Poststroke depression occurs in approximately one-third of all ischemic stroke survivors and has been linked to worse functional outcome, slower recovery, and worse quality of life
(1–
3). Prior studies have also linked depression or depressive symptoms to increased mortality for up to 10 years after a stroke, although many of these studies are limited by selection bias, small sample size, and absence of a definitive depression diagnosis
(4–
8). Further, depression may not exist in a vacuum after a stroke: other mental health conditions may also be present, and few studies have examined whether these diagnoses confer additional mortality risk. Knowing which mental health diagnoses are linked to higher poststroke mortality may provide better mortality risk prediction and may encourage clinicians to identify and treat these conditions more aggressively. The objective of this study was to evaluate the effect of poststroke depression and other mental health diagnoses on survival after hospitalization for ischemic stroke in a national cohort of veterans.
Method
We used U.S. Department of Veterans Affairs (VA) administrative databases to construct a national cohort of patients discharged from any VA medical center with a primary diagnosis of ischemic stroke, defined as ICD-9 codes 434 and 436 in the primary position. This strategy has at least 90% positive predictive value for identifying cases of acute ischemic stroke
(9). Patients were eligible for inclusion in the database if they were discharged between October 1, 1990, and September 30, 1997. Patients hospitalized at VA medical centers in Puerto Rico and the U.S. Virgin Islands were excluded. For veterans with more than one admission for stroke, the first admission was considered the index event. Since DSM-IV requires depressive symptoms to be present for at least 2 weeks, we excluded stroke patients who died within 30 days of their index stroke event from this study to ensure the depression diagnosis was received poststroke (N=4,974 excluded).
From the centralized VA administrative data center we extracted demographic characteristics and summary information about episodes of inpatient care, including up to 10 ICD-9-CM diagnosis codes at discharge from the index hospitalization. We used these discharge diagnoses to construct the Charlson Index, a well-validated comorbidity index that is predictive of subsequent mortality
(10,
11).
We used ICD-9 codes associated with episodes of care within 3 years poststroke to divide patients into three nonoverlapping groups: 1) those with poststroke depression, 2) those with a mental disorder or substance abuse diagnosis other than depression, and 3) those with no poststroke psychopathology. Patients diagnosed with depression comorbid with another mental disorder or substance abuse diagnosis were classified in the depressive group. Diagnosis of depression in the first 3 years poststroke was defined using ICD-9 codes 296, 298, 300.4, 309.0, 309.1, and 311. Patients with a depression ICD-9 code at index hospitalization discharge were not classified in the poststroke depression group, since these patients may have had a preexisting depression diagnosis that may or may not have been clinically symptomatic at the time of their stroke. Other mental health diagnoses were identified using ICD-9 codes for schizophrenia, major affective disorder other than depression, anxiety disorders, personality disorders, and substance abuse and dependence (list of ICD-9 codes available on request).
One potential variable of interest that may influence both the development of poststroke depression and mortality is severity of stroke. Since the national Veterans Health Administration database did not include any indicator of stroke severity, we reviewed charts of all ischemic stroke patients at our local VA medical center who were also in the national dataset. We matched each of the local patients with an ICD-9 diagnosis of poststroke depression with one local patient with another mental disorder or substance abuse diagnosis and up to three local patients with no poststroke psychopathology. All comparison patients were matched for patient age and year of stroke. We then used a previously published algorithm to abstract the written admission notes and construct a retrospective National Institutes of Health (NIH) Stroke Scale
(12). We used this local subset of the national database to examine the effect of admission stroke severity on poststroke mortality.
Date of death was identified through the Beneficiary Information and Resource Locator, which does not contain information regarding the cause of death. No pharmacy data were available during the study period. Data were merged by using scrambled social security numbers and date of discharge from the index stroke admission to construct patient-level data files. This project was approved by the local institutional review board.
