Clinical and experimental data suggest a role of the respiratory system in the pathophysiology of panic disorder. This has led to the idea that disorderly respiratory control mechanisms may underlie the occurrence of panic attacks
(1,
2). Despite the evidence for a connection between panic attacks and respiration, the nature of respiratory abnormalities remains unclear. Some studies have shown higher respiratory frequency, tidal volume, and minute ventilation and lower baseline end-tidal CO
2 levels in patients with panic disorder than in patients with other anxiety disorders and healthy comparison subjects
(3–
5), whereas other studies have not confirmed these results
(6,
7).
In order to clarify the nature of respiratory abnormalities in panic disorder, we investigated the baseline respiratory functioning of a group of patients with panic disorder and healthy comparison subjects. Since biological systems are characterized by dynamic processes with extensive interactions between multiple inputs, nonlinear methods are considered the gold standard for measuring the complexity of physiological functions
(14). Each physiological signal, such as respiratory or cardiac, usually represents the output of complex mechanisms, including multiple feedback/coupling interactions and inputs from internal and external sources. The moment or linear statistics, such as mean and standard deviation, are unable to analyze the dynamics of complex physiological signals, whereas nonlinear statistics unravel highly significant differences in circumstances in which the former do not distinguish between groups. Many studies
(15–
18) have demonstrated that nonlinear measures, including fractal dimension, correlation dimension, largest Lyapunov exponent, and approximate entropy, are more valuable than linear measures for studying variability in heart rate. We used the approximate entropy index, a nonlinear measure of irregularity, to study the dynamics of baseline breathing patterns in our subjects. The approximate entropy index has been widely used to study endocrine function
(19–
21), heart rate
(22–
24), and respiratory physiology
(25). We know of only three studies
(26–
