Cigarette smoking continues to be the single most important preventable cause of death and disability in the United States
(1). Several studies have reported higher rates of tobacco dependence among individuals with mental illness than among those without mental illness
(2,
3). Smoking-cessation counseling is an effective treatment for tobacco dependence
(4); however, previous research suggests that primary care physicians offer smoking-cessation counseling to about one-fifth of their patients who smoke
(5). With respect to those with psychiatric illness, APA’s
Practice Guideline for the Treatment of Patients With Nicotine Dependence (6) suggests that smoking-cessation counseling can be beneficial.
The goal of this study was 1) to determine how often psychiatrists offer smoking-cessation counseling to their patients who smoke and 2) to determine which factors are independently associated with a psychiatrist offering smoking-cessation counseling to their patients who smoke.
Method
Using the National Ambulatory Medical Care Survey (http://www.cdc.gov/nchs/about/major/ahcd/namcsdes.htm), we conducted a cross-sectional analysis of office-based visits to psychiatrists for individuals 18 years of age and older during 1992–1996 to investigate the prevalence of smoking-cessation counseling.
The National Ambulatory Medical Care Survey
(7) is a national probability sample survey conducted by the National Center for Health Statistics, which annually collects information on the use of ambulatory medical services provided by office-based physicians in the United States. Physicians complete a one-page form on a systematic sampling of office visits occurring during a random 1-week period. The survey does not include physician visits in federally based and hospital-based outpatient settings, so it reflects mainly nonacademic physicians. For the years 1992–1996, the response rate for the survey was approximately 70%. To minimize the effect of nonresponse estimates, the National Ambulatory Medical Care Survey data were adjusted by imputing for nonresponding physicians the practice characteristics of similar responding physicians.
From 1992 to 1996, the survey included questions on smoking status and smoking-cessation counseling. Current smoking status was reported by checking one of the following boxes: smoker, nonsmoker, or smoking status unknown. The nonsmokers category may have included both ex-smokers and those who had never smoked. Smoking-cessation counseling was reported by checking a box under the heading, “Tobacco use/exposure” if counseling was given. Counseling could include information on smoking cessation and prevention of tobacco use, as well as referrals for smoking-cessation programs. Our dependent variable was whether psychiatrists offered smoking-cessation counseling during office visits to psychiatric patients who smoked.
The National Ambulatory Medical Care Survey collects information on basic patient demographics, diagnoses, and treatment. We used information regarding patient characteristics and practice-setting characteristics that we hypothesized might influence a psychiatrist’s decision to offer smoking-cessation counseling. Patient characteristics were age, gender, geographic region (Northeast, South, Midwest, West), payment source (private fee-for-service insurance, health maintenance organization, Medicaid, Medicare, or self-pay/no charge), and diagnoses. Psychiatric diagnoses were based on ICD-9 codes and categorized into five separate conditions: psychotic disorders, depressive disorders, bipolar affective disorders, anxiety disorders, and substance use disorders. Medical diagnoses associated with an increased risk for cardiovascular disease were present if physicians recorded obesity, hypertension, or diabetes mellitus either by ICD-9 code, by checking a box for these diagnoses, or by documenting medication for diabetes mellitus. Characteristics regarding practice setting were available for urban versus rural location and follow-up visit versus new-patient visit.
We performed chi-square tests and developed a logistic regression model to examine visit characteristics associated with receiving smoking-cessation counseling
(8).
Although the National Ambulatory Medical Care Survey is based on a complex multistage sampling design, for confidentiality reasons, the National Center for Health Statistics does not release the primary sampling units for these surveys. Because this analysis tested a hypothesis of an association, we report results with unweighted data
(9). We performed multiple sensitivity analyses using different techniques to approximate the complex survey design by using the survey weights in the analysis and the strata of geographic region and urban or rural designation as a proxy for primary sampling units. These results were essentially similar to and unchanged from logistic regression models using unweighted data. In order to account for the possibility of physician clustering, we reanalyzed our logistic regression model using generalized estimation equations
(10).
Results
There were 8,451 visits to 573 unique psychiatrists from 1992 to 1996. In 75.7% (N=6,400) of the 8,451 visits to psychiatrists, physicians classified patients as either smokers or nonsmokers, while in 23.0% of the visits, the physician did not know the smoking status of the patient. Of the 6,400 visits in which the physician knew the patient’s smoking status, in 25.2% (N=1,610) of these visits, the physicians documented that the patients were smokers. Our analysis focused on these 1,610 visits for smokers.
