The events of Sept. 11, 2001, highlighted the importance of understanding the effects of trauma and disaster on rescue and disaster workers. These first responders are exposed to life-threatening situations, work with survivors and families, and often recover the dead and injured. Firefighters and volunteer mortuary workers have high levels of posttraumatic stress disorder (PTSD) symptoms
(1,
2) and rates of PTSD that range from 11% to 32%
(3,
4). Physical health morbidity and increased health care utilization have also been noted after exposure to traumatic events and disasters
(5–
7). Higher rates of somatization and physical complaints have been reported in disaster workers working with the dead
(4,
8,
9). Generally, disaster workers with the highest levels of early symptoms are at the greatest risk 1 and 2 years later
(10,
11), although recovery is also reported
(4).
To our knowledge, no prospective studies of exposed disaster workers with a comparison group have examined acute stress disorder, PTSD, and depression. In order to better plan for the health care of disaster workers, we examined acute stress disorder, PTSD, depression, and health care utilization in 207 disaster or rescue workers over the 13 months after the crash of a United Airlines DC-10. In addition, we examined early dissociative symptoms, disaster exposure, and previous disaster experience as risk factors.
Method
The Disaster
A United Airlines DC-10 carrying 355 passengers and crew was forced to crash-land after a midair explosion that caused failure of the plane’s hydraulic system. Upon landing, the plane broke apart and burst into flames. Some victims, still in their seats, were thrown from the aircraft. Others died in the burning fuselage. Of those aboard, 112 people died, 59 were seriously injured, and 184 survived.
Subjects
One month after the disaster, we contacted 440 exposed disaster workers assigned to the airport disaster and the rescue response team. We also contacted 700 disaster and rescue workers at a similar-sized community and airport approximately 90 miles away who were matched for socioeconomic level, geography, and urban/rural location as a potential comparison group. After describing the study, 207 exposed disaster workers (mean age=36.8, SD=9.7) and 421 of the comparison group (mean age=36.2, SD=9.9) agreed to participate, signed informed consent, and completed assessments. Participants in the study were similar to those who did not participate in age and gender. The median date for completion of the time 1 assessment was 2 months postdisaster (90% completed within 16 days of the median), time 2 was 7 months postdisaster (90% completed within 56 days) (exposed disaster workers, N=161; comparison group, N=283), and time 3 was 13 months postdisaster (90% completed within 22 days) (exposed disaster workers, N=116; comparison group, N=217). Within the exposed group and the comparison group, the completers did not differ from the noncompleters on any demographic variables.
Assessments
Acute stress disorder and PTSD were assessed for exposure to this disaster. Acute stress disorder was assessed for the week after the disaster at the first assessment by using a previously validated measure that was modified according to the recommendation of Staab et al.
(12) to require at least three of the possible five dissociative symptoms of criterion B (e.g., “feeling numb,” “feeling as if it hadn’t happened or wasn’t real”) to meet the DSM-IV criteria for acute stress disorder. In order to measure early dissociative symptoms, we created two variables: the presence of any early dissociative symptoms and the number of early dissociative symptoms. We identified PTSD at 13 months by using the DSM PTSD-IV Scale, a validated assessment of PTSD with good sensitivity and specificity when compared with SCID diagnoses in community samples
(13–
15). Clinically significant depression was assessed dichotomously by using the standardized cutoff (score >50) established for the Zung Self-Rating Depression Scale
(16) at 7 and 13 months postdisaster. We assessed PTSD only at 13 months, in part due to the space limitations on the 7-month survey and because we were most interested in PTSD as a possible long-term outcome of acute stress disorder. Depression related to trauma has been rarely studied as an early or later response. Three types of disaster exposure were assessed. A total of 45 subjects (22%) were exposed to physical danger, 98 subjects (47%) worked with or assisted survivors, and 131 subjects (63%) worked with the dead. Subjects were grouped into low exposure (none, one, or two types of exposure) versus high exposure (three types of exposure), with 12.1% (N=25) scoring in the high exposure category. Subjects reported health care for the intervening time at each assessment point by responding “yes” or “no” to the following four questions: 1) annual physicals, 2) physical problems, 3) emotional or family problems, and 4) they felt they needed but did not seek medical care.