28) to date that have analyzed data on psychiatric patients by means of the approximate entropy index.
The aim of this study was to unravel possible differences in the breath-by-breath complexity of respiration dynamics between patients with panic disorder and healthy subjects. The contribution of sighing to the irregularity of breathing patterns was assessed. The effect of variables that might influence breathing patterns was also evaluated.
Results
For the patients with panic disorder, the mean illness duration was 7.1 years (SD=7.9). Twenty-eight patients (70%) were agoraphobic. The mean total score on the Panic-Associated Symptom Scale was 7.0 (SD=4.1), and the mean scores on the panic attack, anticipatory anxiety, and agoraphobia subscales were 3.5 (SD=2.5), 2.3 (SD=2.0), and 0.6 (SD=0.9), respectively. The mean total score on the Fear Questionnaire was 45.7 (SD=24.5), and the mean scores on the agoraphobia, blood-injury phobia, and social phobia subscales were 14.7 (SD=12.8), 18.8 (SD=12.0), and 12.2 (SD=8.1), respectively.
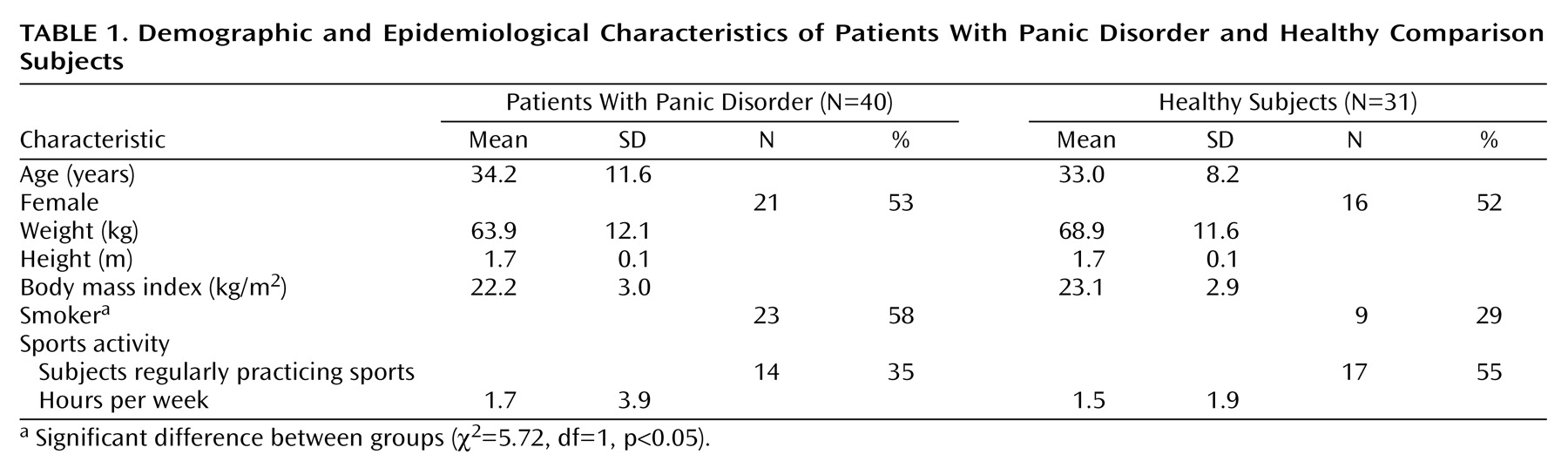
There were no significant differences between the two groups in gender distribution, age, weight, height, body mass index, number of subjects who regularly practiced sports, and hours of sports activity per week, whereas there were significantly more smokers among the panic disorder patients than among the healthy comparison subjects (
Table 1).
ANOVA showed that the patients with panic disorder had significantly higher baseline anxiety levels, as measured by the State-Trait Anxiety Inventory, before assessment of respiratory physiology (mean score=45.6, SD=11.6) than the healthy comparison subjects (mean=29.2, SD=4.1) (F=56.8, df=1, 69, p<0.01). The mean scores on the visual analogue scale for anxiety before respiratory assessment in the patients with panic disorder and the comparison subjects were 36.5 (SD=25.3) and 7.0 (SD=8.7), respectively. During assessment they were 31.7 (SD=27.1) and 4.1 (SD=5.6). After respiratory assessment they were 22.9 (SD=24.9) and 2.7 (SD=4.7). ANOVA for repeated measures showed significant effects of diagnosis (F=43.0, df=1, 68, p<0.01) and time (F=8.1, df=2, 138, p<0.01) in the visual analogue scale scores, while no significant time-by-diagnosis interaction was found.
