Extended Meth Abstinence Boosts Memory and Motor Skills
Methamphetamine is a commonly abused drug. With protracted abstinence from methamphetamine, the brain appears to recover some of its lost dopamine transmission. To determine whether the improvement is widespread and whether it translates into better mental performance, Wang et al. (p. 242) measured brain metabolism and cognitive ability in former methamphetamine users within 6 months of detoxification and again at 1 year. Between these times, metabolism improved significantly in the thalamus, where incoming information is filtered and passed to other brain regions. The improvement in metabolism correlated with improved performance on motor and memory tasks. In the users with at least 9 months’ abstinence, thalamic metabolism was similar to that of healthy subjects without drug use. Long-term abstinence, however, did not increase metabolism in the striatum and nucleus accumbens, which may account for the persistent lack of motivation and pleasure in detoxified methamphetamine users.
Depression Morphs Between Episodes
Most people who have an episode of major depression have a recurrence later. The recurrence is likely to take a different form though, report Oquendo et al. (p. 255). Patients hospitalized for severe depression who remained well for 2 months were reassessed at 3, 12, and 24 months. Among the 78 who had a recurrence, only a few symptoms were consistent between episodes, and the correlations were modest. Even the depression subtype (melancholic, psychotic, or atypical) was likely to be different in the second episode. Such variation suggests that separate episodes of depression may be considered different manifestations of the disorder and that subtype can differ within, as well as between, individuals. A change in subtype also has practical implications, since certain subtypes appear to respond preferentially to specific treatments.
Mapping Schizophrenic Properties in the Thalamus
Because the thalamus acts as a switchboard in the brain, it may be critical to the disrupted circuitry believed to underlie schizophrenia. The multiple nuclei of the thalamus have unique individual connections to other brain areas and may hold clues to the mechanisms of schizophrenia. Hazlett et al. (p. 305) measured metabolism in three nuclei—mediodorsal nucleus, pulvinar, and centromedian nucleus. Patients with schizophrenia had lower metabolism in the mediodorsal nucleus and centromedian nucleus than did healthy subjects. Both regions have connections to the prefrontal cortex, and higher metabolism in the mediodorsal nucleus correlated with better verbal learning by the patients. Lower metabolism in the pulvinar of the patients was associated with more hallucinations and other positive symptoms, whereas lower activity in the mediodorsal nucleus was related to more severe negative symptoms.
How Seniors Can Kick the Sleeping Pill Habit
The incidence of insomnia increases with age, as does use of sleeping medications. Prolonged use is common but creates the potential for numerous adverse effects. Benzodiazepines are a particular danger for the elderly. Discontinuation of benzodiazepines, however, also poses physiological and psychological risks. To minimize these pitfalls, Morin et al. (p. 332) combined 10 weeks of supervised drug tapering and cognitive behavior therapy for elderly patients who had already tried numerous times to stop taking benzodiazepines for insomnia. At the end of treatment, 85% of the patients were drug free, compared to 54% of patients receiving only cognitive behavior therapy and 48% of those doing drug tapering only. At 12-month follow-up, the rates were 70%, 42%, and 65%, respectively. Adding cognitive behavior therapy to drug tapering helped alleviate insomnia, and sleep improvements became more noticeable after several months.