We compared the groups of patients with poststroke depression, other mental disorder or substance abuse diagnoses, and no poststroke psychopathology by using analysis of variance. To examine time to death, defined as the number of days between discharge from the index admission and death, we developed Cox proportional hazards models. The following independent variables were included: age, gender, ethnicity (white versus nonwhite), hypertension, diabetes, coronary artery disease, congestive heart failure, hyperlipidemia, atrial fibrillation, number of discharge diagnoses, Charlson Index >2 (dichotomous), presence of depression (yes/no), and presence of other mental health or substance abuse diagnosis (yes/no). To evaluate the possibility of a cohort effect, we also examined models including a variable for year of index admission. Since including this variable did not alter hazard ratios or confidence intervals by more than 0.005, the models presented do not include year of index admission as an independent variable.
Results
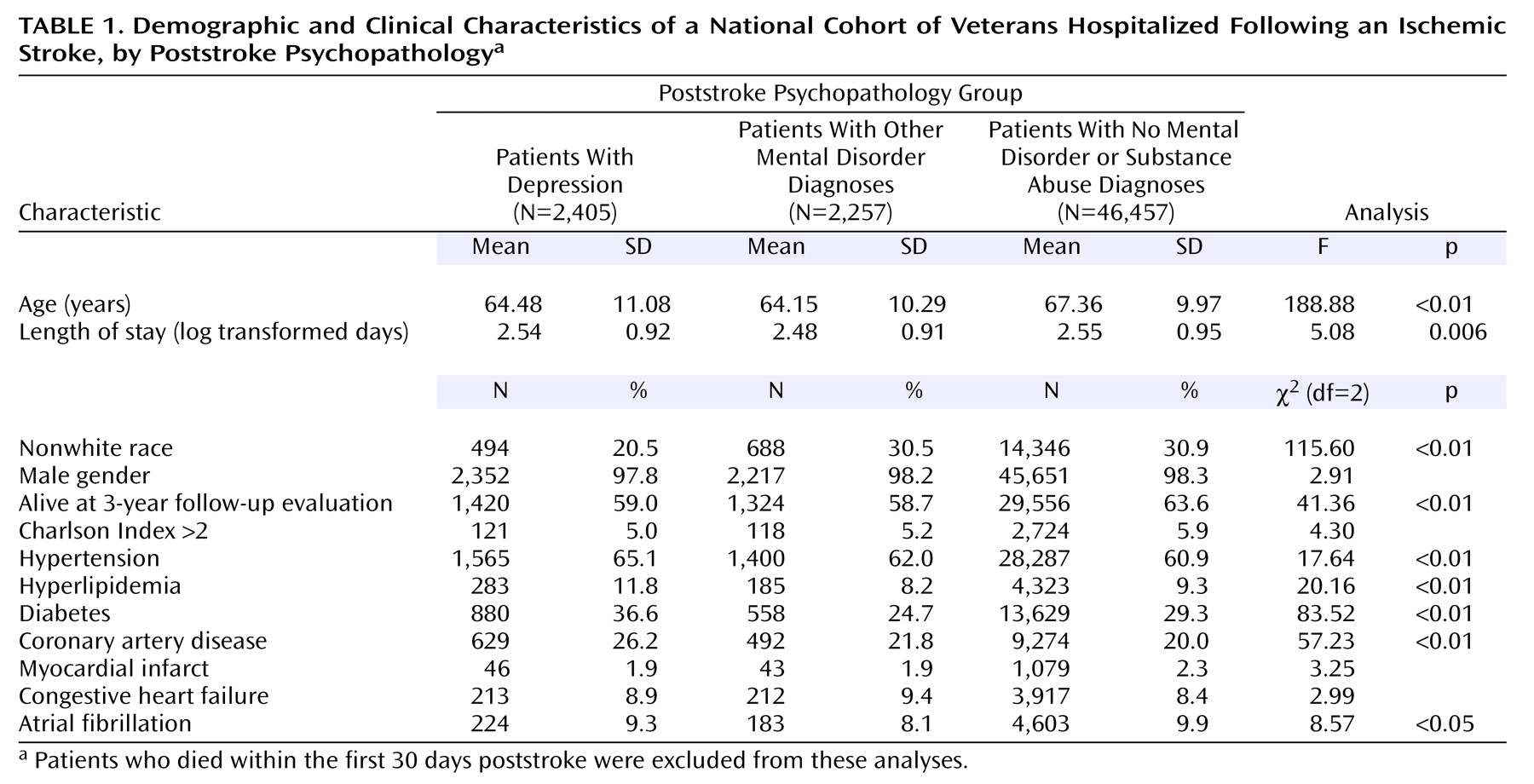
