Mapping the course of bipolar disorder systematically from onset is a critical research challenge
(1–
7). Prospective studies starting near illness onset are especially valuable for being less confounded by prolonged illness and comorbidity
(8–
15). Documenting the course of bipolar disorder reliably requires clinically meaningful definitions of specific disorder phases, ideally based on operational criteria that facilitate comparisons across studies. Efforts are emerging to develop operational criteria for syndromal, symptomatic, and functional recovery, to distinguish recovery from remission (sustained recovery), and to define switching (new illness phase without recovery), relapse (return of illness soon after recovery), and recurrence (later episode following recovery)
(10–
17). For over a decade, the McLean-Harvard First-Episode Project has been prospectively following bipolar disorder patients from their first lifetime hospitalization
(8–
10,
16,
17). This report is based on the assessment of patients with first-episode bipolar disorder who were followed for nearly 4 years to quantify time to specific types of recovery and time to new illness episodes as well as to identify predictors of recovery and new illness episodes.
Method
The research methods employed are detailed elsewhere
(10,
16,
17). Briefly, trained evaluators recruited subjects consecutively over 8 years (1989–1996) from inpatient units at McLean Hospital within 72 hours of hospitalization. Diagnoses were updated to DSM-IV criteria after 1994. Subjects were 18–75 years of age at first hospitalization, initially met DSM criteria for a manic or mixed episode, and provided written informed consent for study procedures approved by the McLean Institutional Review Board. Exclusion criteria were 1) current substance withdrawal; 2) delirium; 3) previous psychiatric hospitalization, unless for detoxification only; 4) documented IQ less than 70; 5) ill for more than 1 year; or 6) previous treatment with a mood stabilizer or antipsychotic for more than 3 months total.
Baseline Measures
Baseline and 2-year clinical assessments included the Structured Clinical Interview for DSM-III-R–Patient Version (SCID-P)
(18) conducted by master’s-level raters with more than 5 years experience, tested to maintain high interrater reliability. Detailed clinical narratives prepared from all available information (baseline and 2-year SCID-P assessments, medical records, and interviews with family members and primary treating clinicians) supported final DSM-IV diagnoses by a best-estimate procedure
(19). Baseline information collected by specifically trained research assistants included demographic and salient clinical data as well as psychosocial functioning for the preceding year, based on symptom rating scales, medical records, SCID-P assessments, and semistructured interviews of patients, relatives, and treating clinicians.
Assessment scales included the expanded Brief Psychiatric Rating Scale (BPRS)
(16,
17,
20) in which 36 items (35 individual factors, including bipolar disorder selective items, and a global score) are each rated for severity (score range=0–7), and a total summed score and subscale scores for psychosis, mania, and depression are also obtained
(9). Other scales used were 1) the Clinical Global Impression (CGI) scale
(21) (score range=1–7); 2) the DSM-IV Global Assessment of Functioning (score range=0–100); 3) the Young Mania Rating Scale
(22); and 4) the 31-item Hamilton Depression Rating Scale
(23). Functional status was rated for occupational level with the Modified Vocational Status Index
(9) (score range=1–7), and residential status was rated with the Modified Location Code Index
(24) (score range=1–9). Both were compared with the highest levels within the preintake year by using a best-estimate procedure
(19) based on information from subjects, family members, and medical records
(9,
16,
17,
20).
Outcome Assessments and Definitions
Inpatients were assessed approximately weekly until discharged. At 6, 12, 24, 36, and 48 months after hospital discharge, follow-up information (e.g., symptoms, occupational and residential status, and current treatment) was obtained systematically by experienced raters blind to baseline information by telephone-based semistructured interviews found to be valid and reliable compared with face-to-face assessments
(25).
Syndromal recovery was defined as a severity rating ≤3 for the DSM-IV A criterion for mania (range=1–7), with no B criterion rated greater than 3 and no two B criteria rated at 3
(10,
14–17). Patients with initial mixed episodes fulfilled recovery criteria for a manic and a depressive episode (no depression criterion >3, nor more than three at 3). In addition, CGI ratings had to be ≤2. For syndromal remission, patients had to maintain recovery criteria for at least 8 weeks, but latency to recovery was timed from hospital entry to when recovery criteria were first met. Symptomatic recovery was defined conservatively (minimal, subsyndromal symptom severity) as total Young Mania Rating Scale score ≤5 and Hamilton depression scale score ≤8, selected to reflect near absence of symptoms
(26,
27).
Functional recovery required that ratings for both occupational level and residential status returned to or exceeded the highest levels within the preintake year, using a best-estimate procedure
(19) based on information from subjects, family members, and medical records
(9,
16,
17,
24).
New illness episodes met DSM criteria for mania, mixed state, psychosis, or major depression. Switching was defined as an early phase shift (to depression, mixed state, or psychosis without mania) without an interval of recovery from the index episode. Relapse was defined as any new illness episode within 8 weeks of syndromal recovery. New episodes after 8-week recovery (remission) were classified as recurrences. Switches were not considered in analyses of time to new illness (relapses or recurrences) or of risk factors for new episodes. Time to new episode was estimated as days from initial recovery to the start of a new episode.
Interrater reliability for SCID-P-based diagnoses yielded an average intraclass correlation coefficient (ICC) of 0.92 for primary diagnoses and 0.90 for secondary disorders
(9). High interrater reliability was also obtained for the expanded BPRS (ICC=0.96), and there was excellent agreement (ICC=0.90) between telephone and in-person outcome assessments
(25).
