Psychotic depression has been distinguished from nonpsychotic depression by its association with poorer premorbid function, longer depressive episodes, less responsiveness to antidepressant medication, and worse prognosis
(1,
2). Empirical evidence also suggests that, compared with nonpsychotic depression, psychotic depression is associated with a higher rate of neurobiological alterations, such as structural brain abnormalities
(3–
5) and excessive hypothalamic-pituitary-adrenal axis activity
(6,
7). Yet the neuropsychological profile of psychotic depression, especially in early and mid-adulthood, has received little systematic investigation. Existing data are inconsistent, often methodologically limited, and potentially confounded by the effects of chronic disease and exposure to antipsychotic treatments.
One avenue to better understanding of the neurocognitive dysfunction associated with psychotic depression involves comparison with clinically related conditions, particularly schizophrenia, with which psychotic depression shares psychotic features, and nonpsychotic depression, with which it shares affective symptoms. Prior studies of patients with nonpsychotic depression have reported executive and attention difficulties
(8–
11) that are relatively benign, compared to the diffuse and severe neuropsychological dysfunction that is often characteristic of schizophrenia
(12–
14). Whether the neuropsychological profile of psychotic depression is more similar to one or the other of these disorders is not known and would have implications for differential diagnosis, treatment, and prognosis. A similar pattern of neurocognitive deficits in psychotic and nonpsychotic unipolar depression would indicate a relatively benign pattern of cognitive and brain dysfunction, even when psychotic features accompany unipolar mood disorders. On the other hand, a neuropsychological profile of psychotic depression that is more consistent with that of schizophrenia would suggest common features of pathophysiology across these psychotic disorders. A neuropsychological profile markedly different from both disorders would provide further support for considering psychotic depression as a separate diagnostic classification and potentially suggest directions for future investigations of the disorder.
Psychotic depression has been associated with more severe dysfunction affecting a wider range of cognitive abilities than the mild and selective impairments observed in nonpsychotic depression
(8–
11). For example, in a previous study, patients with psychotic depression (N=12) showed impairments in memory and visual-spatial abilities that were associated with structural abnormalities found through magnetic resonance imaging
(3). In another study, patients with psychotic depression (N=46) performed worse than matched patients with nonpsychotic unipolar depression (N=34) on measures of verbal and nonverbal ability, attention, and manual dexterity
(15). However, the majority of participants in both groups were receiving medication at the time of testing, and the effect of past and current treatments on cognitive function in this population is not well understood. To address potential medication effects, Schatzberg et al.
(16) tested subjects after a 2-week washout period (6 weeks for antipsychotic medications) and found greater deficits in attention, response inhibition, and verbal memory for patients with psychotic depression (N=11), compared to healthy individuals (N=23) and patients with nonpsychotic unipolar depression (N=32).
Less consistent findings have resulted from investigations comparing the neuropsychological profiles of patients with psychotic depression to those of patients with schizophrenia and bipolar disorder. On measures of attention, memory, and problem solving, no differences were found between patients with schizophrenia and a heterogeneous group of patients with psychotic and nonpsychotic affective disorders
(17). These findings led the authors to conclude that similar cognitive impairments in schizophrenia and affective disorders represent “a final common pathway.” However, it is unclear what proportion of the affective disorder group had a history of psychosis and what effect this history may have had on test performance. Goldberg and colleagues
(18) found that schizophrenia patients scored significantly more poorly in several cognitive areas, compared with a combined group of patients with unipolar and bipolar affective illness. Similarly, chronic schizophrenia patients performed significantly more poorly on neuropsychological tests than patients with unipolar or bipolar psychotic affective disorder
(19). However, the degree to which these findings can be attributed to the course of illness or to previous treatment with psychoactive medication is unclear because most of the patients were chronically ill and were receiving medication at the time of testing. In a study that specifically assessed nonverbal problem solving, Rossi et al.
(20) found that patients with chronic psychotic bipolar illness scored between patients with chronic schizophrenia and healthy comparison subjects. Other studies have found that patients with psychotic affective disorder are more comparable to patients with schizophrenia. For example, an investigation of neuropsychological function in patients with first-episode schizophrenia and patients with first-episode affective disorders found that the schizophrenia patients performed worse than the affective disorder patients in some areas but that in other areas the level of impairment in the schizophrenia patients was similar to that in the patients with psychotic unipolar and bipolar depression
(21). In a study of older patients, both patients with schizophrenia and those with psychotic unipolar depression showed greater dysfunction in motor abilities, attention, and learning, compared to patients with nonpsychotic unipolar depression
(22). Again, the majority of participants in these studies were receiving medication at the time of testing, and there was no clinical follow-up of first-episode patients to confirm diagnosis.
