Individuals with severe mental illness are at a high risk for blood-borne infectious diseases, such as HIV and hepatitis B. Hepatitis C virus shares risk factors for transmission with these viruses; 1.8% of the general population has been exposed to the hepatitis C virus and is therefore at risk for the long-term health consequences of chronic infection
(1). Ominously, a recent study
(2) found the seroprevalence of hepatitis C virus to be 19.6% among 931 severely mentally ill patients, approximately 11 times that of the general U.S. adult population. If representative of public-sector patients generally, this finding has grave import for treatment and outcome in this population. For comparison purposes, we attempted to determine the prevalence of hepatitis C among patients admitted to one public-sector psychiatric hospital outside Chicago.
Method
Laboratory information was reviewed on all civil patients admitted at least once to Elgin Mental Health Center between Jan. 1, 1998, and Dec. 30, 2000, who agreed to have blood sampled at admission; for those admitted more than once, the most recent results were used. During that time, routine admitting orders included syphilis serology, a CBC and blood chemistry, and testing for hepatitis B surface antigen and antibody. Testing for hepatitis C antibody was also routinely performed, with Abbott hepatitis C virus enzyme immunoassay 2.0 (Abbott Laboratories, Abbott Park, Ill.), and positive tests were repeated for confirmation and tested for viral load with RNA but without viral genotyping. Statistical analysis used SAS Version 6.12 (Cary, NC, SAS Institute, 1996); categorical data were analyzed with chi-square tests (with continuity correction where appropriate) and continuous data with Wilcoxon’s two-sample tests or t tests.
This retrospective study was approved by the institutional review boards of Elgin Mental Health Center and Finch University of Health Sciences/the Chicago Medical School and the Illinois Department of Human Services interdisciplinary research review board.
Results
Hepatitis C virus serostatus was available for 1,556 of 1,768 nonduplicated admissions, of whom 133 (8.5%) were seropositive. The 212 patients for whom hepatitis C virus serostatus was not available were slightly more likely to be married or divorced (χ2=16.59, df=5, p=0.005) but did not otherwise differ demographically or diagnostically (data not shown).
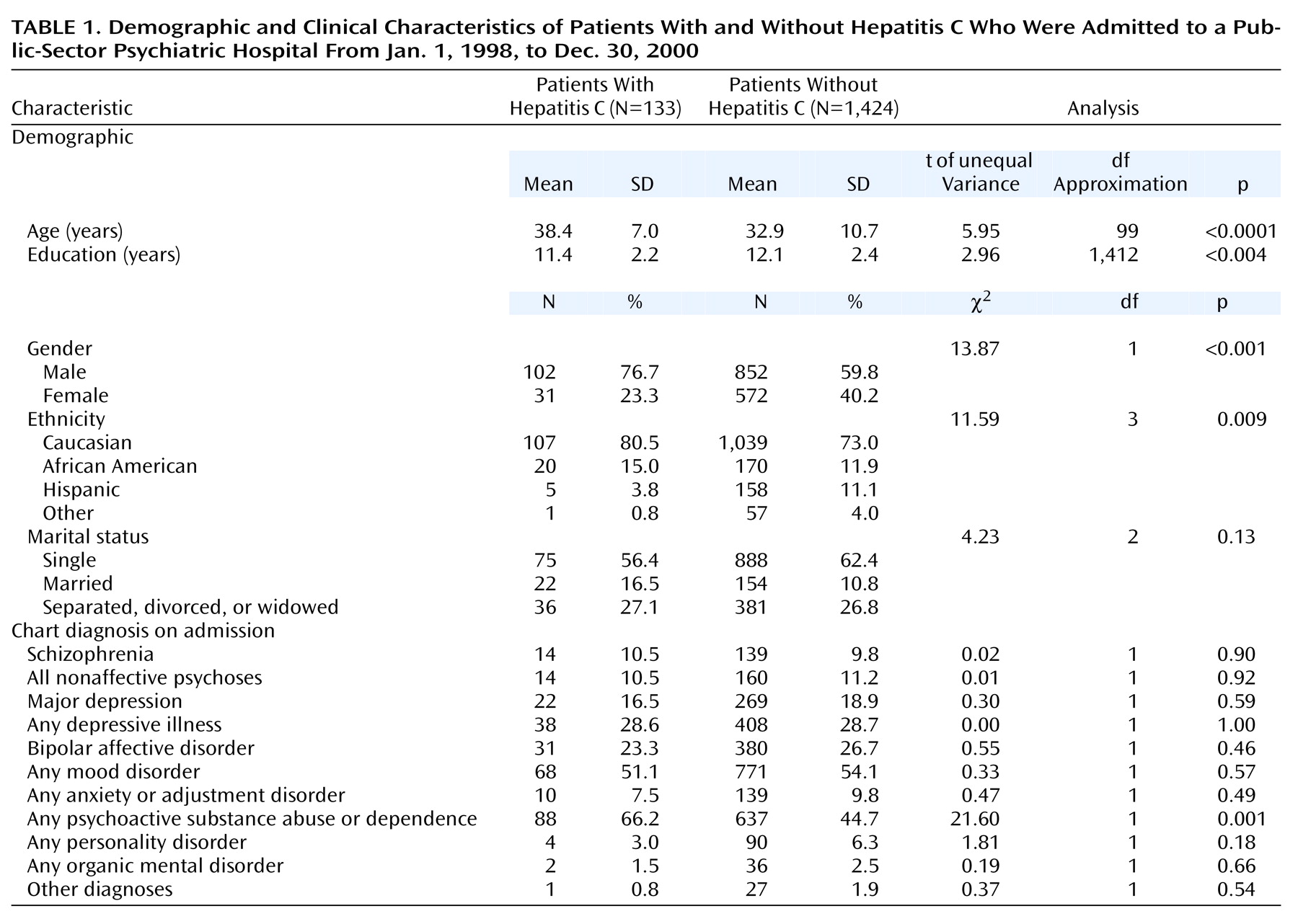
Patients who were positive for hepatitis C virus were more likely to be male, slightly less well educated, and slightly older and to have a psychoactive substance use disorder diagnosis but no other psychiatric diagnoses (
Table 1). Patients who were positive for hepatitis C virus had higher levels of alkaline phosphatase (z=4.19) and direct bilirubin (z=4.32) and lower albumen (z=–4.04) and platelet counts (z=–3.12) (p<0.01 in all instances).