Statistical Analyses
Age at onset was median-dichotomized (28 years). Onset/prodrome was rated rapid (≤6 months) or gradual (>6 months). Individual expanded BPRS items were rated severe (scored 5–7) or nonsevere (0–4), and a median split for scores on the expanded BPRS subscale items of mania, depression, or psychosis provided high- and low-scoring subgroups.
Rates of recovery or new episodes among recovered patients were compared in subgroups of interest by using contingency tables (chi-square) or Fisher’s exact test if cells held <10 subjects (with df=1, unless stated otherwise). Mann-Whitney (U) rank methods compared distributions of continuous variables in subgroups. Group recovery and recurrence latencies were compared by Kaplan-Meier life table survival analyses, tested with Mantel-Cox log-rank (chi-square) tests. Variables with preliminary bivariate associations (p≤0.10) with recovery or recurrence were included in multivariate analyses.
Cox proportional hazards models (for time to syndromal recovery and to new episode) and multiple logistic regression models (for categorical functional recovery) evaluated candidate variables for independent association with outcomes. For both types of models, we computed robust standard errors (SEs) or associated 95% confidence intervals (CIs). We tested goodness of fit of multivariate models by deciles of fitted values and partial residual plot methods
(28). We also checked for compliance with the proportional hazards assumption and for goodness of fit of Cox models with Arjas plots and Schoenfeld residuals
(29). Explanatory variables with adjusted odds ratios (for logistic regression) or hazard ratios (for Cox regression) substantially different from 1.0 (p<0.05) were retained for final multivariate regression models.
Averages are means with standard deviations. Times to recovery or recurrence (and 95% CI) in survival analyses were estimated as weeks by which 50% of subjects (or 25%, if <50% by 2 years) reached recovery or new illness. Correlations were determined by linear regression (r) or Spearman nonparametric rank (rs) methods. Statistical significance required two-tailed p<0.05. Analyses were performed with commercial microcomputer programs (Stata, Stata Corp., College Station, Tex.; Statview-5, SAS Institute, Cary, N.C.).