The lack of consistent findings regarding psychotic depression and other psychiatric disorders may reflect confounding variables and methodological limitations. In many previous studies, group comparisons were potentially confounded by chronic illness, effects of medication and other treatments, illness severity, and age-related effects. Methodological limitations have included small numbers of subjects, lack of healthy comparison groups, and a focus on limited neuropsychological domains. The present study was designed to characterize the profile of neurocognitive dysfunction in psychotic depression by 1) comparing groups of patients with psychiatric disorders that share the clinical features of either psychosis or depression, 2) assessing patients before any lifetime exposure to antipsychotic treatment, 3) including longitudinal clinical follow-up to confirm subjects’ diagnoses, 4) evaluating a broad range of cognitive abilities, 5) including a comparison group of healthy patients, and 6) minimizing potential confounds by matching all groups demographically.
Method
Subjects
After hospitalization for a first lifetime episode of psychosis, with no prior antipsychotic treatment, 106 consecutively admitted patients who met the research diagnostic criteria for a psychotic disorder on the basis of the Structured Clinical Interview for DSM-III-R or DSM-IV (SCID) were recruited at the University of Pittsburgh Medical Center. Diagnosis was based on clinical data and was derived by trained raters and experienced clinicians during multidisciplinary consensus conferences. Scheduled follow-up evaluations at 12 and 24 months confirmed that 20 individuals met the criteria for unipolar depression with psychotic features. A diagnosis of a schizophrenia spectrum disorder (schizophrenia [N=71] or schizoaffective disorder [N=15]) was confirmed for the remaining 86 patients with a first episode of psychosis who were included in the study. Fourteen patients with nonpsychotic unipolar depression confirmed by a SCID interview were recruited, as were 81 healthy individuals from the community who had no history of psychiatric treatment and no axis I disorder, as confirmed by a SCID interview. The patients with psychotic depression and schizophrenia had no prior lifetime treatment with antipsychotic medication. The patients with nonpsychotic unipolar depression were antipsychotic naive and free of antidepressant medication for at least 3 weeks before enrollment. Several patients with psychotic symptoms (N=21) were previously treated with antidepressant medications and were free of those agents for more than 6 weeks on average. Treatment with antipsychotic or other medications was initiated after administration of the neuropsychological battery. All participants had no known history of neurologic disorders or of substance dependence or abuse within 6 months, no psychiatric disorders other than those previously specified, and no history of head injury with loss of consciousness, other medical disorders that may affect brain function, or recent/current ECT or treatment with anticonvulsants or benzodiazepines. Verbal and written consent were provided by all participants, and the study was approved by the University of Pittsburgh Institutional Review Board.