We identified 51,119 patients hospitalized following an ischemic stroke who survived beyond 30 days afterward, of whom 2,405 (4.7%) received an ICD-9 diagnosis of depression and 2,257 (4.4%) received other mental disorder or substance abuse diagnoses within 3 years of their index admission (
Table 1). Relative to those with no poststroke psychopathology, those with poststroke depression were younger and were less likely to be alive at the end of the follow-up period. Patients diagnosed with poststroke depression were more likely to be white relative to those with other mental disorder or substance abuse diagnoses and the no poststroke psychopathology group. The other mental disorder or substance abuse diagnosis cohort consisted of 1,369 veterans with substance abuse, 785 with anxiety disorders, 264 with schizophrenia, 207 with personality disorders, and 136 with other affective disorders. The raw numbers sum to more than 2,257 because some veterans had more than one mental disorder or substance abuse diagnosis.
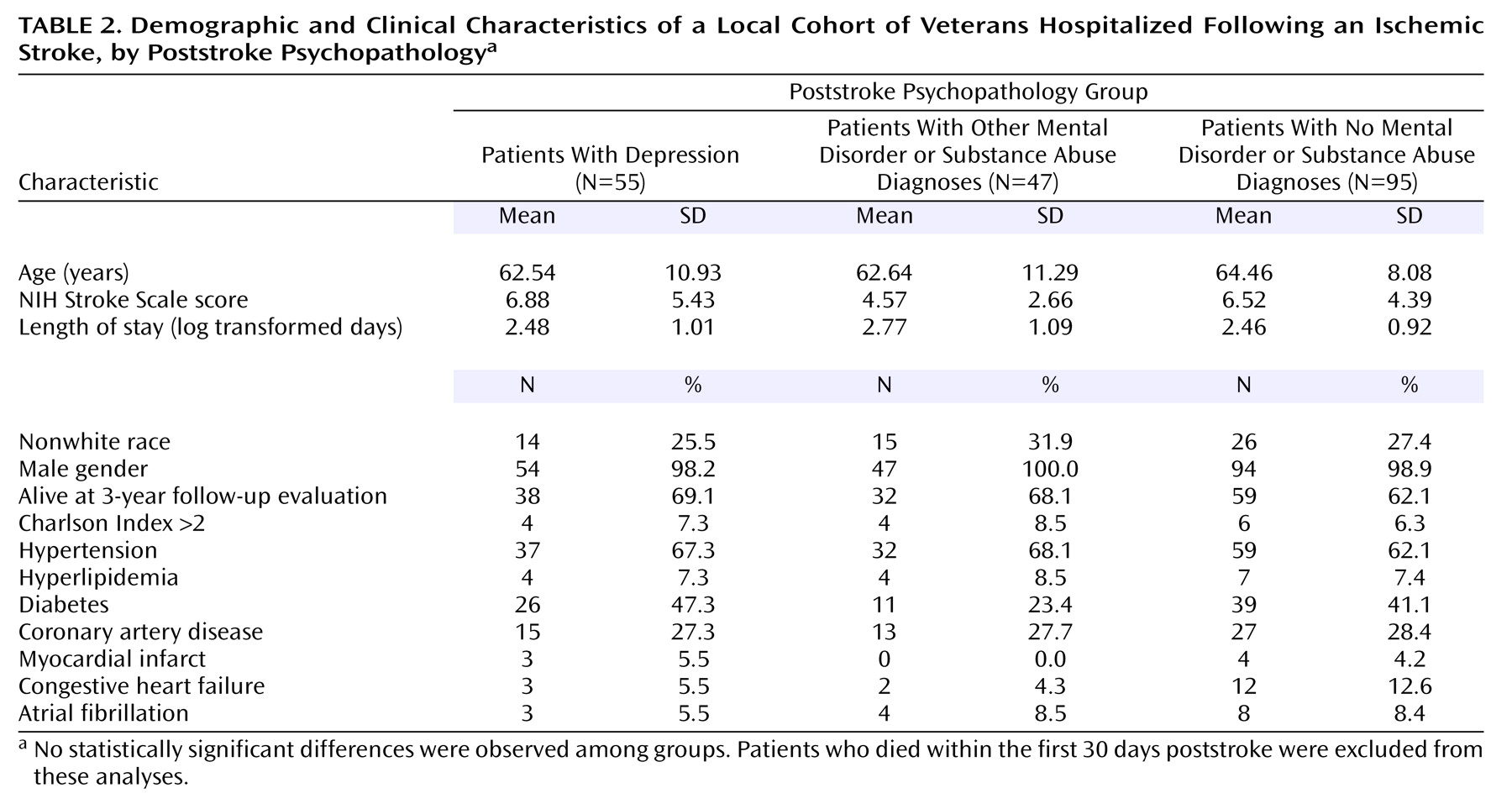