Results
Subject Characteristics at Baseline
Subjects were recruited from a total of 784 patients experiencing their first lifetime psychiatric hospitalization (1989–1996), of whom 239 were in their first manic/mixed episode of bipolar I disorder; 173 of these subjects (72.4%, 95 men and 78 women) were recruited for this study. The mean age was 32.5 years (SD=13.7, range=18–72, median=28). The 66 nonrecruited patients either did not complete initial evaluations during a very brief hospitalization (N=42), did not meet study criteria (N=10), or refused to participate (N=14). Of the 173 subjects, 151 (87.3%) were followed for 2 years; overall, follow-up averaged 4.86 years (SD=2.51). Among the 22 with incomplete follow-up data (at 6 months: N=14; at 12 months: N=2; at 24 months: N=6), eight were lost to follow-up, one died, and 13 withdrew consent. There were no significant differences in sex or age between recruited and nonrecruited patients nor were there differences in sex, age, or initial illness severity ratings between those followed for 2 years and those lost to follow-up.
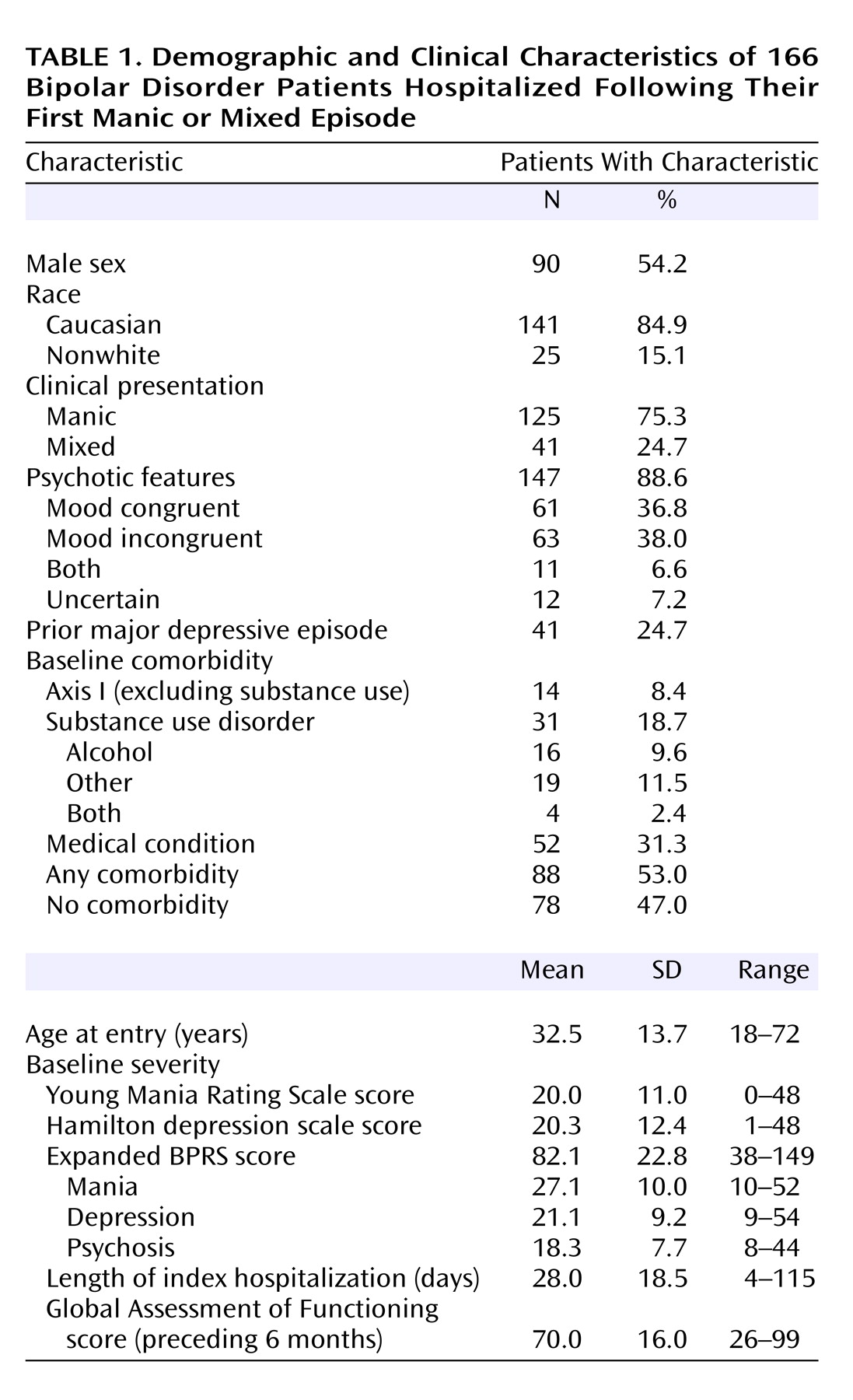
By 2 years, seven (4.0%) of 173 entering subjects had been rediagnosed to nonaffective psychotic (N=3) or schizoaffective (N=4) disorders; analyses presented are for the 166 remaining subjects. At admission (
Table 1), the episodes of 125 of the 166 subjects were manic (75.3%), and 41 (24.7%) were mixed. Most subjects (N=147, 88.6%) had initial psychotic features considered mood congruent or mood incongruent; 11 (6.6%) had both at different times. Most subjects (N=125, 75.3%) were in their first lifetime affective episode, but 41 (24.7%) had experienced prior episodes of depression that did not require hospitalization. Axis I (N=14, 8.4%), substance use (N=31, 18.7%), or general medical (N=52, 31.3%) comorbidity affected 88 subjects (53.0%); nine had two or more comorbid diagnoses. Initial scores on the total expanded BPRS and Young Mania Rating Scale indicated moderate to high symptomatic severity (