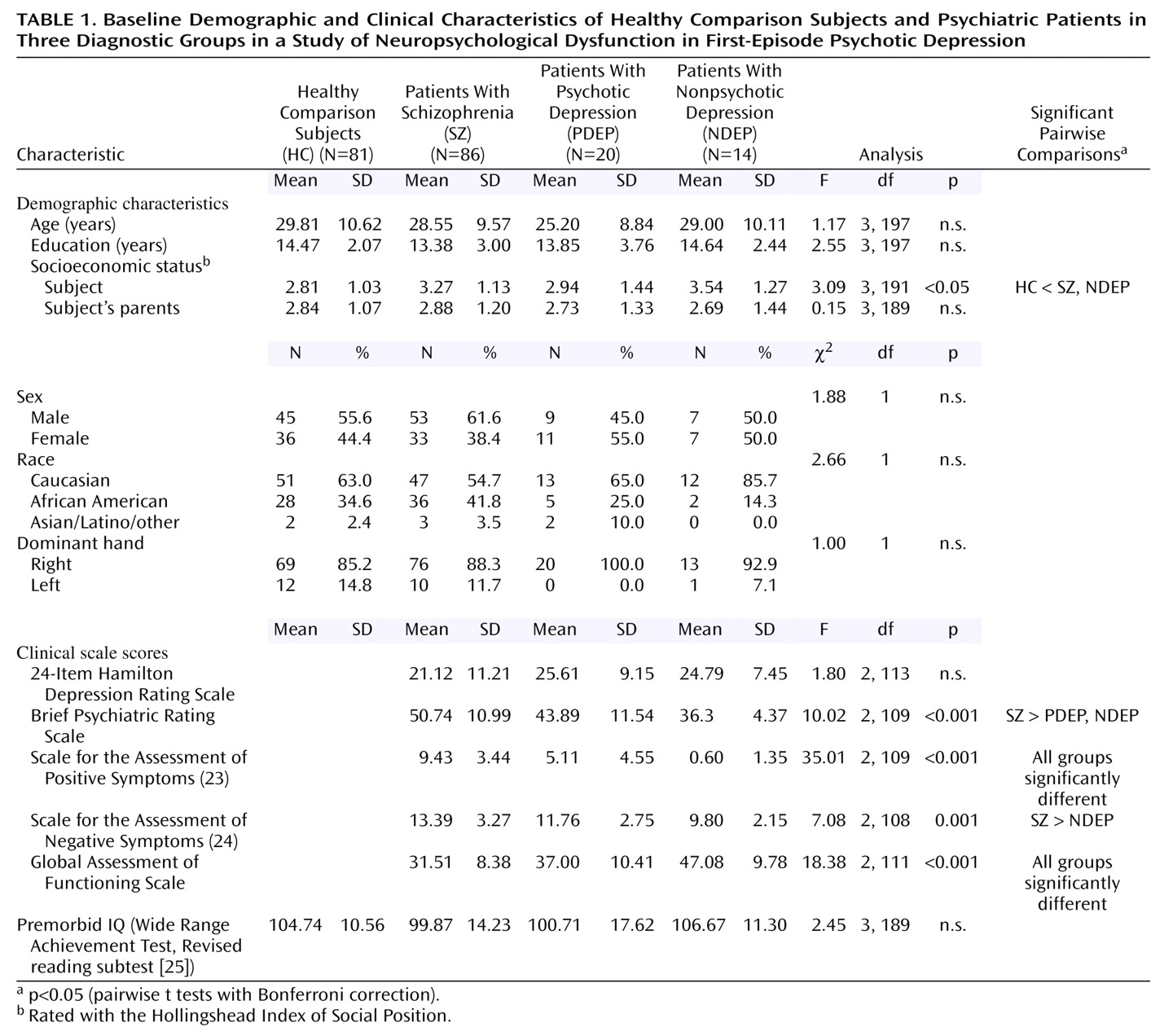
All groups were matched demographically on age, sex, and parental socioeconomic status, as measured with the Hollingshead Index of Social Position. Demographic and clinical data are summarized in
Table 1. Analysis of demographic information revealed that the healthy comparison subjects had higher personal socioeconomic status, compared to the nonpsychotic unipolar depression and schizophrenia groups. However, there were no statistically significant group differences for mean estimated premorbid intelligence level, as measured by the Wide Range Achievement Test, Revised reading subtest
(25).
Clinical and Neuropsychological Evaluation
Participants in the three psychiatric groups underwent diagnostic examination with the SCID. The severity of their psychiatric symptoms was rated with the the 24-item Hamilton Depression Rating Scale, the Brief Psychiatric Rating Scale (BPRS), the Scale for the Assessment of Positive Symptoms (SAPS)
(23), and the Scale for the Assessment of Negative Symptoms (SANS)
(24). The Global Assessment of Functioning Scale (GAF) score (DSM-III-R, p. 12; DSM-IV, p. 32) was obtained as part of the SCID. Of the 20 participants with psychotic depression, 80% (N=16) displayed mood incongruent psychotic features.
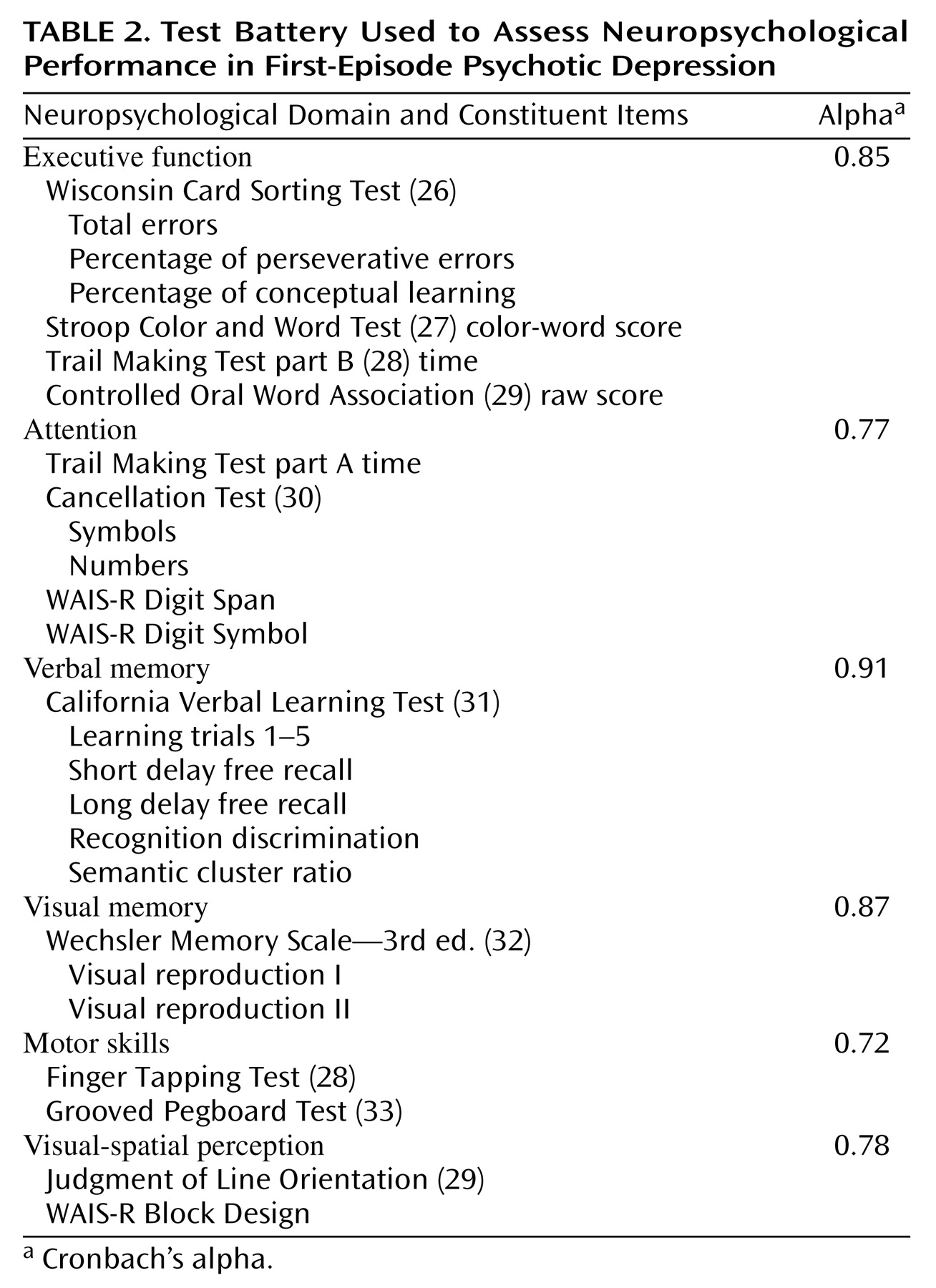
All participants completed a standard neuropsychological battery before beginning treatment with antipsychotic agents. At the time of testing, the examiners were unaware of the patients’ diagnoses, which typically had not yet been determined. The battery included tests of general intelligence, executive function, attention, verbal memory, visual memory, motor skills, and visual-spatial perception. The tests used to evaluate function in each of these neuropsychological domains, determined on an a priori basis, are listed in
Table 2.
Data Analysis
To provide a standard metric for comparison across neuropsychological tests and domains, test scores were standardized (by using z scores) to the performance of the healthy comparison group. To meet the assumptions for parametric analysis, each of the neuropsychological variables was assessed for normality of distribution by calculating two-tailed tests of skewness and kurtosis. The scores for both the Judgment of Line Orientation and California Verbal Learning Test recognition discrimination were negatively skewed in a manner that was not amenable to normalization by using routine transformations. For these two scores only, non-normalized reference means and standard deviations were computed by using the model of a one-tailed z distribution. Outliers resulted in nonnormal distributions for the percentage of