Baseline Anxiety
A MANCOVA with the State-Trait Anxiety Inventory score as covariate showed no significant differences in the mean values of any of the respiratory parameters between the patients with panic disorder and the healthy comparison subjects. The mean respiratory rates were 16.53 (SD=4.04) and 16.33 (SD=3.72) breaths/minute, respectively; the mean tidal volumes were 0.55 (SD=0.20) and 0.51 (SD=0.17) liter; the mean minute ventilations were 8.53 (SD=2.98) and 7.87 (SD=2.13) liters/min; the mean ratios of tidal volume to time in inspiration were 0.38 (SD=0.13) and 0.34 (SD=0.10); the mean P
co2 values were 32.43 (SD=4.60) and 32.89 (SD=3.07) mm Hg; the mean ratios of minute ventilation to P
co2 were 0.27 (SD=0.16) and 0.24 (SD=0.07); and the mean ratios of minute ventilation to P
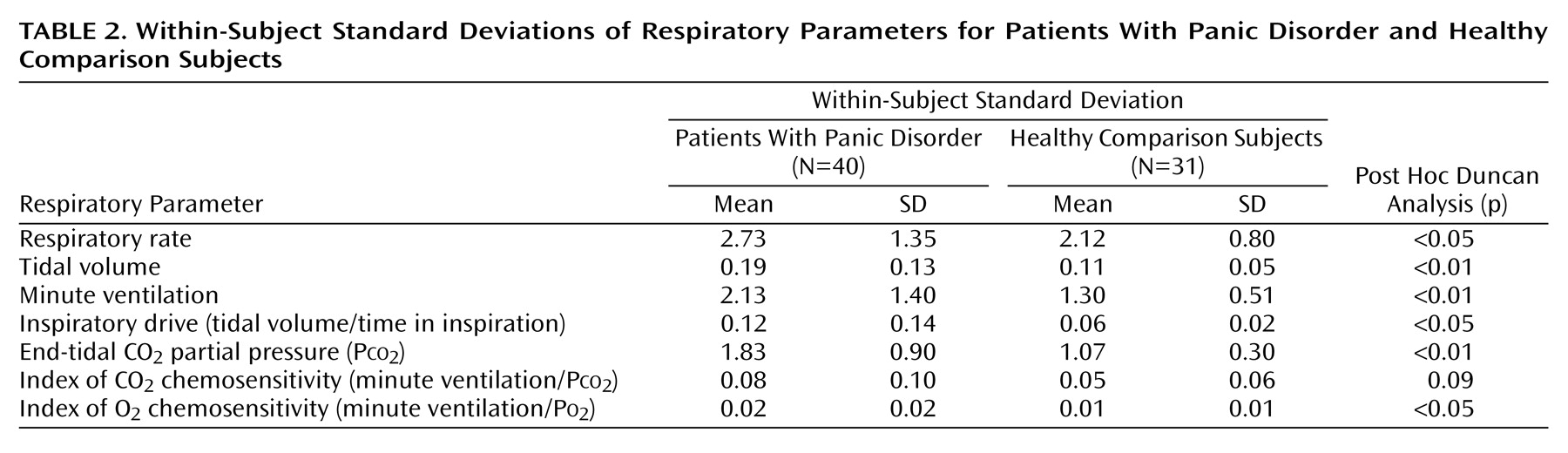
o2 were 0.08 (SD=0.03) and 0.07 (SD=0.02). However, significantly higher average within-subject standard deviations were observed in the patients with panic disorder than in the comparison subjects (R=3.2, df=7, 62, p<0.01). Post hoc Duncan comparisons showed significantly higher standard deviations in the patients with panic disorder for all respiratory parameters except the ratio of minute ventilation to P
co2 (
Table 2).
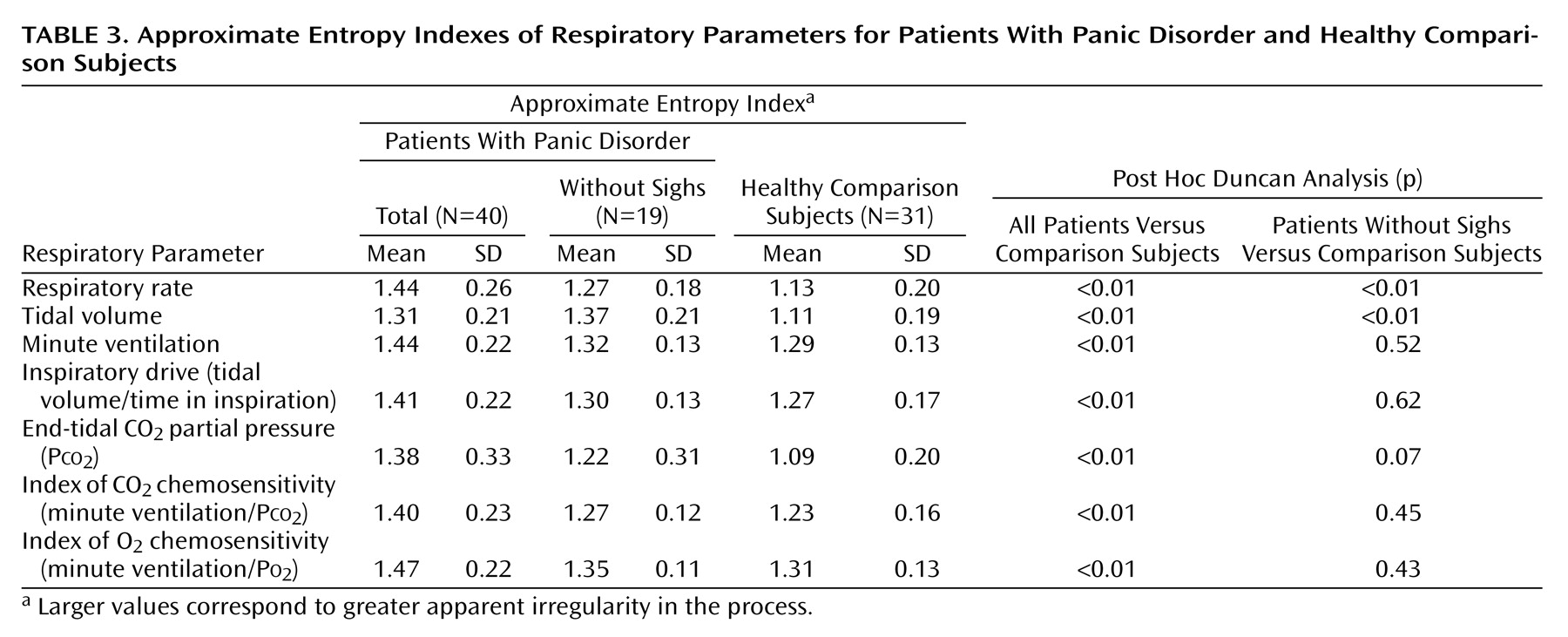
A MANCOVA with the State-Trait Anxiety Inventory score as covariate showed significantly higher approximate entropy indexes of the baseline respiratory parameters in the patients than in the comparison subjects (R=2.6, df=7, 62, p<0.02). Post hoc Duncan comparisons showed significantly higher indexes in the patients with panic disorder than in the healthy comparison subjects for all respiratory parameters (
Table 3).
Similar results were obtained when the score on the visual analogue scale for anxiety before respiratory assessment was included as a covariate in the MANCOVA (data available on request).
Gender