Table 1). Length of the average initial hospital stay diminished greatly across intake years, from 43.7 days (SD=24.0) in 1989 to only 10.8 days (SD=4.6) in 1996 (for length of stay versus intake years, r
s=–0.58, N=166, p<0.0001).
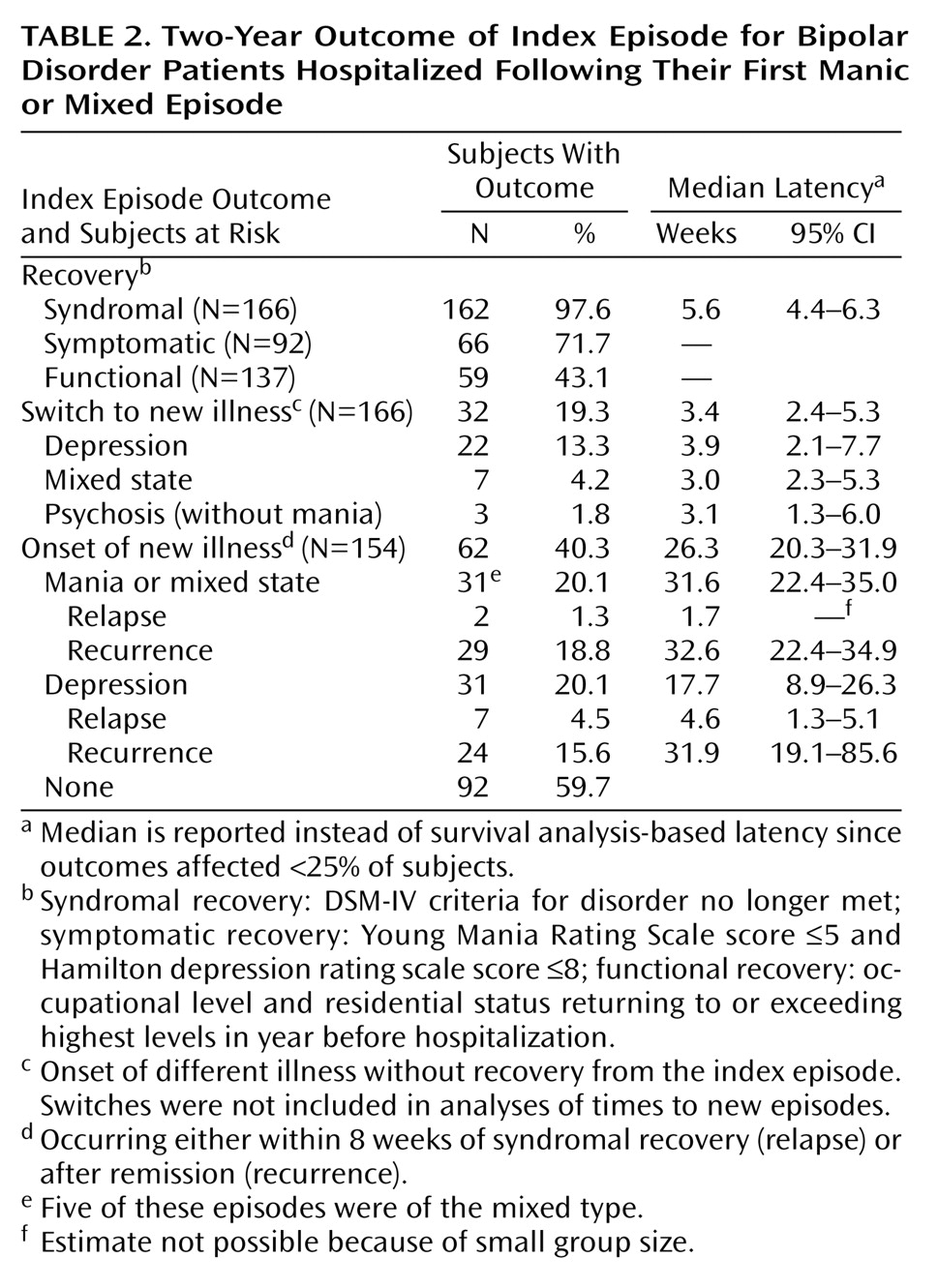
Likelihood of Syndromal, Symptomatic, and Functional Recovery
Nearly all subjects (97.6%, N=162) achieved syndromal recovery from their initial manic/mixed episode by 2 years, with a mean latency of 13.7 weeks (SD=21.8; median=5.6), and a survival computed time to 50% of subjects recovered of 5.4 weeks (
Table 2). Survival computed proportions of subjects recovering by 3, 6, 12, and 24 months, respectively, were 76.5% (N=127), 85.5% (N=142), 91.6% (N=152), and 97.6% (N=162). According to Young Mania Rating Scale and Hamilton depression scale ratings, only 71.7% of subjects (N=66 of 92) were considered symptomatically recovered by 2 years (
Table 2). At 6 and 24 months of follow-up, respectively, only 39.5% (N=60 of 152) and 43.1% (N=59 of 137) had achieved functional recovery according to residential and occupational status, although another 13.3% (N=22 of 166) had achieved and then lost functional recovery within 2 years of intake.
Factors Associated With Syndromal and Functional Recovery
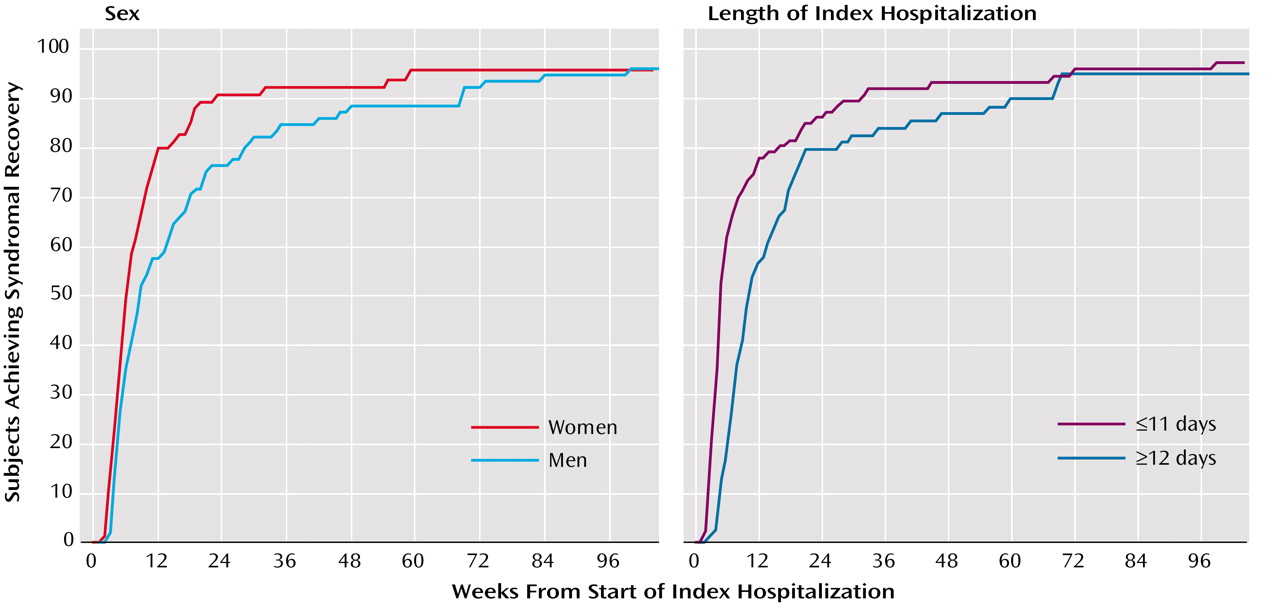
Initial bivariate comparisons identified factors associated with a shorter time to syndromal recovery in 50% of the subjects (in descending order of significance, all df=1): attaining functional recovery at 6 months (4.6 versus 7.4 weeks; χ2=11.1, p<0.001); below-median length of stay, adjusted for intake year (3.6 versus 8.3 weeks; χ2=9.71, p=0.002); below-median baseline depression ratings (4.9 versus 8.0 weeks; χ2=6.64, p=0.01); above median (28 years) age at study entry (4.6 versus 7.3 weeks; χ2=4.63, p=0.03); and being married (5.0 versus 6.1 weeks; χ2=4.30, p=0.04). Other factors with lesser association included absence of initial mood-incongruent psychotic features (5.1 versus 7.1 weeks; χ2=3.27, p=0.07), and female sex (5.1 versus 6.1 weeks; χ2=1.94, p=0.16). Ethnicity was uncorrelated with time to syndromal recovery (Caucasian versus other: 5.4 versus 8.0 weeks; χ2=1.41, p=0.24).