perseverative errors on the Wisconsin Card Sorting Test, the Trail Making Test part B, the Wechsler Memory Scale—3rd ed. delayed visual reproduction test, the bilateral Finger Tapping Test, and the dominant-hand Grooved Pegboard Test. The distribution of these variables normalized when the outliers were omitted, and the z scores were computed by using the normalized distribution. Examination of individual variable scores revealed some extreme scores (five to eight standard deviations below the mean) that were truncated to z=–5.0 to avoid undue influence of outliers. After normalization and truncation, scores for each neuropsychological function were computed as the mean of the variables that compose each function
(14,
34). Specifically, summary measures were calculated for executive function, attention, verbal memory, visual memory, motor skills, and visual-spatial perception. A composite of global neuropsychological function was computed as the mean of all six summary scores.
To assess group differences in neuropsychological function, one-way analysis of variance (ANOVA) was conducted by using the global composite scores. In the presence of group differences in global neuropsychological function, simple pairwise group contrasts were conducted to clarify group differences. To assess potential profile differences among groups, two-way repeated-measures multivariate analysis of variance (MANOVA) was conducted with neuropsychological function (executive function, attention, verbal memory, visual memory, motor skills, and visual-spatial perception) as the within-subjects factor and diagnostic group (schizophrenia, psychotic depression, nonpsychotic depression, and healthy comparison) as the between-subjects variable. Because of unequal cell size, Pillai’s test was used to compare the groups. Significant interactions were clarified by using a series of univariate ANOVAs for each neuropsychological function. To maintain acceptably low type I error rates, we employed a conservative approach to a priori planned analyses by utilizing Bonferroni corrections for simple contrasts and post hoc group comparisons. The unequal group sizes may have differentially influenced power, particularly for comparisons involving the two groups of depressed patients, and the probability of type II error is unclear. Demographic covariates were not used during analysis of neuropsychological performance because the groups did not differ significantly in age, sex, education, parental socioeconomic status, or premorbid intelligence.
Results
Clinical Features
Compared to the two groups with unipolar depression, the schizophrenia group was rated as having more positive symptoms of psychosis and lower global (daily) functioning (
Table 1). Negative symptom ratings were greater for the schizophrenia patients than for the patients with nonpsychotic depression. There was no difference in the severity of negative symptoms between the schizophrenia group and the psychotic depression group.