Statistical Analyses
Comparisons between exposed disaster workers and comparison subjects were made with chi-square analyses and t tests, as appropriate. Potential risk factors for acute stress disorder, PTSD, and depression were evaluated by univariable logistic regressions, multivariable logistic regression, and chi-square analyses. We chose risk factors that were variables of clinical importance in workers that might be seen in order to identify risk factors for acute stress disorder, PTSD, and depression. We examined several multivariable models to address 1) clinical questions relating to previous disaster experience and its possible role as sensitizing to later acute stress disorder, PTSD, or depression and 2) the comorbidity of PTSD and depression. We adjusted for marital status because it was a predictor of depression at 13 months. The estimate of the odds ratio and its 95% confidence interval (CI) are reported. To ensure stability of findings, analyses were repeated by using listwise deletion to include only subjects present at 3, 7, and 13 months after the accident. Goodness-of-fit chi-square analyses assessed how well the model predicted the data
(17).
In order to control for experiment-wise error, when we examined health care utilization, we first examined the association of exposed disaster workers and comparison subjects across all times, looking only at those subjects present for all three assessments with chi-square analysis. If there was a significant finding, we proceeded to examine each assessment point. Significance level was set at p=0.05. Statistical Analysis Software
(18) was used for all analyses.
Results
Rates of Acute Stress Disorder, PTSD, and Depression
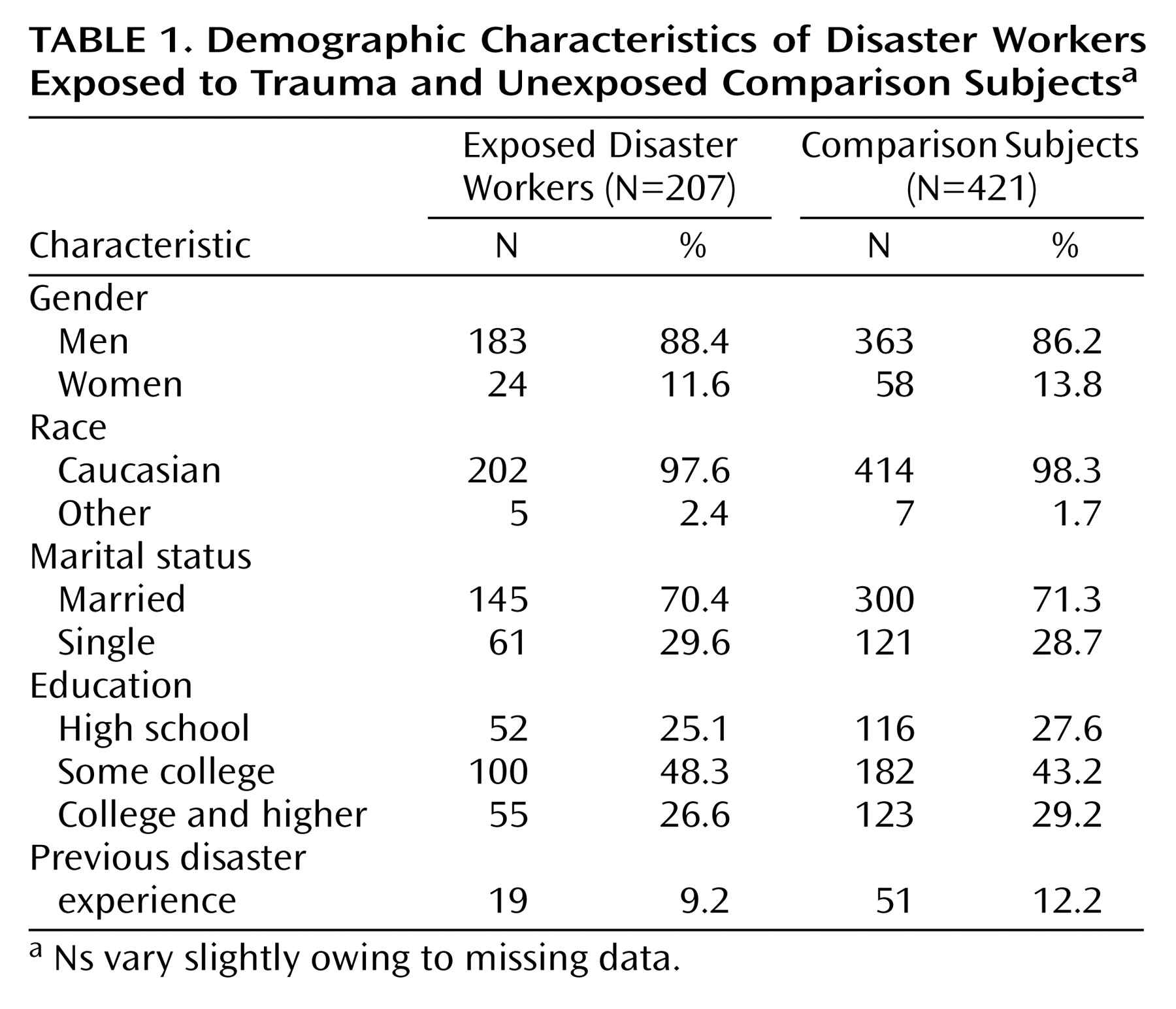
There were no differences between the exposed disaster workers and the comparison subjects on demographic characteristics at any assessment point (
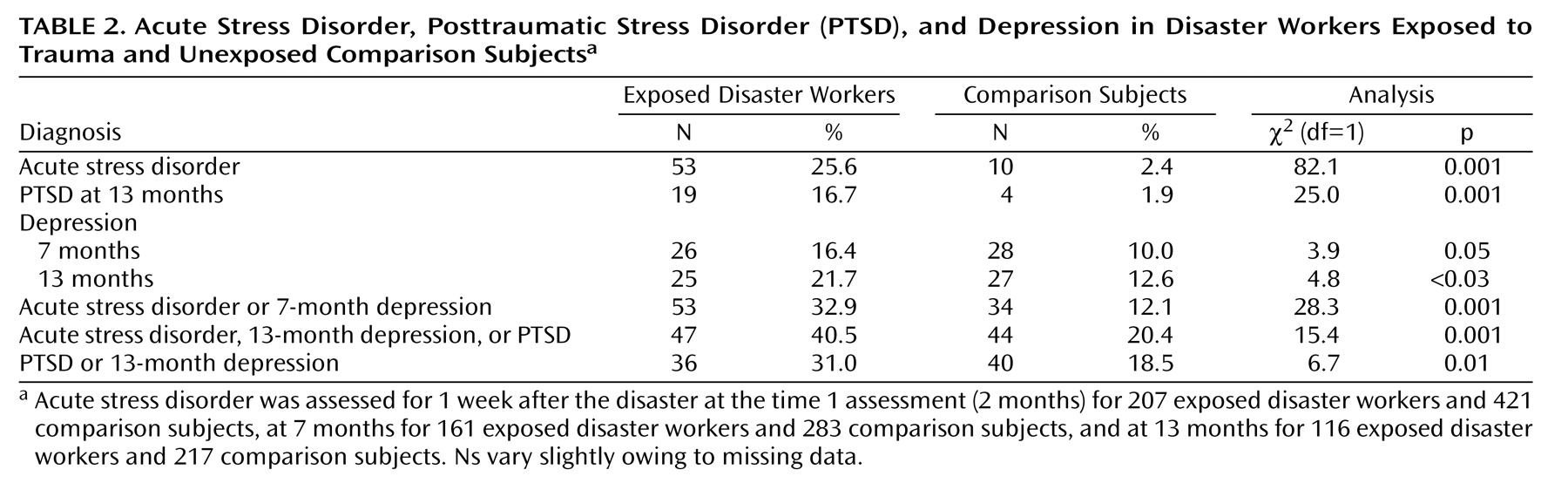
Table 1). There were no differences between the exposed disaster workers (N=19, 9.2%) and the comparison subjects (N=51, 12.2%) on previous disaster experience. The exposed disaster workers had significantly higher rates of acute stress disorder than the comparison subjects (25.6% versus 2.4%) (p=0.001) (
Table 2). The exposed disaster workers had significantly higher rates of PTSD at 13 months (16.7% versus 1.9%) (p=0.001) and depression at 7 months (16.4% versus 10.0%) (p=0.05) and at 13 months (21.7% versus 12.6%) (p<0.03).