Similar preliminary bivariate analyses for likelihood of achieving functional recovery at 2 years found the following factors: older age (≥30 years) at entry (58.5% versus 29.2%; χ2=12.0, p=0.001); shorter length of index hospitalization (55.7% versus 29.9%; χ2=9.34, p=0.002); Caucasian versus other race (47.5% versus 15.8%; χ2=6.69, p=0.01); and being married (58.3% versus 37.6%; χ2=4.64, p=0.03). Having below- versus above-median baseline depression ratings was weakly related to functional recovery (50.0% versus 35.7%; χ2=2.37, p=0.12). Women and men did not differ in likelihood of functional recovery (44.4% versus 41.9%; χ2=0.09, p=0.76), and there was no correlation of presence/absence of mood-incongruent psychotic features with functional recovery (43.3% versus 45.9%; χ2=0.08, p=0.78).
We then applied Cox (syndromal recovery) and logistic (functional recovery) multivariate regression analyses to factors identified by the preceding bivariate analyses (p≤0.10), plus initial depression severity and sex. Only three features remained associated with earlier syndromal recovery: 1) shorter initial hospitalization (hazard ratio=1.99, 95% CI=1.36–2.93; p<0.001); 2) female sex (hazard ratio=1.72, 95% CI=1.16–2.56; p=0.008); and 3) below-median initial depression ratings (hazard ratio=1.65, 95% CI=1.14–2.39; p=0.008). For functional recovery at 2 years, only two factors were significantly associated: 1) being older than 30 (odds ratio=3.28, 95% CI=1.58–6.82; p=0.001) and 2) shorter initial hospitalization (odds ratio=2.82, 95% CI=1.36–5.88; p=0.006). The survival analyses of recovery versus time functions for women/men and for shorter/longer initial hospitalization are depicted in
Figure 1.
Risks and Timing of First Relapse or Recurrence
By 2 years, 92 (59.7%) of 154 subjects who attained syndromal recovery from the initial episode of mania had both reached and remained in remission without new episodes following recovery from the index episode (
Table 2). However, 32 (19.3%) of 166 switched without recovery directly into an episode of depression (N=22), a mixed state (N=7), or psychosis (N=3). Only 5.8% (N=9 of 154) experienced an early relapse (mania or mixed state: N=2; depression: N=7). Another 34.4% (N=53 of 154) experienced a recurrence (mania: N=24; mixed state: N=5; depression: N=24) within 2 years of follow-up postrecovery. Overall median latency to 50% risk of any new episode (first relapse or recurrence) was 26.3 weeks (relapse: 4.3 weeks [95% CI=0.3–5.1]; recurrence: 32.3 weeks [95% CI=22.4–34.9]). Risks of new episodes of mania and depression were equal in incidence (both N=31, 20.1%), but latency to new depression was shorter than to new mania (17.7 versus 31.6 weeks [z=7.8, p<0.001]).
Factors Predicting New Illness Episodes
In preliminary bivariate analyses, the following factors were associated with greater risk of new mania (all df=1): lower occupational status (25% versus 12.9%; χ2=4.50, p=0.03); psychotic features at baseline (22.8% versus 0%; χ2=4.71, p=0.03); initial manic versus mixed presentation (23.7% versus 8.3%; χ2=4.07, p=0.04); and above-median index hospitalization length (27.1% versus 14.3%; χ2=3.93, p=0.05). The following univariate factors were associated with greater risk of new depression: initial mixed versus manic presentation (44.4% versus 12.7%; χ2=18.5, p=0.001); higher occupational status (32.3% versus 12.0%; χ2=8.31, p=0.004); above-median initial depression score (32.8% versus 15.4%; χ2=5.25, p=0.02); and lack of initial psychotic features (38.9% versus 17.7%; χ2=4.60, p=0.03). Initial expanded BPRS total or subscale severity ratings for mania, depression, or psychosis were uncorrelated with the occurrence of new episodes of mania or depression.
Multivariate Cox regression analyses of factors with suggestive preliminary associations found new episodes of mania to be associated, in rank-order, with initial mood-congruent psychotic features (hazard ratio=2.79, 95% CI=1.31–5.91; p=0.007); relatively low premorbid occupational status (hazard ratio=2.53, 95% CI=1.15–5.55; p=0.02); and initial manic versus mixed state (hazard ratio=3.38, 95% CI=1.00–11.5; p=0.05). In contrast, new episodes of depression were associated with higher initial occupational status (hazard ratio=5.08, 95% CI=2.16–11.9; p<0.0001); initial mixed presentation (hazard ratio=4.52, 95% CI=2.23–9.16; p<0.0001); and any comorbidity (hazard ratio=2.60, 95% CI=1.20–5.66; p=0.02).