Neuropsychological Comparisons
To assess the possibility that neuropsychological differences existed between the 15 patients with schizoaffective disorder and the remaining participants in the schizophrenia group, a two-way repeated measures MANOVA was conducted (group [schizoaffective disorder versus schizophrenia] by neuropsychological domain). The results showed no omnibus difference in neuropsychological performance between the subjects with schizoaffective disorder and those with schizophrenia (F=0.93, df=1, 83, p>0.05). Thus, data for the schizoaffective disorder patients and schizophrenia patients were pooled in the following analyses, consistent with the a priori data analytic plan.
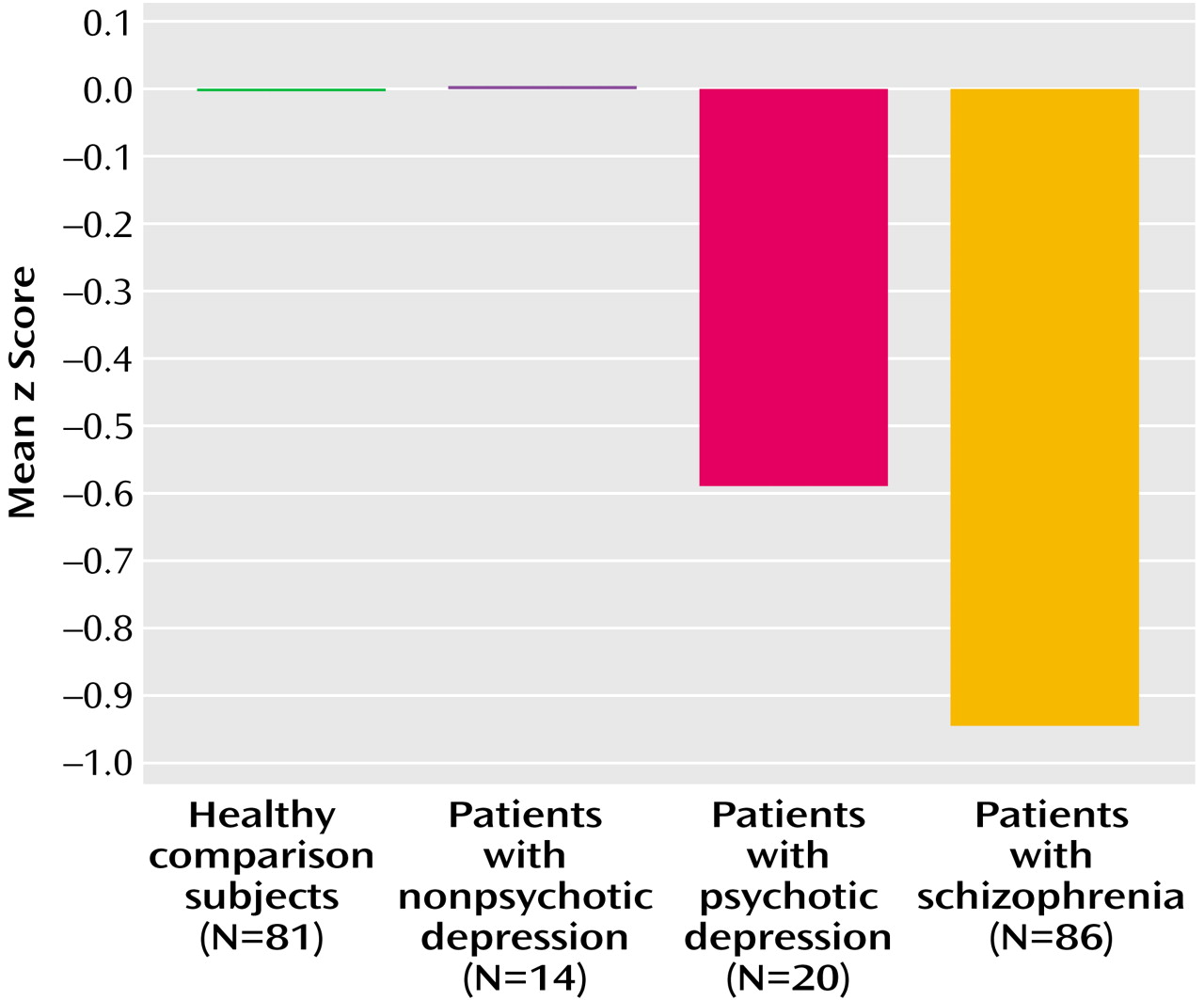
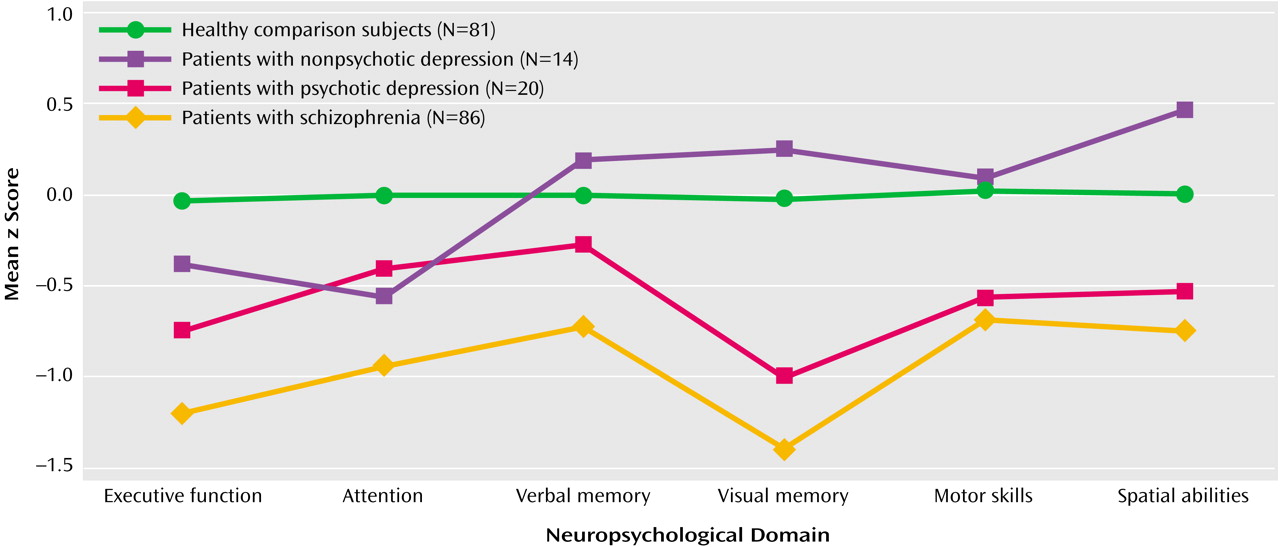
Global neuropsychological performance differed significantly among the diagnostic groups (F=25.76, df=3, 197, p<0.001) (
Figure 1). Simple contrasts among groups made with a Bonferroni correction revealed that global performance was significantly better for the healthy participants, compared to the schizophrenia and psychotic depression groups. Schizophrenia patients also performed significantly worse overall, compared to the patients with nonpsychotic depression. The results of a repeated-measures MANOVA to clarify differences in global neuropsychological function are illustrated in
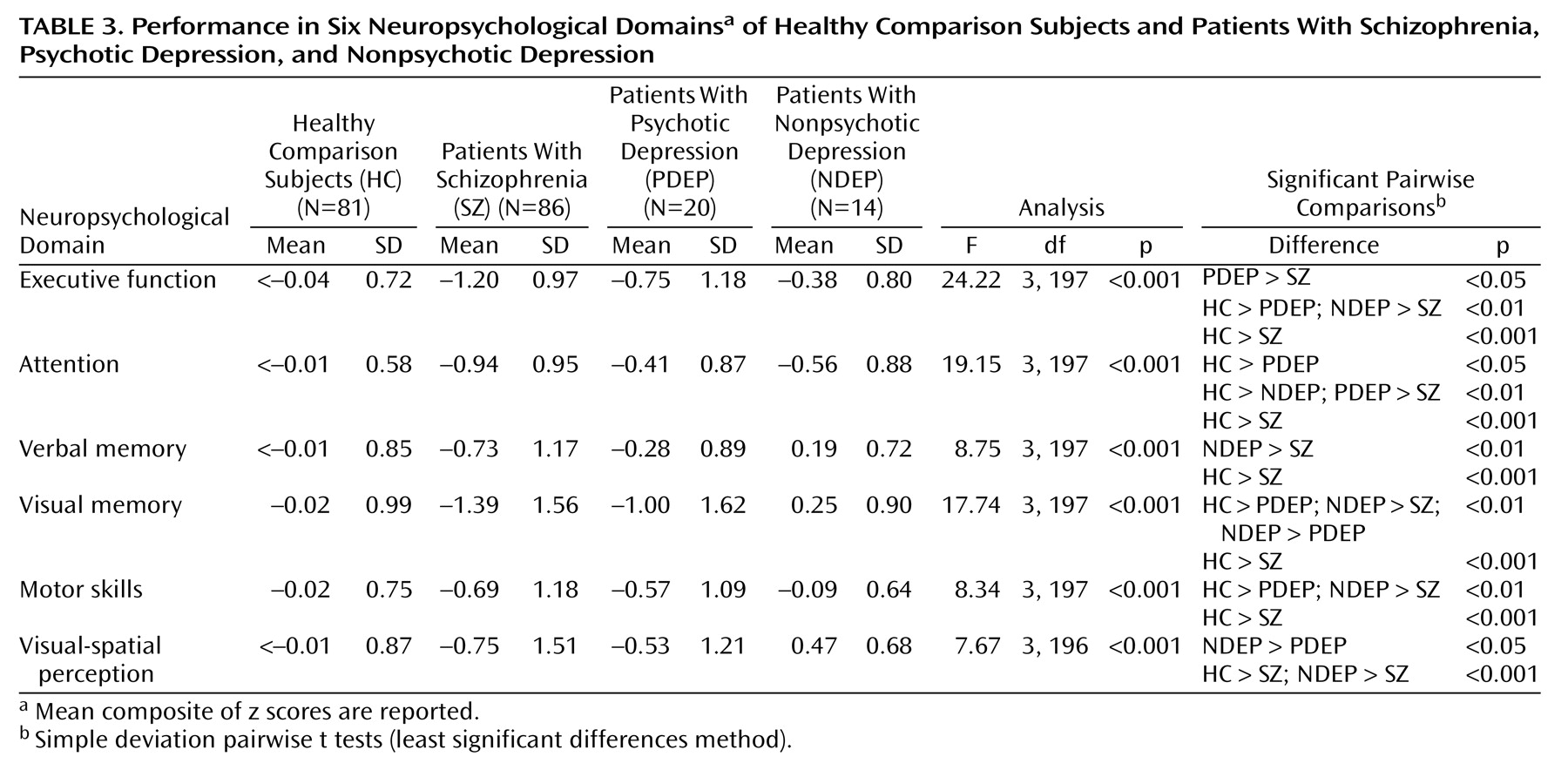
Figure 2. Significant main effects were found for both diagnosis (F=26.6, df=3, 196, p<0.001) and neuropsychological function (F=5.93, df=5, 192, p<0.001), as well as for the interaction of diagnosis and neuropsychological function (F=2.54, df=15, 582, p=0.001). Univariate ANOVAs were conducted separately for each neuropsychological function to clarify the two-way interaction (