Risk Factors for Acute Stress Disorder in Exposed Disaster Workers
We examined gender, age, education, marital status, previous disaster experience, and disaster exposure as risk factors for acute stress disorder. Exposed disaster workers who were younger were at greater risk of acute stress disorder (odds ratio=0.35, 95% CI=0.18–0.68, p=0.002). Of the married subjects, 30 (20.7%) had acute stress disorder, while 23 (37.1%) of the unmarried subjects had acute stress disorder (χ2=6.14, df=1, p=0.01). Unmarried subjects were 2.26 times more likely to develop acute stress disorder than those who were married (95% CI=1.18–4.34, p<0.02). Acute stress disorder was not related to any other demographic characteristic nor to previous disaster experience or disaster exposure.
Risk Factors for PTSD in Exposed Disaster Workers
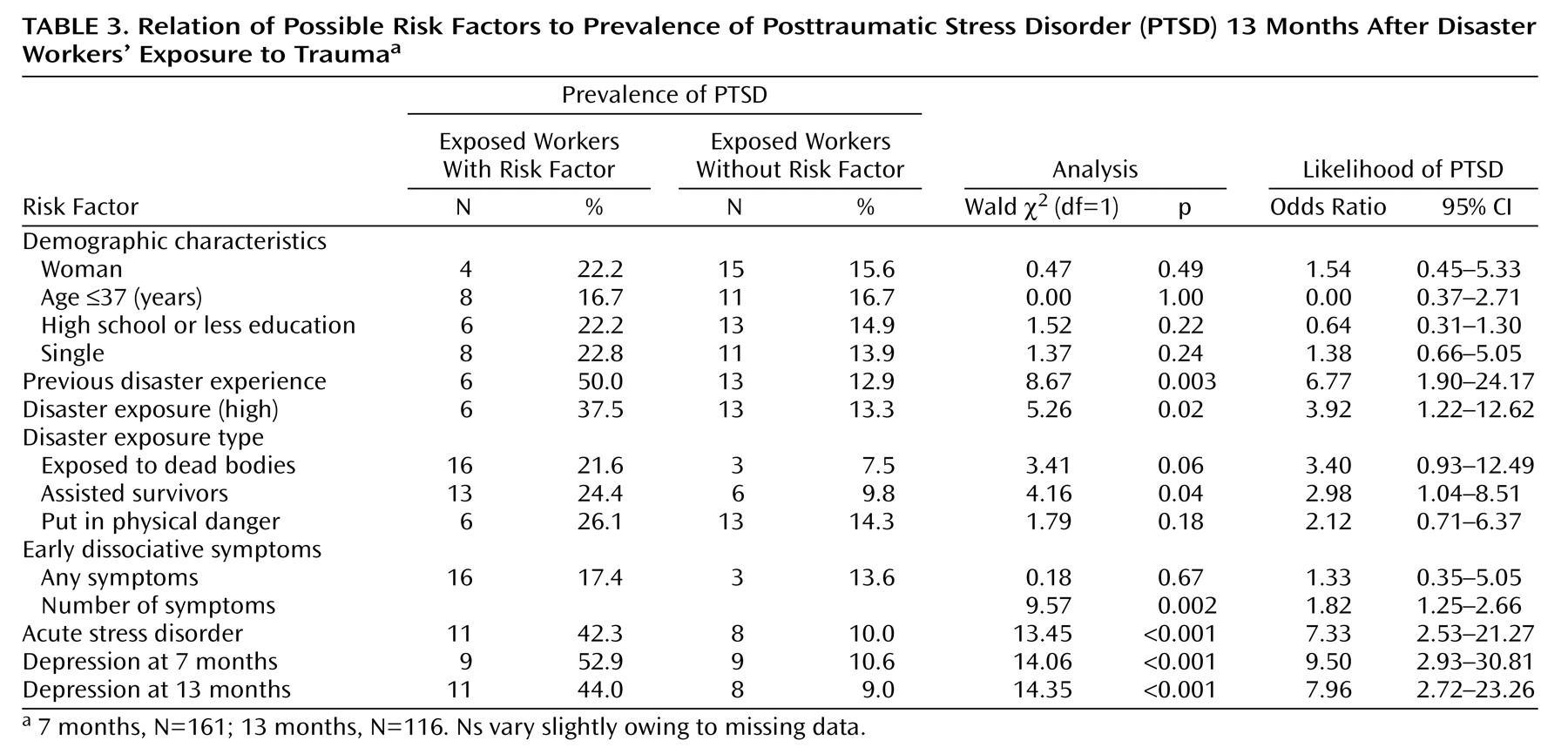
PTSD was not related to any demographic factors. Exposed disaster workers with previous disaster experience were 6.77 times more likely to develop PTSD at 13 months (95% CI=1.90–24.17, p=0.003) (
Table 3). Because exposure may increase the risk for PTSD and was significant here, we adjusted for disaster exposure. Even after adjusting for exposure, previous disaster experience remained a significant risk factor for PTSD (odds ratio=6.34, 95% CI=1.70–23.61, p=0.006).