A MANCOVA with the State-Trait Anxiety Inventory as a covariate and diagnosis and gender as grouping factors showed significant gender effects for the mean values of the respiratory parameters (R=6.0, df=7, 60, p<0.01), whereas no significant diagnosis effect or diagnosis-by-gender interaction was found. The male subjects showed significantly higher mean values for tidal volume, minute ventilation, tidal volume/time in inspiration, Pco2, and minute ventilation/Po2 than the female subjects (post hoc Duncan comparisons, p<0.01 for all measures), whereas the mean values for respiratory rate and minute ventilation/Pco2 were not significantly different (data available on request). A MANCOVA with the State-Trait Anxiety Inventory score as a covariate and diagnosis and gender as grouping factors showed a diagnosis effect for the standard deviations (R=3.0, df=7, 60, p<0.01) and approximate entropy indexes (R=2.5, df=7, 60, p<0.05) but did not show either a significant gender effect or a diagnosis-by-gender interaction for the standard deviations or approximate entropy indexes of any respiratory parameter.
Smoking
A MANCOVA with the State-Trait Anxiety Inventory as covariate and diagnosis and smoking as grouping factors showed a significant diagnosis effect for the standard deviations (R=2.5, df=7, 60, p<0.05) and approximate entropy indexes (R=2.2, df=7, 60, p<0.05) but not for the mean values of the respiratory parameters. No significant effect of smoking on the mean values, standard deviations, or approximate entropy indexes for any respiratory parameter was found. No significant diagnosis-by-smoking interaction was found for the mean values or approximate entropy indexes of any respiratory parameter, whereas a significant effect on the standard deviations was found (R=2.5, df=7, 60, p<0.05). Post hoc Duncan comparisons showed higher standard deviations in smoking patients with panic disorder than in smoking comparison subjects for respiratory rate (mean=3.08, SD=1.58, and mean=1.63, SD=0.48, respectively) (p<0.01), tidal volume (mean=0.18, SD=1.11, and mean=0.01, SD=0.05, respectively) (p<0.05), minute ventilation (mean=2.27, SD=1.37, and mean=1.17, SD=0.41, respectively) (p<0.01), Pco2 (mean=1.94, SD=0.91, and mean=1.17, SD=0.44, respectively) (p<0.01), minute ventilation/Po2 (mean=0.03, SD=0.03, and mean=0.01, SD=0.00, respectively) (p<0.05), and tidal volume/time in inspiration (mean=0.10, SD=0.07, and mean=0.05, SD=0.02, respectively) (p<0.01).