The mean age was 41.7 years (SD=12.2). A total of 52.0% of the visits were for women, 94.1% were for Caucasians, and Medicaid or Medicare insured 25.0% of the visits. A total of 88.3% of the psychiatric office visits occurred in metropolitan areas, divided nearly equally between the following geographic regions: Northeast (25.4%), South (28.4%), Midwest (20.1%), and West (26.1%). Approximately 10% of the visits were made by patients diagnosed with bipolar affective disorders, 80% of the patients were diagnosed with a depressive disorder, 20% were diagnosed with a drug use disorder, and 13% had obesity, hypertension, or diabetes mellitus. A total of 9.1% of these visits were categorized as continuity visits or return visits to the same physician. Psychiatrists offered diet counseling at 6% of the patient visits and exercise counseling at 4% of the visits.
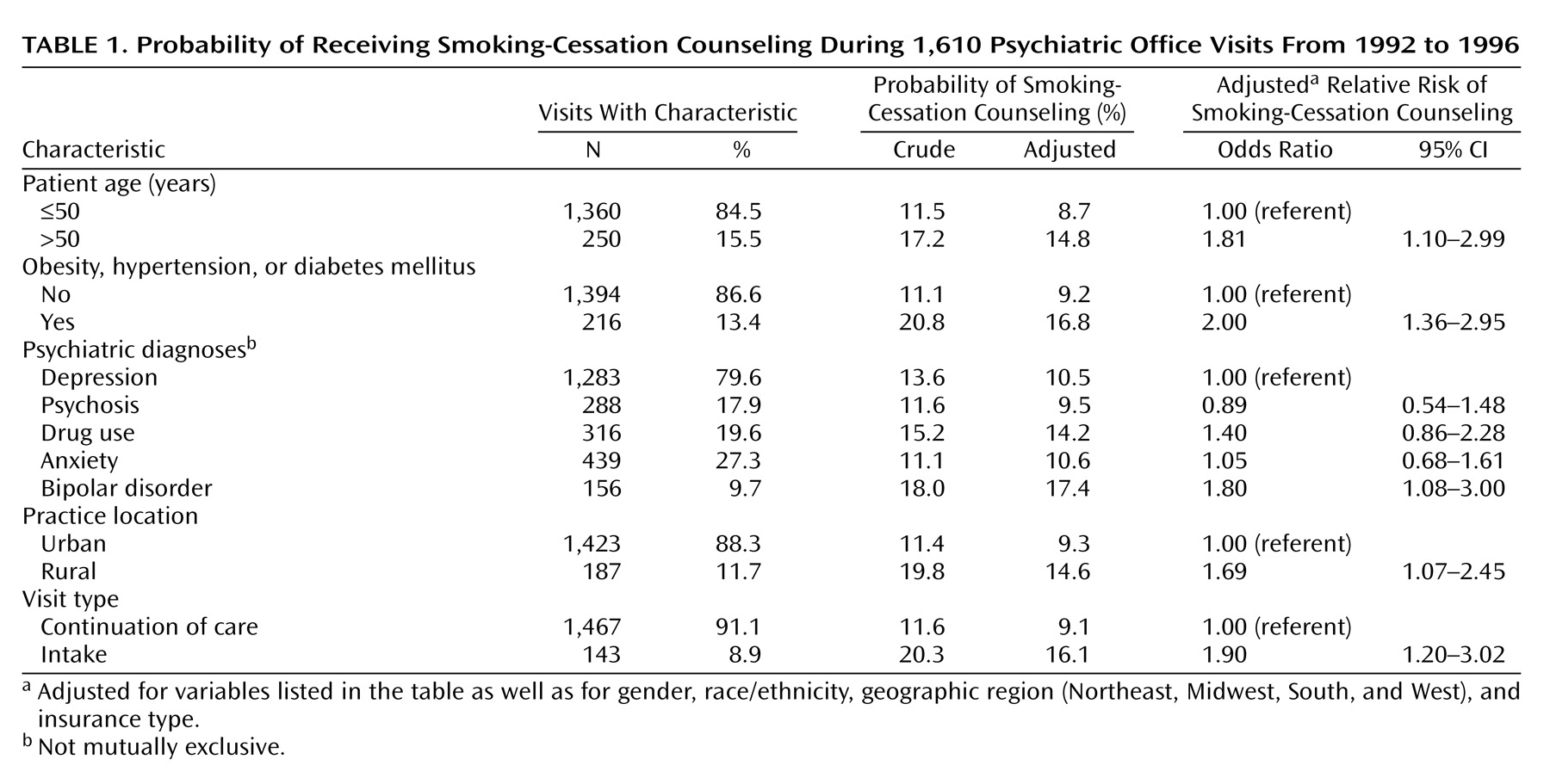
Psychiatrists offered smoking-cessation counseling at 12.4% (N=200) of the visits. The adjusted probability of receiving smoking-cessation counseling was significantly higher (p<0.05) for those with the following characteristics compared to those without: age greater than 50 (14.8% versus 8.7%); a medical diagnosis of obesity, hypertension, or diabetes mellitus (16.8% versus 9.2%); residence in a rural location (14.6% versus 9.3%); and having an initial visit (16.1% versus 9.1%). Compared to those with a depressive disorder, only those with bipolar affective disorder were significantly more likely to receive smoking-cessation counseling (17.4% versus 10.5%). The magnitudes of association seen when comparing those with a characteristic to those without a characteristic were reflected in adjusted odds ratios and are presented in
Table 1. Stratified analyses based on the presence or absence of psychotherapy or visit length did not alter these findings. Neither nicotine gum nor the transdermal nicotine patch was prescribed at any patient visit for smokers. Psychiatrists did not use the diagnosis of nicotine dependence at any patient visit. Subsequent analysis using generalized estimation equations did not change the results.
Discussion
In this cross-sectional study of a national sample of office-based psychiatric visits, we found that psychiatrists offered smoking-cessation counseling at 12.4% of the visits to psychiatric patients who smoked. In comparison, primary care physicians were reported to offer smoking-cessation counseling to 19% of psychiatric patients with substance abuse disorders and 30% with anxiety and depressive disorders
(5,
11). With respect to other health behaviors, we found that psychiatrists offered diet counseling at 6% of patient visits and exercise counseling at 4% of visits.
Our findings also suggest that smoking-cessation counseling is more likely to be offered at visits with older individuals and visits with individuals diagnosed with medical conditions that increase the risk for cardiovascular disease. This is in keeping with previous research that suggests physicians are more likely to counsel smokers that are at a higher risk for developing smoking-related medical conditions such as coronary artery disease