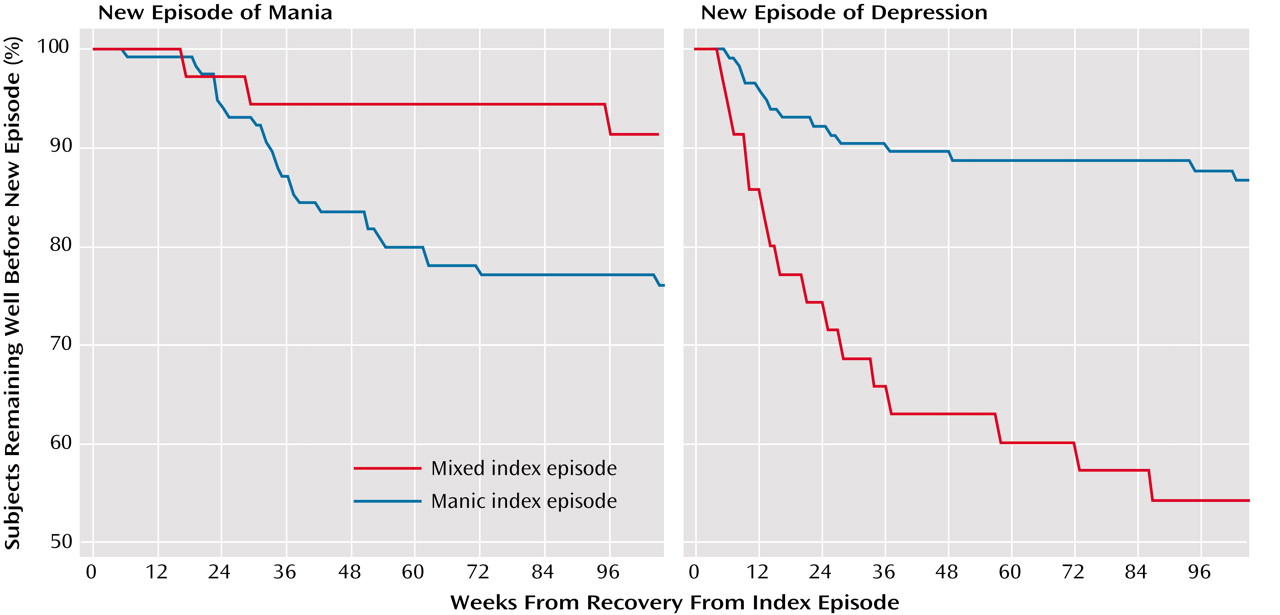
A slightly shorter time to onset of a new episode of mania was found in those whose initial presentation was manic versus mixed (χ
2=4.65, df=1, p=0.03) (
Figure 2), but there was a much shorter time to onset of a new episode of depression in those whose initial presentation was mixed versus manic (χ
2=14.1, df=1, p<0.0001) (
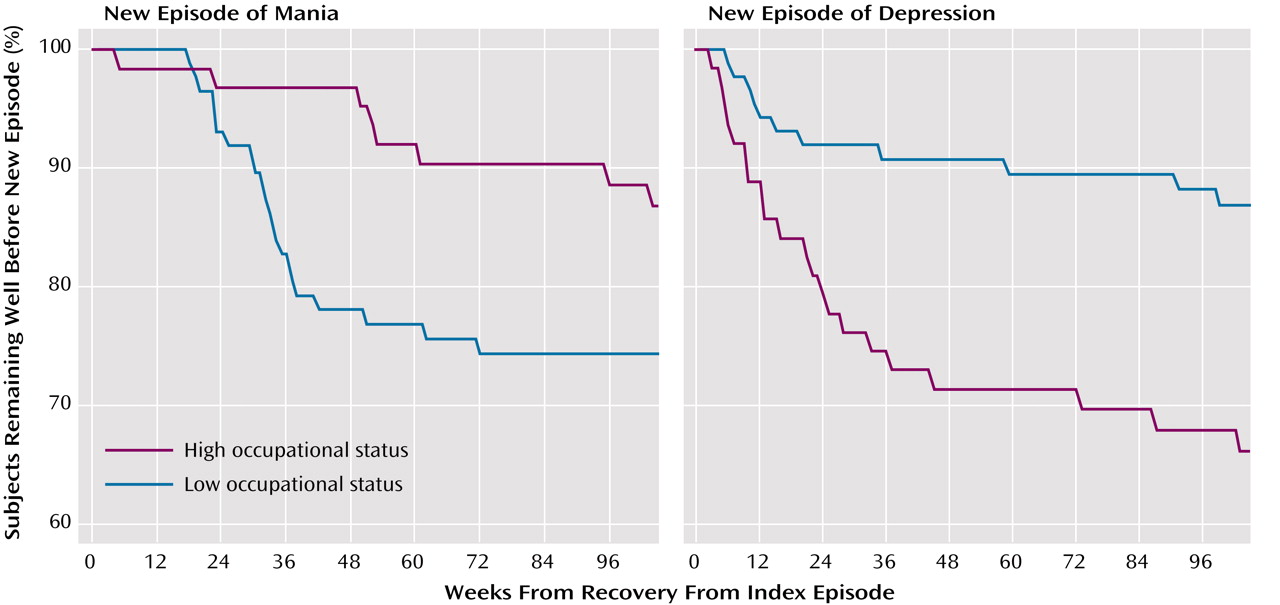
Figure 2). Also, time to onset of a new episode of mania was shorter with lower occupational status (χ
2=4.57, df=1, p=0.03) (
Figure 3), but time to onset of a new episode of depression was shorter with higher occupational status (χ
2=10.4, p=0.001). There was also a significant interaction, indicating that most of the relationship between new episodes of depression and higher baseline occupational status was found following mixed-state presentations.