Exposed disaster workers with acute stress disorder were 7.33 times more likely to develop PTSD (95% CI=2.53–21.27, p<0.001). Exposed disaster workers who experienced early dissociative symptoms were no more likely to have PTSD at 13 months. However, the mean number of early dissociative symptoms of the 19 exposed disaster workers with PTSD was 2.95 (SD=1.7) compared to 1.77 (SD=1.3) in the 95 exposed disaster workers without PTSD (t=–3.43, df=112, p<0.001; odds ratio=1.82, 95% CI=1.25–2.66, p=0.002).
Exposed disaster workers who were depressed at 7 months were 9.5 times more likely to have PTSD at 13 months than those who were not depressed (95% CI=2.93–30.81, p<0.001). Of those exposed disaster workers with PTSD, slightly less than 50% also had comorbid depression. Exposed disaster workers who were depressed at 13 months were 7.96 times more likely to meet PTSD criteria (95% CI=2.72–23.26, p<0.001).
Exposed disaster workers with high exposure were more likely to have PTSD at 13 months (odds ratio=3.92, 95% CI=1.22–12.62, p=0.02). In particular, exposed disaster workers who assisted survivors were 2.98 times more likely to have PTSD than those who did not assist survivors (95% CI=1.04–8.51, p<0.05).
Because PTSD and depression are often comorbid and previous disaster experience may theoretically sensitize to future acute stress disorder (and was a risk factor here), we adjusted for previous disaster experience and depression at 7 months. Of importance, exposed disaster workers with acute stress disorder continued to be 6.96 times more likely to develop PTSD after adjustment for previous disaster experience and depression at 7 months (95% CI=1.75–27.68, p=0.006), while those with depression at 7 months were 5.4 times more likely to develop PTSD after adjustment for acute stress disorder and previous disaster experience (95% CI=1.39–20.96, p<0.02). Previous experience also remained a significant risk factor for PTSD (odds ratio=10.68, 95% CI=2.08–54.80, p=0.004) after adjustment for acute stress disorder and depression at 7 months.
Risk Factors for Depression in Exposed Disaster Workers
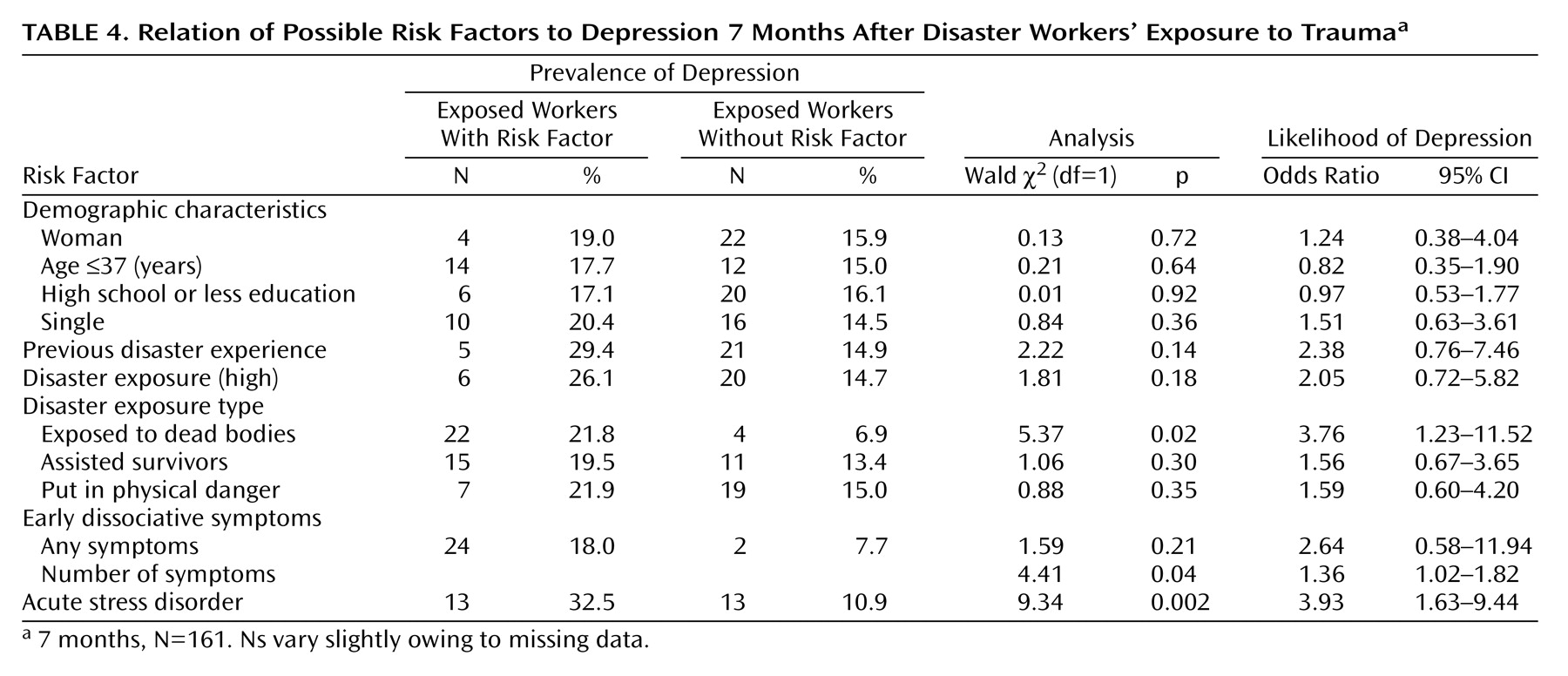
Depression at 7 months was not related to any demographic characteristic, previous disaster experience, or high exposure (
Table 4). Exposed disaster workers who had acute stress disorder were 3.93 times more likely to be depressed at 7 months than those without acute stress disorder (95% CI=1.63–9.44, p=0.002). Exposed disaster workers who experienced early dissociative symptoms were no more likely to have depression at 7 or 13 months than those who did not experience early dissociative symptoms. However, the greater the number of early dissociative symptoms, the greater the risk for depression at 7 months (odds ratio=1.36, 95% CI=1.02–1.82, p=0.04). The mean number of early dissociative symptoms of the 26 exposed disaster workers with depression at 7 months was 2.69 (SD=1.4) compared to 2.02 (SD=1.5) in the 133 exposed disaster workers without depression at 7 months (t=–2.15, df=157, p=0.03). Exposed disaster workers with high exposure were more likely to develop depression at 13 months (odds ratio=3.50, 95% CI=1.15–10.64, p=0.03).
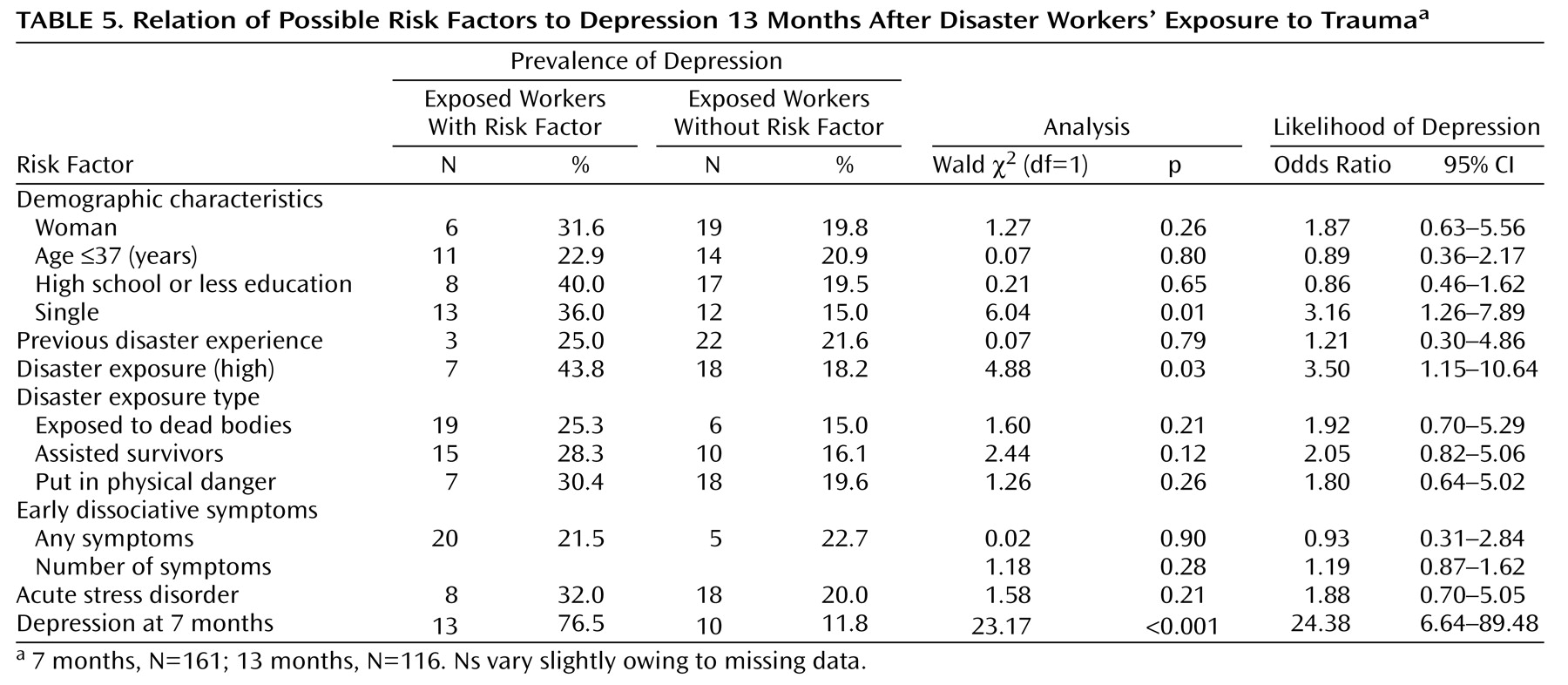
The risk for depression at 13 months was 3.16 times greater for those who were single compared to those who were married (95% CI=1.26–7.89, p<0.02) (