Table 3). With the exception of having lower attention scores than the healthy comparison subjects, the patients with nonpsychotic depression performed similarly to the healthy comparison group in all areas. The schizophrenia patients performed more poorly than the healthy participants in all domains and more poorly than the patients with nonpsychotic depression in all domains but attention. Significantly impaired performance was noted for the patients with psychotic depression, relative to the healthy participants, in all areas but verbal memory and visual-spatial perception. The patients with psychotic depression performed more poorly than their nonpsychotic counterparts in visual memory and visual-spatial perception. The psychotic depression and schizophrenia groups differed only on measures of executive function and attention.
As
Table 1 shows, several group differences were noted in clinical symptoms. To assess the potential effect of clinical state on neuropsychological performance, correlations were computed among clinical variables and each of the six neuropsychological domains. Despite differences in the severity of positive symptoms among the patient groups, no relationship was found between SAPS scores and neuropsychological performance in any domain for any clinical group. Similarly, no relationship between GAF scores and neuropsychological performance was found for any patient group. A significant negative correlation was found between SANS scores and executive function for schizophrenia patients (r=–0.35, df=83, p=0.001). Among patients with psychotic depression, BPRS scores were significantly correlated with global neuropsychological performance (r=–0.52, df=17, p<0.05), visual memory (r=–0.57, df=17, p=0.01), motor skills (r=–0.46, df=17, p=0.05), and visual-spatial perception (r=–0.56, df=17, p<0.05).