However, few had abnormal values. Of 133 patients who were positive for hepatitis C virus, 12 (9.0%) had albumen levels below 3.5 mg/dl (in comparison to 58 [4.1%] of the 1,424 patients who were negative for hepatitis C virus) (χ2=5.84, df=1, p<0.02), and 14 (10.5%) had platelet counts of less than 130,000/ml (in comparison to 22 [1.5%] of those who were seronegative) (χ2=39.56, df=1, p<0.001). Direct bilirubin levels were more likely to be higher than 0.2 mg/dl among patients who were positive for the hepatitis C virus (in five [3.8%] of the 133 who were positive for hepatitis C in comparison to five [0.4%] of the 1,424 who were negative for hepatitis C) (χ2=17.12, df=1, p<0.001), but the groups did not differ in percentages showing abnormal elevations of either total bilirubin (above 1.3 mg/dl) or alkaline phosphatase (above 110 IU/liter). For total bilirubin, 5.3% (N=7) versus 3.9% (N=55) (χ2=0.31, df=1, p=0.58), respectively; for alkaline phosphatase, 5.3% (N=7) versus 3.9% (N=56) (χ2=0.26, df=1, p=0.61).
Alanine aminotransferase levels (obtained for 616 patients) were higher (z=8.12, p<0.001) and were somewhat more likely to be above the normal value of 60 IU/liter among patients who were seropositive (26 of 66 [39.4%] versus 29 of 550 [5.3%]) (χ2=80.23, df=1, p<0.001). Aspartate aminotransferase levels (obtained for 1,292 patients; z=10.51, p<0.001) were also higher overall and above 42 IU/liter in 51 of 106 (48.1%) of the patients who were positive for hepatitis C virus versus 97 of 1,186 (8.2%) of the patients who were negative for hepatitis C virus (χ2=149.08, df=1, p<0.001).
Hepatitis B surface antibody (indicating prior exposure) was present in 37 (27.8%) of the 133 patients who were positive for hepatitis C virus (versus 161 [11.3%] of 1,421 who were seronegative) (χ2=28.28, df=1, p<0.001). Only eight subjects (none of whom was seropositive for hepatitis C virus) had hepatitis B surface antigen (i.e., evidence of active infection) present. One of nine total subjects with positive rapid plasma reagin was seropositive for hepatitis C virus.
Discussion
Our results parallel those of Rosenberg et al.
(2), although we found roughly half the rates of hepatitis C virus and hepatitis B coinfection they found, perhaps reflecting either geographic differences in prevalence and/or differences in risk behaviors between the differently ascertained study groups
(3). In their study, risk factors were primarily injection drug use and high-risk sexual practices. Given the association with psychoactive substance use disorder diagnoses in our group, it may be that the same holds true in this group, although comparison data are lacking.
Relatively few patients who were positive for hepatitis C virus in our group had abnormally elevated aminotransferase levels; given the observed prevalence of hepatitis C, routine screening of admissions might be reasonable in this population.
Of those infected with hepatitis C virus, 55%–85% will progress to chronic infection, and while many never progress past a stage of chronically elevated aminotransferase levels without overt symptoms of liver disease, 10%–20% ultimately progress to hepatic cirrhosis, and many will develop hepatocellular carcinoma
(4,
5). Antiviral therapy is at present expensive, associated with significant side effects, ineffective in a substantial number of cases, and in this population likely to be difficult to administer because of the need for ongoing compliance and the lack of coordination between public health and mental care health systems
(6,
7). While little is known about hepatitis C outcome among the severely mentally ill, it is likely to be worse because of lack of access to and compliance with health care and further worsened by hepatic damage due to substance use
(8). Moreover, since most psychotropic drugs are hepatically metabolized, chronic hepatitis C may complicate pharmacotherapy in this population. The high prevalence of the virus in this population also places mental health care workers at risk for infection, many of whom may be unfamiliar with universal precautions protocol.
It seems likely that hepatitis C virus will differentially afflict the severely mentally ill, but the effectiveness of antiviral treatment in this population is unknown. Heightened awareness of potential hepatotoxicity when prescribing drugs, as well as education of those infected about cessation of substance use may improve clinical outcomes and indicate a role for more routine screening. However, much remains to be learned about primary prevention and effective provision of treatment in this group.