Sports
A MANCOVA with the State-Trait Anxiety Inventory score as covariate and diagnosis and sports as grouping factors showed a significant diagnosis effect for the standard deviations (R=3.4, df=7, 60, p<0.05) and approximate entropy indexes (R=2.3, df=7, 60, p<0.05) but not for the mean values of the respiratory parameters. No significant sports effect or diagnosis-by-sports interaction for mean values, standard deviations, or approximate entropy indexes of any respiratory parameter was found.
Clinical Characteristics
Linear Pearson correlation did not show any significant correlation between the approximate entropy index of any respiratory parameter and illness duration or severity of clinical symptoms, measured by the global and subscale scores on the Panic-Associated Symptom Scale and the Fear Questionnaire.
Sighs
A t test showed a higher number of sighs by the patients with panic disorder than by the healthy comparison subjects (mean=4.6, SD=6.8, and 0, respectively) (t=3.8, df=69, p<0.01). Twenty-one patients (53%) with panic disorder made sighs, whereas 19 (48%) did not. None of the healthy subjects had sighs in their breathing patterns. There were no significant differences in gender distribution, age, weight, height, body mass index, number of subjects who regularly practiced sports, hours of sports activity per week, illness duration, or severity of clinical symptoms between the patients with sighs and without sighs.
We compared the mean values, standard deviations, and approximate entropy indexes for all respiratory parameters in the patients with sighs, patients without sighs, and comparison subjects. A MANCOVA with the State-Trait Anxiety Inventory score as covariate showed no significant difference in the mean values of any respiratory parameter among the three groups. A MANCOVA with the State-Trait Anxiety Inventory score as covariate showed a significant group effect for the standard deviations (R=6.7, df=14, 122, p<0.01). Post hoc Duncan comparisons showed higher standard deviations in the patients with sighs than in the comparison subjects for all respiratory parameters (p<0.01), higher standard deviations in the patients with sighs than in patients without sighs for respiratory rate, tidal volume, minute ventilation, and Pco2 (p<0.01), but no difference between the patients without sighs and comparison subjects in any respiratory parameter (data available on request).
A MANCOVA with the State-Trait Anxiety Inventory score as covariate showed a significant group effect for the approximate entropy indexes (R=4.4, df=14, 122, p<0.01). Post hoc Duncan comparisons showed higher approximate entropy indexes in the patients with sighs than in the comparison subjects for all respiratory parameters (p<0.01), higher indexes in the patients with sighs than in the patients without sighs for respiratory rate (mean=1.62, SD=0.16, and mean=1.27, SD=0.18, respectively) (p<0.01), minute ventilation (mean=1.59, SD=0.17, and mean=1.32, SD=0.13) (p<0.01), P
co2 (mean=1.58, SD=0.16, and mean=1.22, SD=0.31) (p<0.01), minute ventilation/P
o2 (mean=1.62, SD=0.16, and mean=1.35, SD=0.11) (p<0.01), minute ventilation/P
co2 (mean=1.55, SD=0.18, and mean=1.27, SD=0.12) (p<0.01), and tidal volume/time in inspiration (mean=1.54, SD=0.18, and mean=1.30, SD=0.13) (p<0.01), and higher indexes in the patients without sighs than in the comparison subjects for respiratory rate and tidal volume (
Table 3). Similar results were obtained by defining a sigh as 2.0 times the mean tidal volume, according to the definition used by Wilhelm and co-workers
(13) (data available on request).
In the patients with sighs, the linear Pearson correlation did not show any significant correlation between the approximate entropy index for any respiratory parameter and the number of sighs.
None of the tested subjects experienced panic attacks or asked to stop the recording during assessment of respiratory physiology.
Discussion
The main finding of our study is that patients with panic disorder had significantly higher approximate entropy indexes and higher average within-subject standard deviations than healthy comparison subjects for the measured respiratory parameters, whereas the mean values did not discriminate between the two groups. Our findings suggest that patients with panic disorder have not only greater overall variability but also greater entropy in baseline respiratory patterns, indicating greater irregularity and complexity in their respiratory functioning. This is in agreement with recent findings of higher values for approximate entropy and the largest Lyapunov exponent, a measure of chaos, for lung volume in patients with panic disorder than in normal subjects
(27).