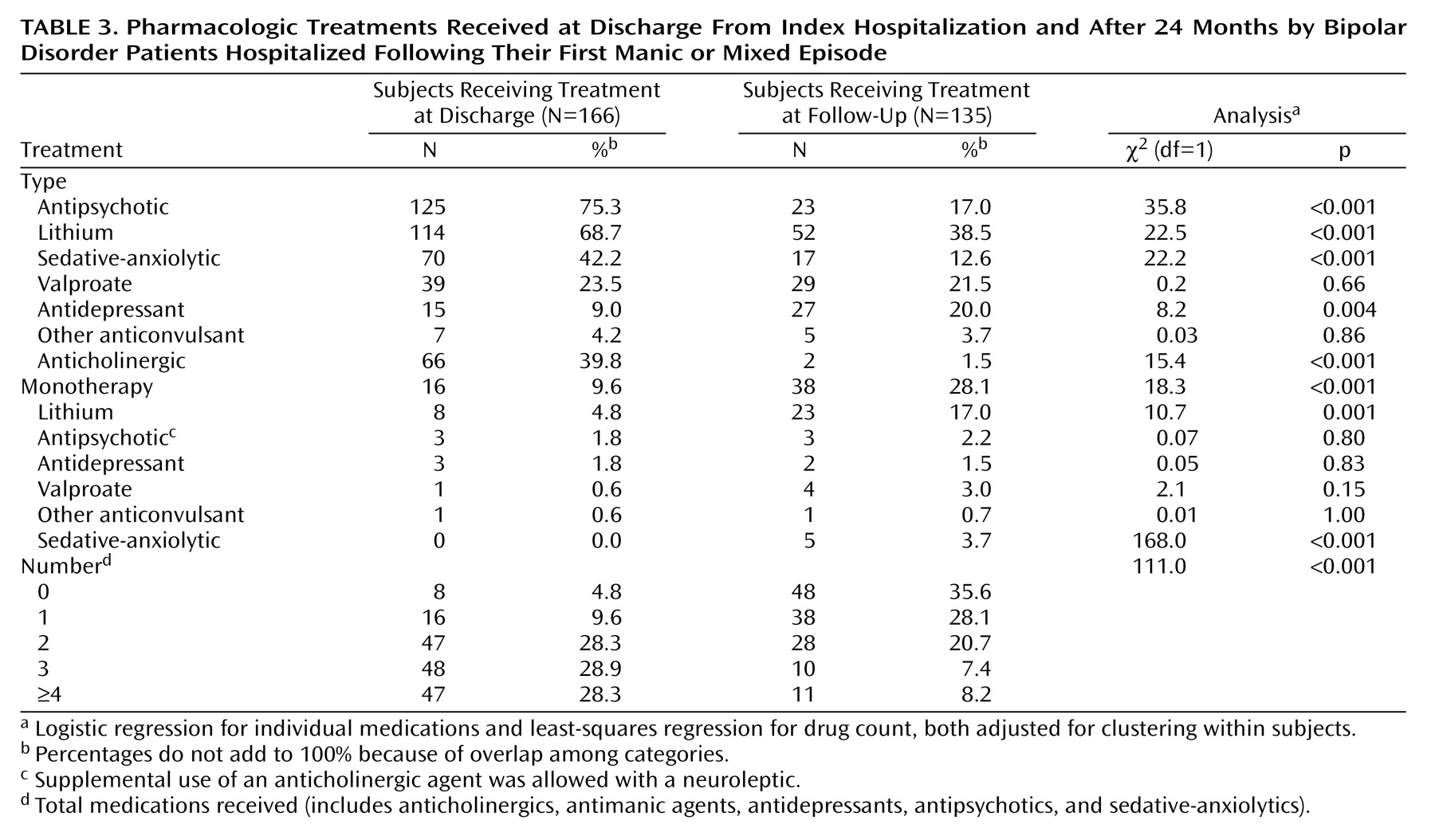
Treatment
Treatments received at index hospitalization discharge and at 24-month follow-up were assigned clinically and varied widely (
Table 3). Almost all subjects (95.2%, N=158 of 166) received at least one psychotropic agent at discharge, but at 2-year follow-up, 35.6% (N=48 of 135) were taking no medication. At discharge, the most commonly prescribed drugs (alone or in various combinations) were antipsychotics (75.3%, N=125 of 166) and lithium (68.7%, N=114), with less use of sedatives or anticonvulsants. At 2-year follow-up, lithium was the most frequent treatment (38.5%, N=52 of 135), and antipsychotic use had declined, with a corresponding decline in use of antiparkinsonism agents. There was also less use of sedatives, whereas anticonvulsant use (valproate and others) decreased only slightly, from 27.7% to 25.2% (
Table 3). Antidepressants were used occasionally at discharge (9.0%, N=15), usually in combination with an antimanic agent, and their use increased by the 2-year follow-up evaluation.