(11). Our finding that smoking-cessation counseling is more likely to be offered at patient visits in rural communities and at patient visits for the treatment of bipolar affective disorders may be indicative of the “primary care” role that psychiatrists may assume in these situations for patients at high risk of developing tobacco dependence
(12). Finally, our findings suggest that psychiatrists may need to be more vigilant about offering smoking-cessation counseling on follow-up patient visits.
This study has several limitations. First, the study’s time period (1992–1996) may not adequately reflect current clinical practice. For example, we were unable to investigate the impact of APA’s
Practice Guideline for the Treatment of Patients With Nicotine Dependence (6) or alternative nicotine treatments, such as bupropion therapy, because these interventions were not available during this time period. However, given the minimal change in the prevalence of smoking in the general population in last decade and continued calls for physicians to improve the rates of smoking counseling, we believe our findings are still relevant. In addition, some studies have estimated the prevalence of smoking in psychiatric populations to be as high as 40%
(2), so the estimate of smoking in this study may be somewhat underestimated. However, because we found that the prevalence of smoking is twice as high as in National Ambulatory Medical Care Survey studies of the general population, we believe that our results have face validity. Finally, because the diagnosis of nicotine dependence was not specifically used, it is possible that psychiatrists saw their role as advising a health habit, not treating a mental disorder.
The National Ambulatory Medical Care Survey data is also limited in that we are unable to account for the length of time or the amount of cigarettes smoked by a patient at a psychiatric visit nor to investigate the effect of visit acuity on the receipt of smoking-cessation counseling. Moreover, because the unit of analysis for this study is a cross-section of patient visits, we are unable to say whether or not a psychiatrist offered counseling at previous visits. Although the National Ambulatory Medical Care Survey data are adjusted to account for the sample of physicians who did not participate in the study, it is possible that a nonresponse bias may still exist.
We also are limited by a small sample size in investigating how current coronary artery disease or chronic obstructive pulmonary disease may influence a psychiatrist to offer smoking-cessation counseling.
In summary, although psychiatrists have higher odds of offering smoking-cessation counseling to certain high-risk subgroups, they may be missing significant opportunities to offer smoking-cessation counseling to their patients who smoke. Interventions to increase awareness of smoking-cessation counseling by psychiatrists may be warranted.