To examine the extent to which profile differences among clinical groups could be attributed to the level of overall psychiatric (BPRS) or negative symptoms (SANS), univariate ANOVAs were rerun with covariation of BPRS and SANS scores to analyze the significant clinical group contrasts reported in
Table 3. For executive function, the schizophrenia patients no longer differed from the patients with nonpsychotic depression (F=1.35, df=1, 90, p>0.05) or the patients with psychotic depression (F=3.35, df=1, 97, p>0.05) when symptom severity was covaried. In contrast, differences in attention between the schizophrenia group and the psychotic depression group were robust even after the covariation of clinical symptoms (F=5.95, df=1, 97, p<0.05). For verbal memory, the difference between the schizophrenia group and the nonpsychotic unipolar depression group dissipated when the comparison controlled for variance in BPRS and SANS scores (F=2.46, df=1, 90, p>0.05). The patients with nonpsychotic depression displayed a robust advantage over the schizophrenia patients in visual memory when clinical symptoms were covaried (F=6.76, df=1, 90, p=0.01), but their advantage over the patients with psychotic depression was lost (F=0.67, df=1, 23, p=0.42). Differences among clinical groups for visual-spatial perception were robust after covariation of clinical symptoms: the patients with nonpsychotic unipolar depression outperformed both the schizophrenia patients (F=4.27, df=1, 89, p<0.05) and the patients with psychotic depression (F=4.08, df=1, 23, p<0.05). Finally, when the severity of clinical symptoms was covaried, the patients with nonpsychotic unipolar depression and the patients with schizophrenia no longer differed on motor skills (F=2.89, df=1, 23, p>0.05).