Baseline anxiety was greater in the patients than in the comparison subjects but was not able to explain our respiratory findings. Moreover, the scores on the visual analogue scale for anxiety during the procedure decreased similarly in the two groups, indicating that the procedure was no more anxiogenic for the patients than for the comparison subjects. Severity of illness did not influence the irregularity of the respiratory pattern either. Other variables that could influence respiratory pattern, i.e., age, weight, height, and body mass index, did not differ between the patients and comparison subjects.
The male subjects had higher mean values of some respiratory measures than the female subjects, as expected from the physiological difference in body mass
(32), whereas no differences were found for respiratory patterns. Sports activity did not influence the measured respiratory parameters. As in epidemiological studies
(42), smokers were more prevalent among the patients with panic disorder than among the comparison subjects. The smoking patients with panic disorder had greater variability in some respiratory parameters than smoking comparison subjects, but they did not differ on the irregularity of their breathing patterns. In brief, the main somatic and individual variables related to respiration are unable to explain the difference in respiratory pattern found.
Approximate Entropy and Sighs
Our findings do not completely overlap with those of studies that showed greater irregularity of tidal volume due to frequent sighs in patients with panic disorder
(8,
10,
11,
13). In our study, the patients with panic disorder showed significantly more sighs than the healthy subjects, but the presence of sighs does not fully explain the irregularity in breathing patterns. Although the patients with sighs showed higher approximate entropy indexes for the respiratory parameters, except for tidal volume, than the patients without sighs, the latter showed significantly higher indexes for respiratory rate and tidal volume than the healthy subjects. These findings suggest that sighs contribute to the irregularity of breathing patterns but do not account for all of the differences in approximate entropy between patients with panic disorder and healthy subjects. At least for the two main respiratory parameters, respiratory rate and tidal volume, the irregularity of breathing patterns in patients with panic disorder is not attributable to the presence of sighs. Moreover, the lack of correlation between the approximate entropy index for any respiratory parameter and the number of sighs supports the possibility that sighs do not fully explain the irregularity of the patterns for the other respiratory parameters.
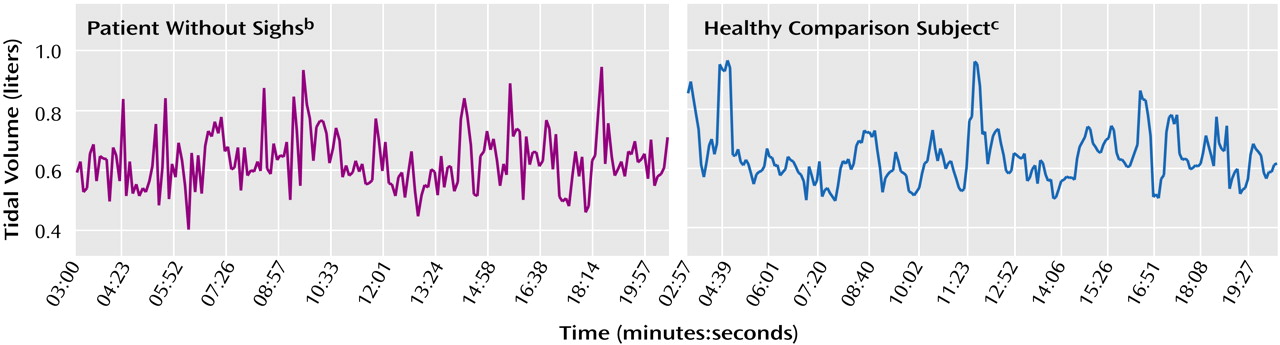
Unlike the approximate entropy indexes, the standard deviations for all the respiratory parameters did not differ between the patients without sighs and the comparison subjects. This finding confirms that a linear measure of variability is unable to fully discriminate between patients and healthy subjects for a highly complex function such as respiration, whereas a nonlinear measure does so (
Figure 1).