Treatment and Outcomes
Time to 50% of subjects attaining syndromal recovery varied with specific treatments (alone or in combination): lithium=5.4 weeks (95% CI=4.6–7.44), antipsychotics=6.3 weeks (95% CI=5.1–8.3), anticonvulsants=8.0 weeks (95% CI=5.6–10.7), and antidepressants=14.3 weeks (95% CI=2.1–23.6). However, the differences were not significant, as seen by a comparison of the extremes (lithium versus antidepressants: χ2=1.03, df=1, p=0.31). Latency to 25% risk of a new episode following recovery similarly varied: antipsychotics=31.9 weeks (95% CI=22.4–48.6), lithium=30.7 weeks (95% CI=20.9–43.6), anticonvulsants=23.6 weeks (95% CI=8.3–39.4), and antidepressants=12.4 weeks (95% CI=5.1–31.3). Again, however, these differences were nonsignificant (e.g., antidepressants versus lithium: χ2=1.65, df=1, p=0.20).
Discussion
This study, based on the largest reported sample of patients in a first manic/mixed episode of DSM-IV bipolar I disorder, followed 173 patients prospectively under naturalistic conditions through nearly 5 years after first lifetime psychiatric hospitalization. Patient recruitment (72%) and retention (87%) were high, and the naturalistic study design permits realistic evaluation of contemporary clinical outcomes. Limiting entry to first-episode patients limits potential bias of prolonged illnesses and often already poor outcomes. In our subjects, comorbidity (53%, N=88 of 166) and initial psychotic features (89%, N=147) were somewhat more common than in some other studies
(30–
32). These features may reflect preferential hospitalization of relatively severely ill manic patients. Indeed, generalizability of our findings may be limited by sampling only patients hospitalized for a first episode of mania, although most patients in a first episode of mania require hospitalization
(33). Another limitation is that premorbid functional levels were assessed by retrospectively collected information. However, these ratings were based on all available information, including from family members and a best-estimate consensus.
Key findings include marked differences in syndromal (98%), symptomatic (72%), and functional (43%) measures of recovery from onset of a first lifetime manic/mixed bipolar episode within 2 years (
Table 2). The differences between syndromal and symptomatic recovery are consistent with clinical impressions and research findings that many bipolar disorder patients, even though not meeting DSM-IV criteria for an episode, still experience significant subsyndromal morbidity, particularly mild depressive symptoms, over prolonged periods
(11,
16,
17,
32,
34–36). Major disparity between syndromal and functional recovery has been reported previously
(9,
10,
14). In a Cincinnati sample, 35% of manic patients recovered functionally by 12 months
(15). This rate is similar to our 39%–43% at 6–24 months. Another 13% achieved and then lost functional recovery within 2 years of follow-up. Syndromal recovery came earlier after relatively brief initial hospitalization, among women, and in those with lower initial depression ratings; functional recovery at 2 years was more likely among older patients and after briefer hospitalization. Syndromal recovery also tended to be most delayed among patients given an antidepressant at hospital discharge and earliest among those treated with lithium.
New episodes (relapses and recurrences) occurred in 40% (N=62 of 154) subjects within 2 years of study intake. Another 19% (N=32 of 166) switched into new phases of illness (mainly depression) without recovery from the index manic episode. In the aggregate, 57% (N=94 of 166) experienced new illness during the follow-up period (
Table 2), consistent with reported failure rates of 39%–52% per year during various maintenance treatments in bipolar disorder patients
(34–
41).
Several factors differentially predicted new episodes of mania versus depression. Significant predictors of a new episode of mania were initial mood-congruent psychotic features, low prehospitalization occupational status, and nonmixed initial mania. In contrast, higher occupational achievement, initial mixed dysphoric states, and psychiatric or medical comorbidity predicted future bipolar depression. Other studies have reported that mixed dysphoric presentation
(9,
42), comorbidity
(9,
39), and psychotic features were associated with poorer outcomes in bipolar disorder
(9,
10,
30–34). Bipolar depression following higher premorbid occupational achievement may reflect the demoralizing impact of severe mental illness on previously relatively healthy and successful young persons. Of note, the initial severity of depression, but not the presence of an initial mixed episode, was associated with outcome in some analyses (e.g., bivariate analyses for functional recovery). It is possible that this apparent discrepancy reflects the narrow DSM-IV definition of “mixed” episodes (syndromal mania co-occurring with full syndromal depression) and the relatively broad inclusion of not only pure mania but also a range of degrees of dysphoria or subsyndromal depression in manic episodes
(43,
44).
Noteworthy treatment-related findings include relatively common use of antipsychotics, sedatives, and lithium at initial hospitalization, with much less use of these drugs 2 years later. Monotherapy was uncommon and usually limited to lithium. Polytherapy with more than three psychotropic drugs, although prevalent at discharge (57%, N=95 of 166 cases), was uncommon at follow-up (16%, N=21 of 135 subjects). The 36% rate of no medication use by the 2-year follow-up evaluation may, in part, reflect noncompliance
(14). Tendencies toward earliest recovery and slowest return of illness among those treated with lithium, and the opposite among those given an antidepressant, are intriguing but difficult to interpret because treatment was not randomly assigned.
In conclusion, strikingly high proportions of patients initially hospitalized with bipolar I disorder encountered substantial levels of morbidity, comorbidity, and dysfunction in the early years of their course. Evidently, current treatments for bipolar disorder, although effective in facilitating early syndromal recovery, provide incomplete long-term protection against subsyndromal symptoms, switches, relapses, or recurrences and have particularly limited impact on functional recovery—at least among those requiring early hospitalization. These sobering findings encourage earlier case-finding and intervention, with much greater emphasis on subsyndromal illness, depression, and functional recovery. Improved treatments for bipolar disorder should include greater integration of psychosocial and rehabilitative interventions with effective and better tolerated medication—all applied early and consistently
(5,
45).