Table 5). Exposed disaster workers with depression at 7 months were 24.38 times more likely to have depression at 13 months than those without 7-month depression (odds ratio=24.38, 95% CI=6.64–89.48, p<0.001). Because marital status was significantly related to depression at 13 months, we also adjusted for marital status in analysis for risk factors for depression at 13 months. Reanalysis of risk factors for depression at 13 months after adjustment for marital status did not alter any results.
Health Care Utilization in Disaster Workers
During the 13 months after the crash, 15.1% (N=15) of exposed disaster workers compared to 4.0% (N=7) of the unexposed comparison subjects obtained medical care for emotional problems (χ2=10.45, df=1, p=0.001). Of the exposed disaster workers, 17.2% (N=17) reported needing any type of medical care (emotional or physical) but not obtaining any compared to 5.8% (N=10) of the comparison subjects (χ2=8.93, df=1, p=0.003). There were no differences between the exposed disaster workers and the unexposed comparison subjects on obtaining medical care for physical problems or annual physicals. Specifically, the exposed disaster workers were more likely to obtain medical care for emotional problems at each assessment point: at 2 months (N=13, 6.4%, versus N=5, 1.2%) (χ2=12.9, df=1, p<0.001), at 7 months (N=14, 9.0%, versus N=5, 1.8%) (χ2=11.84, df=1, p=0.001), and at 13 months (N=5, 4.4%, versus N=2, 1.0%) (χ2=3.86, df=1, p=0.05). More exposed disaster workers felt they needed medical care at 2 months (N=7, 3.5%, versus N=4, 1.0%) (χ2=4.75, df=1, p<0.03), but not at any other time.
