construct of borderline personality disorder. Support for the three-factor model was provided by a significantly better fit to the data than in the unitary model. The three-factor model was strengthened by its replication with data from the follow-up assessment.
Results from the confirmatory factor analysis for both the unitary and three-factor models both fit well statistically. In addition to the significantly improved degree of fit acquired with the three-factor model over the unitary model, the replication of the three-factor model in two independently conducted assessments strengthened support for understanding borderline personality disorder in terms of three components. However, we concur with other researchers who have warned against overreliance on indices of fit in the absence of theoretical or conceptual reasoning
(29). In addition to the good fit indicated by our confirmatory tests, the three-factor model is also supported on the conceptual basis that three different classes of criteria are comprised by borderline personality disorder (personality traits, symptomatic behaviors, and symptoms). These findings outline components of borderline personality disorder that may exhibit differential stability
(30) or etiologic processes
(31) and inform treatment formulations
(32). Thus, the three-factor model offers the advantage of clarifying our understanding of the diagnosis by elucidating its components.
The data regarding the DSM-IV criteria for borderline personality disorder obtained with the Diagnostic Interview for DSM-IV Personality Disorders
(20) demonstrated good internal consistency as indicated by an alpha of 0.86 and the pattern of intercriterion correlations that were found. Internal consistency (alpha=0.83) and intercorrelational results with the follow-up data were strikingly similar, lending further support. There was a lower endorsement of criterion number 5 (suicidal or self-mutilative behavior) in the follow-up study group, perhaps reflecting a lower level of acuity (recall that the baseline study group had been recruited largely at intake from clinical sites). The consistency of these data, along with the good statistical fit evidenced by the one-factor model, provides strong support for the latent diagnostic construct of borderline personality disorder.
While our results support the diagnostic construct as a whole, the three components of the disorder that were replicated in our study offer the advantage of a better understanding of the diagnostic heterogeneity found in patients diagnosed with borderline personality disorder. We also note that these components can be captured dimensionally by deriving factor scores. On the other hand, our identification of three components of the diagnosis of borderline personality disorder does not necessarily imply subtypes of the disorder. Factors that made up the three-factor model had intercorrelations of 0.90 or greater on both tests of the model, indicating that they are not in the least independent. Some of what is reflected in the heterogeneity of the disorder from our results (and from the results of other studies) could reflect the fact that different aspects of the disorder are present at different times. In this sense, one could postulate dynamic relationships between the latent constructs implied by the factors. For instance, affective dysregulation may moderate behavioral impulses. It will be important for future studies to look closely at the differential stabilities and temporal sequences of these factors to help better determine such relationships.
Findings from prior factor-analytic studies have produced useful results that identify key components of borderline personality disorder, but differences in the various editions of diagnostic systems employed, as well as the variety of populations studied, make comparisons of results difficult
(7–
10). Nonetheless, studies that have examined axis II personality disorders more broadly have demonstrated consistencies across various editions of DSM
(33–
35). It is especially noteworthy that the three-factor model
(9) was replicated in this study by using a more recent edition of the DSM (i.e., a model based on DSM-III-R criteria was replicated by using DSM-IV criteria), a more broadly based study group (i.e., a model based on a group of acutely disturbed psychiatric inpatients was replicated with a study group of individuals varying in level of treatment), and with a different measure (i.e., a model formed with data obtained from the Diagnostic Interview for DSM-IV Personality Disorders
[20] was replicated with data obtained from the Personality Disorder Examination
[36]). Replication of the three-factor model in light of these differences further supports the validity of the three-factor model.
Because our patient study group was large, demographically diverse, and derived from a number of different clinical sites, our results are more generalizable than those of prior studies. Patterns of co-occurring axis I and II diagnoses in our study group are comparable with those found in clinical study groups
(37). In addition, our study group was well defined, and our selection procedures ensured an adequate distribution of the criteria of borderline personality disorder as well as those of other axis II disorders so that a broad spectrum of axis II pathology was represented in our study group. The comparison group without personality disorder ensured that the spectrum of subjects without personality disorder was well represented.
Overall, our results provide statistical support for both the one- and the three-factor models of borderline personality disorder. The question might be raised as to which approach has the most utility for understanding this complex disorder. However, we do not view the unitary and three-factor models as necessarily competing. Rather, understanding borderline personality disorder in terms of these three constituent components offers a way to target areas for treatment, clarify etiological pathways, and address the problems associated with diagnostic co-occurrence in this complex disorder. Regarding the latter, these components may be helpful in clarifying the boundaries of borderline personality disorder in relation to other diagnoses. For example, the affective dysregulation component may have elements in common with axis I affective disorders. It will also be important for future studies to validate these factors externally. This could be done by using multitrait, multimethod procedures, including information other than from the DSM-IV, in future tests of the latent constructs that we identified. The components identified in our studies might also be refined by integrating data from other sources, such as dimensional measures of personality traits. Finally, an important area of study will be to test the stability of the factors and their relationship to various treatments.
Acknowledgements
The Collaborative Longitudinal Personality Disorders Study is an ongoing, longitudinal, multisite, follow-along study of personality disorders that is funded by the National Institute of Mental Health. Award sites are Brown University Department of Psychiatry and Human Behavior, Providence, R.I. (MH-50837), Columbia University and New York State Psychiatric Institute, New York (MH-50839), Harvard Medical School and McLean Hospital, Boston (MH-50840), Texas A&M University, College Station, Tex. (MH-50838), Vanderbilt University, Nashville, Tenn. (MH-50838), and Yale University School of Medicine, New Haven, Conn. (MH-50850). Collaborators, beside the authors, include Martin B. Keller (Brown University) and John M. Oldham (Columbia University) (principal investigators) and Jennifer Bame Rettew (Harvard University), Shirley Yen (Brown University), Elizabeth Schaefer (Harvard University), and Regina T. Dolan-Sewell (Brown University) (project coordinators).