Schizophrenia Mutes Pleasure But Not Fear
Emotional abnormalities are among the most striking features of schizophrenia. Mapping these disturbances to brain regions has begun, but it is complicated by the effects of antipsychotic medications. Paradiso et al. (p. 1775) observed the brain functioning of medication-free schizophrenia patients as they rated pictures classified as pleasant or unpleasant. Compared to healthy volunteers, the patients rated the unpleasant images normally but gave significantly less positive ratings to the pleasant images. The patients did not activate frontal brain regions used by healthy volunteers as they rated the pleasant pictures, nor did they activate the “fear/danger recognition regions” such as the amygdala during the unpleasant pictures. Symptom severity also affected the ratings. Unpleasant pictures were rated as more unpleasant by patients with prominent psychotic symptoms (delusions and hallucinations), but less so by patients with negative symptoms.
Contrasting Visual Effects of Antipsychotic Drugs
In the days before antipsychotic medications, some patients reported hypersensitive perception of sensory stimuli, including visual contrast. Some recent studies, however, indicate poor detection of visual contrast. Chen et al. (p. 1795) propose that the dynamics of dopamine explain these findings. Dopamine is critical to the ability to detect visual contrast, and antipsychotic compounds block dopamine receptors. The newer, “atypical” antipsychotics block receptors for much shorter periods. This difference is demonstrated by the thresholds for detecting visual contrast in schizophrenia patients taking typical, atypical, and no antipsychotics and in healthy subjects. The average threshold was significantly higher for patients taking typical antipsychotics than for patients taking atypicals and for healthy subjects. The threshold for patients receiving no antipsychotics at all, on the other hand, was significantly lower than that of healthy subjects, consistent with heightened perceptual sensitivity.
Update on Race and Antipsychotic Drugs
Over the past 25 years, racial differences in the pharmacological treatment of schizophrenia have been reported. Copeland et al. (p. 1817) have extended these findings to the latest generation of antipsychotic medications, “atypicals,” which generally produce less troubling side effects. Among nearly 70,000 veterans receiving drug treatment for schizophrenia, Hispanic and African American patients were less likely to receive atypicals. Overall the discrepancy was not large, but for some drugs there were noteworthy differences. Clozapine prescriptions were less than half as common among African Americans and Hispanics as among whites. Clozapine is the first choice for refractory schizophrenia. It is also especially effective with coexisting substance abuse, but veterans with substance abuse were also less likely to receive it. The reasons for the racial discrepancies were not apparent, but concerns about diabetes and agranulocytosis may have reduced clozapine prescriptions for African Americans.
Check DNA Before Taking an Antidepressant?
Side effects of clozapine, an antipsychotic drug, have been linked to the gene for the serotonin (5-HT) 5-HT2A receptor, HTR2A. Many antidepressants also affect serotonin, and their side effects thus might also be related to individual variation in the HTR2A gene (genotypes). Another gene, CYP2D6, controls activity of an enzyme that is important in the metabolism of many antidepressants, including paroxetine and mirtazapine. Murphy et al. (p. 1830) examined the influence of HTR2A and CYP2D6 genotypes on side effects in elderly depressed patients taking paroxetine and mirtazapine, which activate and block 5-HT2A receptors, respectively. CYP2D6 genotype, determined with a high-throughput microarray technique, was not associated with side effects from either medication, and HTR2A genotype did not influence side effects from mirtazapine. However, patients taking paroxetine who had two C alleles at the HTR2A 102 T/C single nucleotide polymorphism (C/C genotype) had worse side effects and were more likely to stop treatment than were patients with the T/C or T/T genotype.