Discussion
Disaster workers have infrequently been studied empirically
(19–
22). To our knowledge, there are no other large-scale longitudinal prospective studies of rescue and exposed disaster workers with a comparison sample that have examined acute stress disorder, PTSD, and depression. Our study indicates that exposed disaster workers are at an increased risk of acute stress disorder, PTSD, and depression. In addition, exposed disaster workers seek care for emotional problems at a rate nearly four times that of the comparison group. Nearly 40.5% of the exposed disaster workers in this 13-month study met criteria for at least one diagnosis.
Acute stress disorder has not previously been examined in disaster workers. The rates of acute stress disorder we found (25.6%) compare to the rates of acute stress disorder in motor vehicle accident survivors (13%)
(19) and in survivors of typhoons (7.2%)
(12). Although several studies of disaster workers have found that acute symptoms are predictive of posttraumatic stress symptoms
(10,
11), none has examined the association of acute stress disorder and PTSD. We found that exposed disaster workers with acute stress disorder were 7.33 times more likely to meet PTSD diagnostic criteria at 13 months. Approximately 42% of those with acute stress disorder developed PTSD. This compares with reports that 30.4% of those with acute stress disorder after a typhoon developed PTSD at 8 months
(12), and 78% of motor vehicle accident survivors diagnosed with acute stress disorder met criteria for PTSD 6 months after their accident
(23).
The rates of PTSD we found (16.7%) are similar to the rates of PTSD found by McFarlane and Papay
(24) in firefighters exposed to a bushfire (12.5%). Approximately 34% of the people exposed to the Oklahoma City bombing developed PTSD 6 months after the disaster
(25), while the rates of PTSD after a tornado and a flood were 15% at 4 months and 21% at 16 months
(26). Women have generally been found to have higher rates of PTSD
(27,
28). However, our sample had a relatively small number of women, which may explain why we found no gender differences in the rates of PTSD.
The increased rate of depression at 7 months (16%) and the even higher rate at 13 months (21.7%) indicate the importance of this diagnosis to health care planning for disaster workers. Few well-designed studies have examined depression after a traumatic event, particularly in rescue or disaster workers. Approximately 8.5% of firefighters exposed to a bush fire met criteria for depression at 42 months
(24). Nearly 23% of the individuals directly exposed to the Oklahoma City terrorist bombing had major depression at 6 months
(25).
Exposed disaster workers with more early dissociative symptoms were at greater risk for PTSD and depression at 7 months. Early dissociative symptoms have been found to be predictive of PTSD
(10,
29) but have not previously been reported as a predictor of depression. Identification of early dissociative symptoms may identify individuals for early pharmacological or behavioral interventions. The neurobiology of early dissociative symptoms and their relationship to depression and PTSD require further study
(30,
31).
The contribution of previous experience with disasters to future risk is of particular importance for occupational groups repeatedly exposed to disasters (e.g., police, firefighters). Whether previous disaster experience sensitizes or inoculates against future risk is a complex issue that has implications for training. In addition, sensitization versus inoculation may be important to unsuccessful versus successful coping after trauma and to the possible development of PTSD. Further study is needed. Our results indicate that exposed disaster workers with previous disaster experience are 6.77 times more likely to develop PTSD. Previous disaster experience is a complex variable that includes previous trauma exposure, training opportunities, and the possibility of past PTSD
(32). Our findings are consistent with other evidence that previous disaster exposure predisposes to the development of acute stress disorder
(33) and PTSD
(34,
35). Several recent studies of nonprofessionals exposed to traumatic events have shown that previous PTSD, but not past trauma alone, may be the critical variable predicting PTSD after a new trauma exposure
(36,
37).
Several important limitations should be considered in interpreting the results of our study. A larger number of subjects would have been preferable in order to increase confidence in our results. Although we used self-reports to assess both predictor and outcome variables and did not have lifetime diagnoses, we used validated scales and scale items and a well-matched comparison group. Recall is a difficulty for the measure of acute stress disorder and early dissociative symptoms. Rates may have been influenced by recall bias. However, the direction of any possible recall bias is not known. Those with higher symptoms at 2 months may recall more symptoms, and alternatively, exposed disaster workers may minimize recall of symptoms. In order to generalize our findings to other disaster populations, a more diverse sample allowing for examination of other possible contributions of demographic variables would also have been preferable. With these limitations in mind, health care planning for disaster workers should address the exposed disaster workers’ increased risk of acute stress disorder, PTSD, and depression. Further study of mental health care needs of disaster workers and other first responders is needed.