Discussion
To our knowledge, this is the first study to provide data that document the neuropsychological profile of psychotic depression in young adults at the time of the first episode of illness, before treatment with antipsychotic medication. Furthermore, the neuropsychological status of these patients was compared with that of patients with other psychiatric disorders that share clinical features with psychotic depression—first-episode schizophrenia, which shares the feature of psychosis, and nonpsychotic unipolar depression, which shares the feature of depressive illness. Visual inspection of the neuropsychological profiles for those groups, represented in
Figure 2, indicates remarkably similar patterns of cognitive dysfunction in schizophrenia and psychotic depression. Absolute levels of dysfunction for all cognitive areas were less severe for patients with psychotic depression than for those with schizophrenia, and statistically significant differences in attention between those groups were robust after covariation of symptom severity. In contrast, the cognitive profile for nonpsychotic unipolar depression differed dramatically from that for psychotic depression and was more consistent with the cognitive profile for the healthy comparison group. The level of performance was generally lower in psychotic versus nonpsychotic unipolar depression, and statistically significant differences between those groups were present for visual-spatial perception. These data not only provide additional support for psychotic depression as a distinct mood disorder but also document the considerable neuropsychological morbidity associated with the disorder. Further, the similarity in the profiles of neuropsychological dysfunction in schizophrenia and psychotic depression suggests that similar, cognitively relevant brain systems are affected in both psychotic disorders. Ultimately, while these two psychotic disorders are likely to result from fundamentally different mechanisms at the level of molecular processes and synaptic physiology, their similarity at the systems level suggests that the disorders share a final common pathway
(17) in terms of their effect on neurocognitive abilities.
In this study, the potential effects of chronic psychotic symptoms and the potential acute or chronic effects of antipsychotic medications were reduced by inclusion of participants with psychotic symptoms during their first episode of psychosis and before antipsychotic treatment. All groups were also matched for age, sex, education, premorbid intellectual abilities, and parental socioeconomic status. Consequently, the observed similarities and differences in cognitive profiles are not attributable to demographic features, medication status, premorbid abilities, or duration of illness. However, differences in clinical symptoms were observed among the clinical groups (
Table 1). Although the correlation analysis revealed relative independence of cognitive performance and clinical state, covariation of BPRS and SANS scores attenuated some group differences, particularly the differences in executive function, verbal memory, visual memory, and motor skills. These findings offer further evidence that psychotic depression is neuropsychologically more similar to schizophrenia than to nonpsychotic unipolar depression
(19–
21,
22,
35). The similarity of neuropsychological profiles observed in psychotic depression and schizophrenia, when considered in conjunction with the results of investigations assessing psychotic and nonpsychotic bipolar disorder patients
(17–
19,
21), suggests that psychosis may be related to a similar global neuropsychological dysfunction regardless of the presence or absence of affective symptoms, albeit perhaps a less severe dysfunction in affective psychotic disorders. Studies that more directly assess neurophysiology and both functional and structural brain abnormalities among these groups are warranted to clarify the underlying similarities and distinctions.
The patients with schizophrenia displayed a profile of executive, attention, and memory deficits consistent with previously documented frontal-temporal dysfunction
(12–
14). These cognitive impairments are enduring features of schizophrenia
(36–
39) that disrupt occupational function and cause long-term disability
(40,
41). The current data suggest a somewhat less severe clinical manifestation and level of neuropsychological dysfunction in psychotic depression. However, several questions remain. Is the course of neuropsychological dysfunction in psychotic depression similar to that observed in schizophrenia? If the neuropsychological dysfunction associated with psychotic depression is enduring, then can cognitive behavior therapy, psychopharmacologic treatments, or other interventions reduce neuropsychological or functional deficits?
The mild difficulties in executive function and attention observed in the nonpsychotic unipolar depression group were consistent with previous characterizations of depression that have implicated attention and executive systems
(8–
11,
42). Despite the small number of participants with mood disorders in this study and the need for replication of the current data, the findings augment the growing support for the presence of mild disruption of frontal-striatal circuitry in nonpsychotic depression
(43,
44).
In summary, the study found that the neuropsychological dysfunction associated with psychotic depression is similar in quality and level of dysfunction to that associated with schizophrenia (when the effects of symptom severity were controlled statistically). On the other hand, the neuropsychological profile for psychotic depression was markedly different in shape and severity, compared to that for nonpsychotic depression. The deficits associated with psychotic depression were not attributable to previous exposure to antipsychotic medication, chronic disease effects, potential diagnostic errors at index examination, or demographic characteristics. Thus, psychosis appears to be associated with a common profile of diffuse neurocognitive dysfunction, regardless of whether it occurs in the context of schizophrenia or depression. Additional studies are needed to assess the long-term stability of neuropsychological impairment in both early- and late-onset psychotic depression, relative to the persistent deficits found in schizophrenia, and ultimately to identify etiological factors underlying the systems-level brain disturbance implicated by the neuropsychological data for patients with psychotic disorders.