The role of sighs in patients with panic disorder is unclear. Since the sighs have a physiological function in maintaining normal lung volumes and reducing unpleasant respiratory sensations
(43), they could be a mechanism that compensates for the abnormal respiratory functioning of patients with panic disorder. Alternatively, the sighs could be an expression of greater abnormality in the functioning of the rhythm-generating respiratory network (see the following). Further studies are necessary to clarify these issues.
Implications of Approximate Entropy for Pathophysiology of Panic Disorder
Entropy characterizes the amount of randomness or disorder in processes and systems. Living organisms have been described as highly complex and dynamic structures that display a meta-equilibrium around homeostatic levels, oscillating between order and disorder
(44,
45). External or internal perturbations can lead a biological system to a state with a high degree of instability, defined as a “bifurcation point,” from which the system may proceed to diverging states, such as a new level of order or, on the contrary, to a “disruption,” such as a pathological phenomenon
(46). The greater entropy in the respiratory functioning of patients with panic disorder may indicate an intrinsic instability state in respiratory homeostasis on which different critical inputs could act as “disrupting” factors leading to panic attacks. Respiratory instability may underlie the susceptibility of patients with panic disorder to hypercapnic challenges
(1).
The question of whether greater respiratory entropy could be a consequence of panic disorder or a trait marker of vulnerability to panic disorder is open, but two studies support the latter hypothesis. Coryell and co-workers
(47) reported abnormal respiratory patterns in healthy first-degree relatives of patients with panic disorder breathing a 5% CO
2 gas mixture. Preliminary data from our team
(48) showed greater approximate entropy in the baseline respiratory patterns of healthy children of patients with panic disorder than in the children of healthy subjects. Instability in respiratory systems might lead to the onset of the disease when the system fails to cope with the stimuli and fails to restore the state of equilibrium. Daily tobacco smoking increases the risk for onset of panic attacks and disorder
(42). Since nicotine seems to modulate neurotransmission in the respiratory brainstem network
(49), an intrinsic respiratory instability might underlie the development of the disorder after the onset of smoking.
The source of greater respiratory entropy in patients with panic disorder is unclear. Respiration is modulated by a complex regulatory system in which the brainstem plays a central role in containing the pacemaker respiratory neurons and the neural network that shape respiratory patterns
(50). Irregularity in breathing patterns might arise from abnormal functioning of the rhythm-generating network, leading to a lack of physiological synchronicity in inspiratory and expiratory neuron activity. Since limbic and cortical areas influence respiration
(51,
52), physiological instability could also originate from brain centers higher than the brainstem. However, the role of higher centers is called into question by the absence of an influence of state anxiety on respiration instability and by the reported lack of influence of cognitive manipulation on doxapram-induced irregularity in tidal volume in patients with panic disorder
(11).
The greater respiratory irregularity might also influence the heart rate of patients with panic disorder. Several studies have demonstrated less variability in heart rate in patients with panic disorder
(53–
55), and one study has shown less chaos in a heart rate time series
(56). Since cardiac activity is regulated by direct connections between respiratory and sympathetic/vagal cardiac centers within the brainstem, abnormal functioning of the respiratory network could affect the autonomic regulation of cardiac activity, leading to abnormal modulation of the heart rate.
Finally, the greater respiratory entropy in patients with panic disorder does not necessarily imply a specific intrinsic instability in the respiratory system, but it might arise from a more global abnormality in the brainstem neuronal circuits regulating physiological homeostasis functions
(57). This idea is supported by the observation that patients with panic disorder show subclinical abnormalities in the functioning of the balance system
(58).
In conclusion, this study shows greater irregularity and complexity in the respiratory functioning of patients with panic disorder. This finding supports the idea of abnormal regulation of the respiratory system as a key mechanism in panic disorder. Greater respiratory entropy could represent a vulnerability factor for panic attacks. Further studies are necessary to confirm the specificity of the results, comparing patients with panic disorder and patients with other anxiety disorders. Identification by brain imaging of specific brain structures related to this abnormal respiration feature could help to build a much-needed neuroanatomical model of “respiratory” panic.