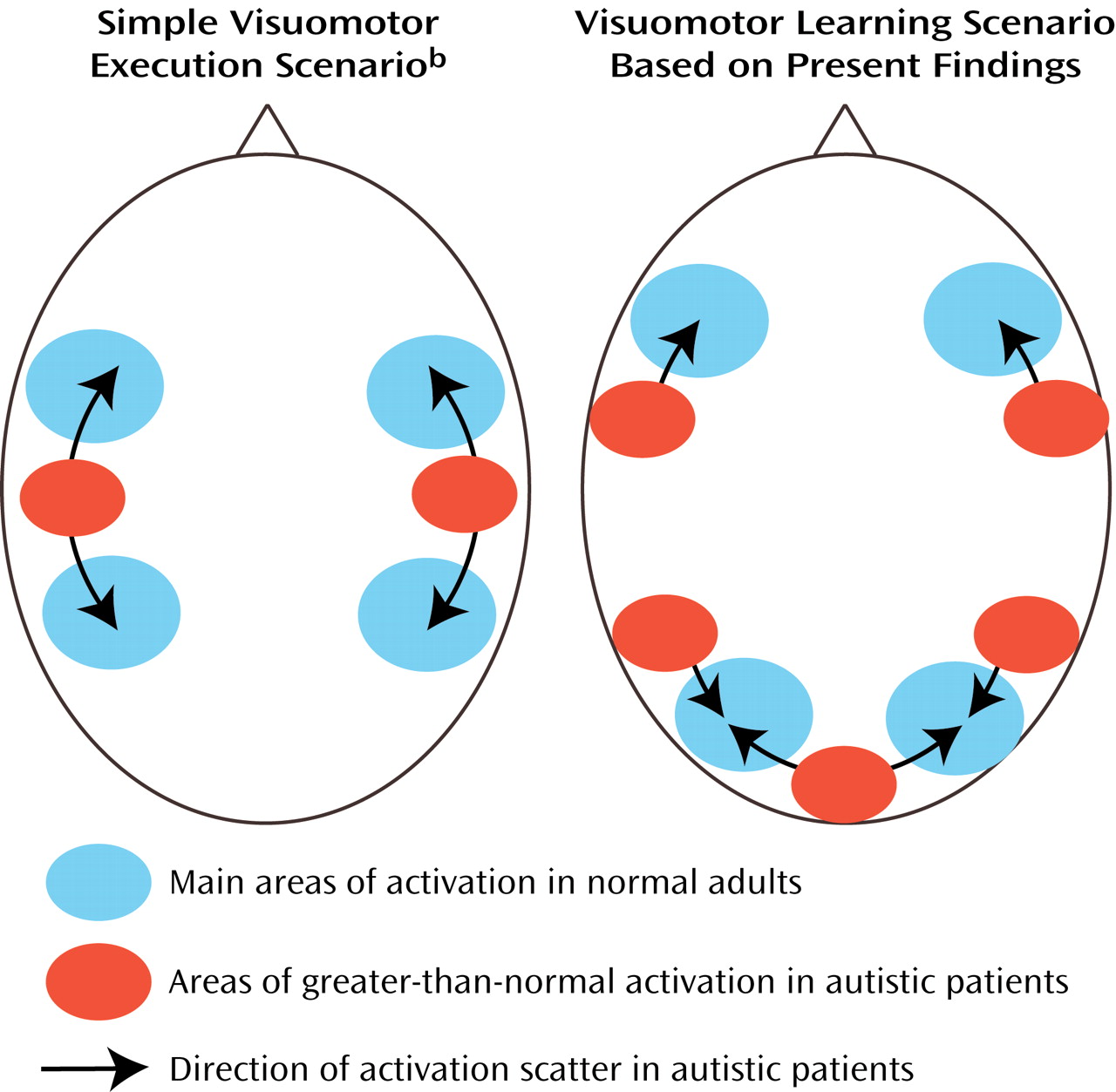
In Autism, Brain Activity Ranges Widely
When patients with autism make simple finger movements, activity in the brain is more widely distributed than it is in healthy subjects. Müller et al. (p. 1847) demonstrated similar findings with more complex visuomotor tasks involving learning. For both high-functioning patients with autism and healthy comparison subjects, extensive activation during the tasks occurred in premotor areas of the brain and in the parietal cortex, which is involved in visuospatial attention. However, the autistic patients showed greater activation in certain parietal areas and in the frontal lobes, and their within-group variability was consistently higher than that of the comparison group. These findings confirm the scattering of brain functions shown in other studies of autism. This scattering is consistent with the hypothesis that during neurodevelopment, brain regions involved in early-developing functions, e.g., motor control, crowd those for later, more complex functions, e.g., language.
The Journal Launches Web-Based Manuscript Submission and Peer Review!