In the local dataset, we identified 55 patients with poststroke depression and matched these with 47 patients with other mental disorder or substance abuse diagnoses subjects and 95 patients with no poststroke psychopathology (
Table 2). Admission NIH Stroke Scale severity was not significantly different in patients with poststroke depression and those with no poststroke psychopathology (median admission ratings of 5 and 6, respectively). In a multivariate analysis of the local database, admission NIH Stroke Scale severity was not related to subsequent 3-year mortality (median NIH Stroke Scale admission ratings of 5 and 4 for those alive after 3 years versus those who died within 3 years, respectively).
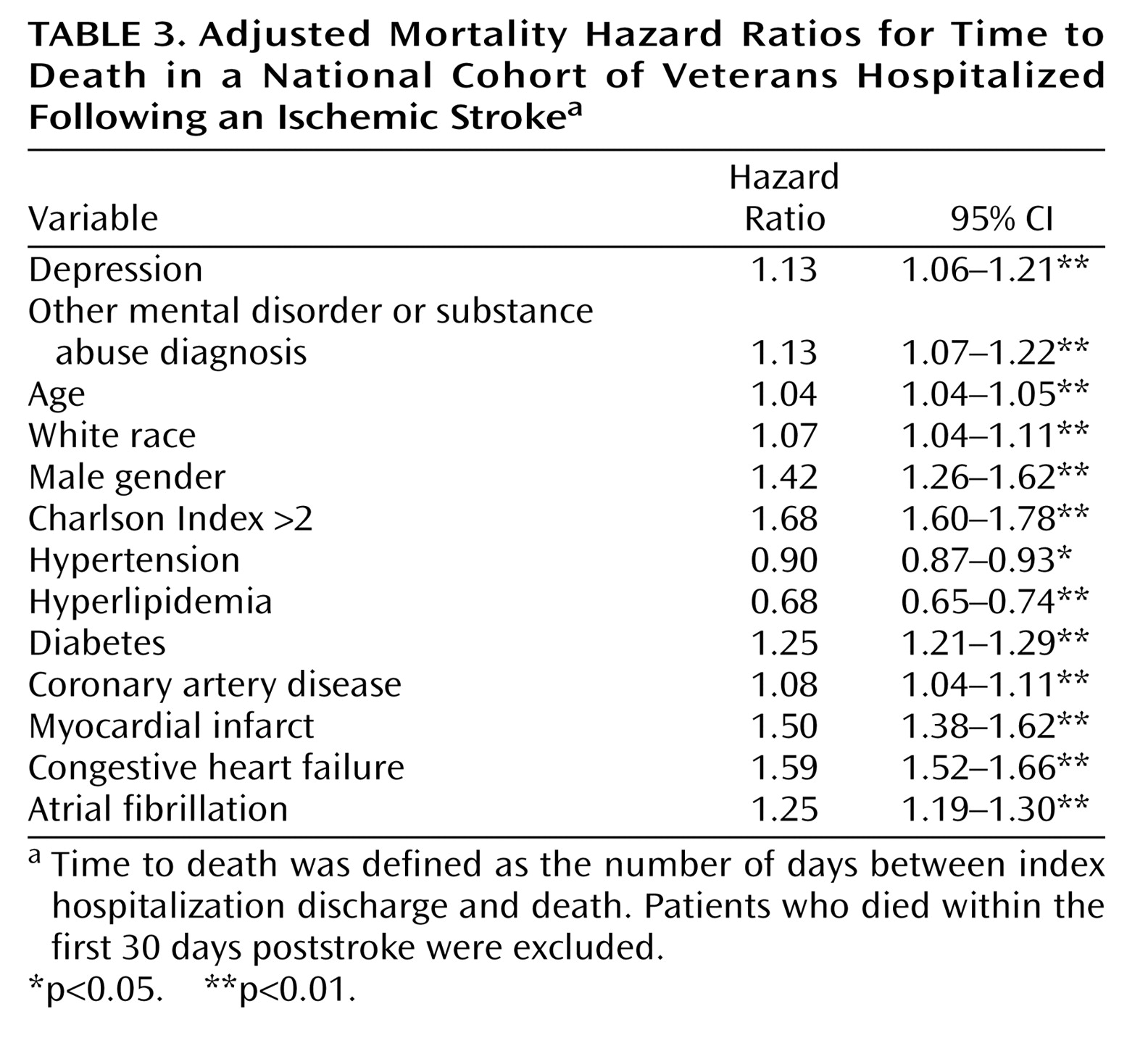
Hazard ratios for time to death are shown in
Table 3. Even when we controlled for specific cardiovascular risk factors with ICD-9 diagnoses and overall mortality risk with the Charlson Index, poststroke depression independently increased the risk of death by 13%. It is important to note that the presence of other mental disorder or substance abuse diagnoses also independently conferred mortality risk of similar magnitude.