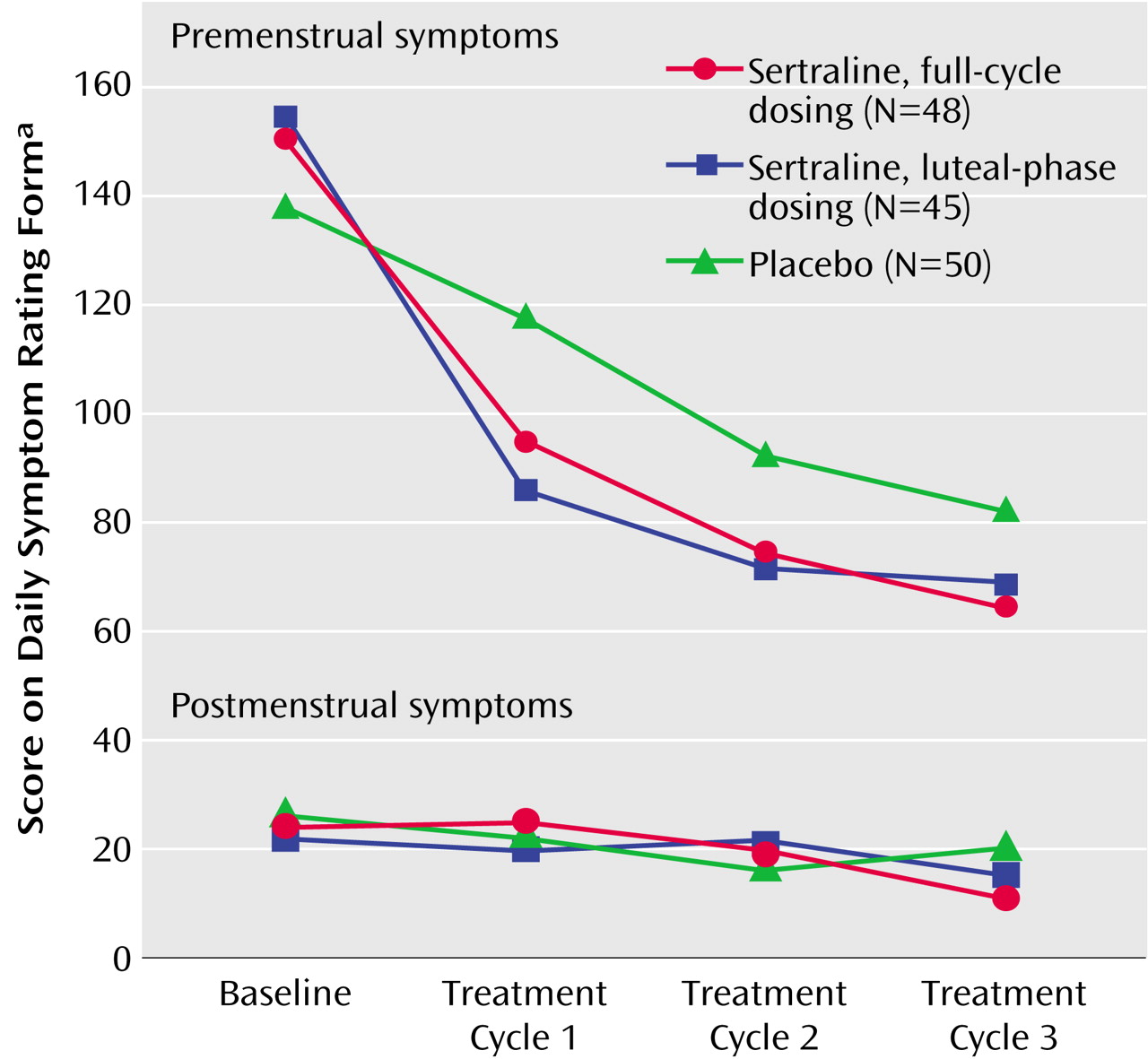
For PMS, Is Part-Time Medication Better?
Either continuous or premenstrual treatment with a selective serotonin reuptake inhibitor is effective in treating severe premenstrual syndrome (PMS). If one of these dosing methods has an advantage in reducing symptoms or minimizing side effects, many women could function even better. Freeman et al. (p. 343) compared continuous sertraline treatment with intermittent dosing: from day 14 of the menstrual cycle to day 2 of the next cycle. For women with premenstrual dysphoric disorder or near-threshold cases, the two dosing regimens were superior to placebo and similar to each other in reducing symptoms. Adjustment to the medication may have been greater in women receiving continuous sertraline; by the third month their adverse effects were no worse than those with placebo. Women receiving intermittent dosing, who stopped and restarted sertraline treatment each month, continued to have more adverse effects than the placebo group. Still, intermittent dosing offers less drug exposure and may be preferred by women with tolerable side effects.
Images in Psychiatry
Sigmund Freud, 1856–1939 (p. 232)