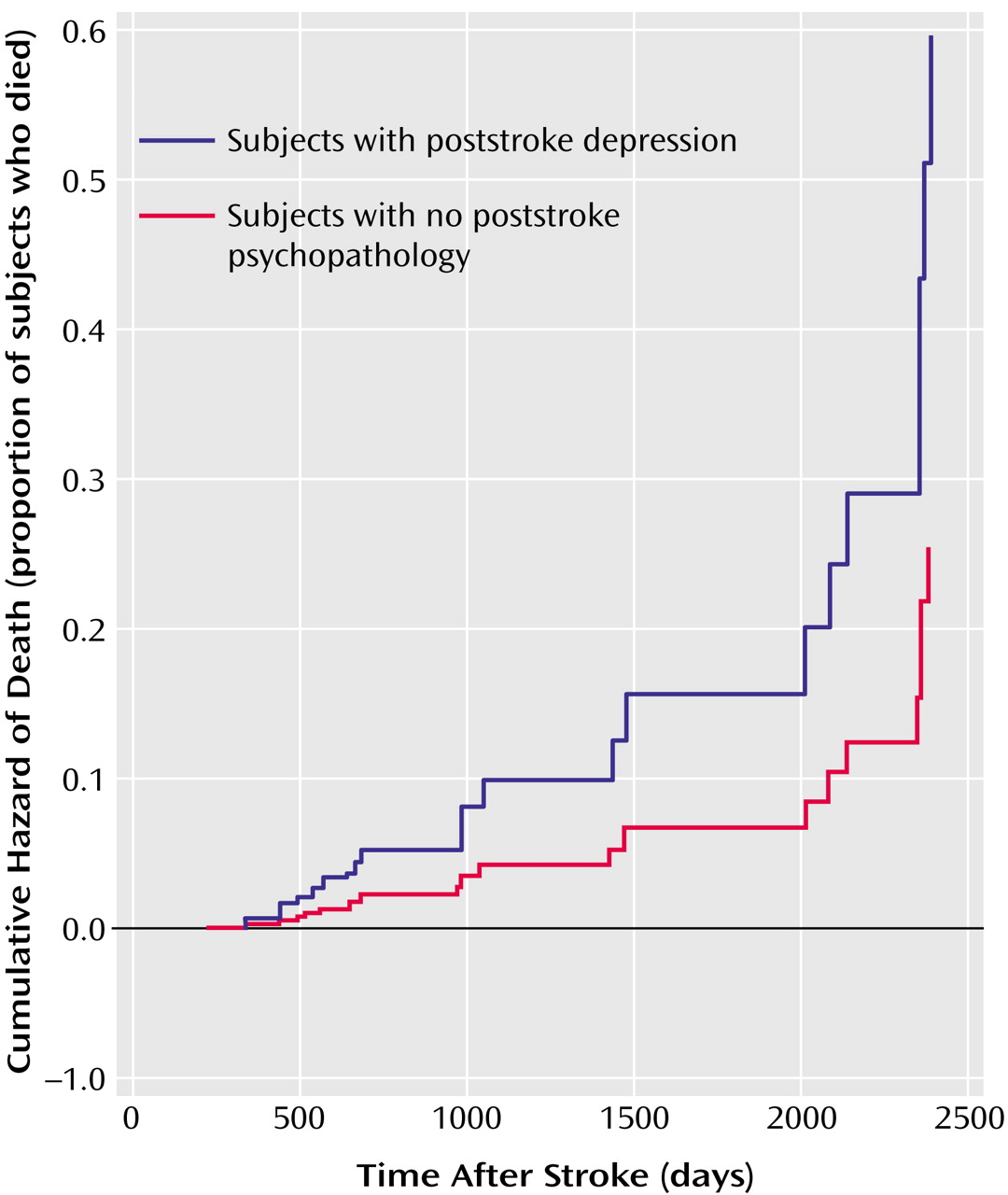
Figure 1 shows the survival curve for patients with poststroke depression and patients with no poststroke psychopathology.
Discussion
This study confirms prior reports of increased long-term mortality in patients with poststroke depression and extends this finding to show that other mental health conditions are also independently associated with an increased risk of death after an ischemic stroke. We found that even after we controlled for common cardiovascular conditions and other diagnoses, mental health diagnoses in the first 3 years after stroke increase the risk of death by more than 10%. In spite of the fact that patients with poststroke depression were younger and had fewer chronic illnesses than nondepressed patients, we found that the mortality risk was still higher in those with poststroke depression and other mental health diagnoses. These data speak to the seriousness of poststroke mental health diagnoses, since the presence of a mental health condition confers as much risk for subsequent mortality as many other cardiovascular risk factors.
Although the national database did not contain data about stroke severity, we constructed a local database in order to be able to assess, albeit on a much smaller and more homogeneous sample, whether admission stroke severity was related to the development of poststroke depression and to mortality after hospital discharge. In our sample, the admission NIH Stroke Scale score was similar between groups with and without poststroke depression, and admission NIH Stroke Scale score was not predictive of subsequent mortality. While it is clear that admission stroke severity is related to early stroke mortality
(13,
14), the purpose of this project was to examine the effect of poststroke depression, an outpatient diagnosis typically made weeks to months after a stroke, on long-term mortality. Patients dying within 1 month after a stroke were excluded from these analyses. Thus, the absence of a stroke severity indicator in the national administrative data set is unlikely to influence our long-term mortality models.
No studies have previously examined the impact of other mental health and substance abuse conditions on poststroke mortality. It may be that the mechanisms by which depression increases poststroke mortality risk are common to many mental disorders rather than unique to depression. Many of the disorders in the other mental disorder or substance abuse diagnosis group would be expected to predate the stroke rather than be a consequence of stroke. Potential biologic and social mechanisms by which this increased mortality risk may be incurred include psychoneurological impairments in immune functioning
(15,
16), functional and cognitive disability
(17,
18), unemployment
(19–
21), lack of exercise
(22,
23), poor nutrition
(24), life stress
(25), and low levels of social support
(26–
29) and coping resources
(30–
32).
Other studies have also reported the association between depression or depressive symptoms and mortality after stroke
(4–
8). Morris and colleagues
(4) reported a threefold increase in mortality during a 10-year follow-up study of a selected group of approximately 200 subjects, but this study had limited power to examine the influence of other chronic conditions on mortality. More recently, other research
(5,
8) has pointed to a link between depressive symptoms and negative attitudes and mortality after stroke. Like these more recent studies, our data suggest that the association between depression and mortality after stroke is somewhat smaller than that first reported by Morris and colleagues. Studies using a continuous measure of depression symptoms, like that by House and colleagues
(5), suggest that severity of depression symptoms, and perhaps specific symptoms of psychological distress and negative thoughts, may be associated with increased mortality risk. Since we had only a dichotomous diagnosis of depression, we were not able to assess the association between depression severity or specific depression symptoms and poststroke mortality.
The relationship between depression and increased risk of mortality has also been seen in other conditions, especially after cardiovascular disease
(33–
36). The mechanisms by which depression may be increasing mortality risk in these conditions is not known, although both physiologic
(16,
17,
37) and biopsychosocial
(19–
33,
38–40) associations have been suggested. Future work should focus on both the physiologic and psychosocial mechanisms by which mental health conditions may confer excess mortality risk so that effective interventions can be developed and tested to reduce poststroke mortality.
This study has several limitations. We used administrative data and thus had limited clinical severity indicators and had to use ICD-9 diagnoses to identify clinical conditions. This likely resulted in an underdiagnosis of depression and other mental disorder or substance abuse diagnoses. It is possible that more severely affected patients are more likely to receive an ICD-9 diagnosis of depression, thus these results may pertain only to patients with more severe depression. Likewise, we are unable to examine possible behavioral and biologic links between depression and increased stroke mortality like sedentary lifestyle and increased inflammation and platelet adhesion. We recognized that stroke severity might be an important mediating variable and so evaluated it in a local subset of the national dataset. Although stroke severity was not a predictor of mortality in this analysis, it is possible that the smaller number of deaths in this dataset limited our power to examine the effect of initial stroke severity on long-term mortality. It is possible that sicker patients have greater utilization of health care and thus have more opportunity for a depression diagnosis (ascertainment bias), but in our study poststroke depression and other mental disorder or substance abuse diagnoses were not independently predictive of inpatient utilization poststroke (data not shown). The possibility of residual confounding between unmeasured physical, mental, and social factors is always present in analyses of large administrative databases. However, our findings do correspond to other literature on depression and mortality after stroke, including prospective studies with more sensitive measures of depression. Finally, although our cohort contained more than 1,000 women stroke survivors, the Veterans Health Administration is a unique sample of mostly chronically ill, socioeconomically disadvantaged men. Further studies are needed to examine whether these relationships are also observed in other more heterogeneous populations.
Despite these limitations, these data show that both poststroke depression and other mental health diagnoses are associated with increased mortality risk after stroke. While the precise mechanisms underlying these associations are not known, these findings have important implications for stroke research and for clinical care. Researchers evaluating mortality after stroke should consider including depression and other mental health diagnoses in multivariate models of long-term stroke mortality. Clinicians treating stroke patients should be alert to the diagnosis and treatment of both depression and other mental health diagnoses. Whether treating poststroke depression and other mental health conditions not only improves patient symptoms but also reduces subsequent mortality risk remains an important, unanswered question.