Evaluation of specific versus generalized cognitive deficits in schizophrenia remains a challenge
(1,
2), but deficits in particular domains can suggest candidate endophenotypes to assist in gene identification. Patients with schizophrenia are impaired in facial recognition
(3), implicating frontotemporal circuits
(4), but whether this reflects a generalized memory deficit is unclear. Conklin et al.
(5) reported that 33 healthy first-degree relatives of patients with schizophrenia were also impaired in face memory (according to Wechsler Memory Scale, 3rd ed., scores) compared with 56 healthy subjects. Impairment in relatives suggests that observed deficits in patients might be associated with genetic susceptibility and not attributable to confounding effects of chronic illness. In the study by Conklin et al., face recognition deficits were not accounted for by verbal memory and spatial attention deficits, but a more generalized nonverbal object memory deficit was not assessed. Lesion and neuroimaging studies suggest separate processing nodes for faces and other nonverbal objects. To shed light on this phenomenon, we evaluated both face recognition memory and visual object memory in patients, their relatives, and healthy subjects.
Results
Distributions of Penn Face Memory Test and Visual Object Learning Test scores departed from normality (Kolmogorov-Smirnov p<0.01). Dependent variables were therefore converted to percent correct, arc-sine transformed, and converted to z scores by using healthy group data.
Analysis of variance (ANOVA) revealed that patients and their relatives were older than comparison subjects (F=42.9, df=2, 295, p<0.001). Therefore, age was addressed in subsequent analyses. Sex was balanced across groups, although there was a trend toward disproportion (χ2=4.98, df=1, p=0.08). Follow-up chi-square tests revealed a similar number of men and women in the group of relatives and the healthy comparison group (χ2=0.02, df=1, n.s.) but a disproportionate number of men in the patient group (χ2=7.50, df=1, p<0.01). Subsequent analyses considered the influence of gender among patients.
Parental education did not differ among groups (F=0.75, df=2, 256, p=0.47), and handedness was equally distributed (χ2=2.93, df=4, p=0.57). BPRS scores were not correlated with Penn Face Memory Test or Visual Object Learning Test scores (p>0.06). These variables were not considered further.
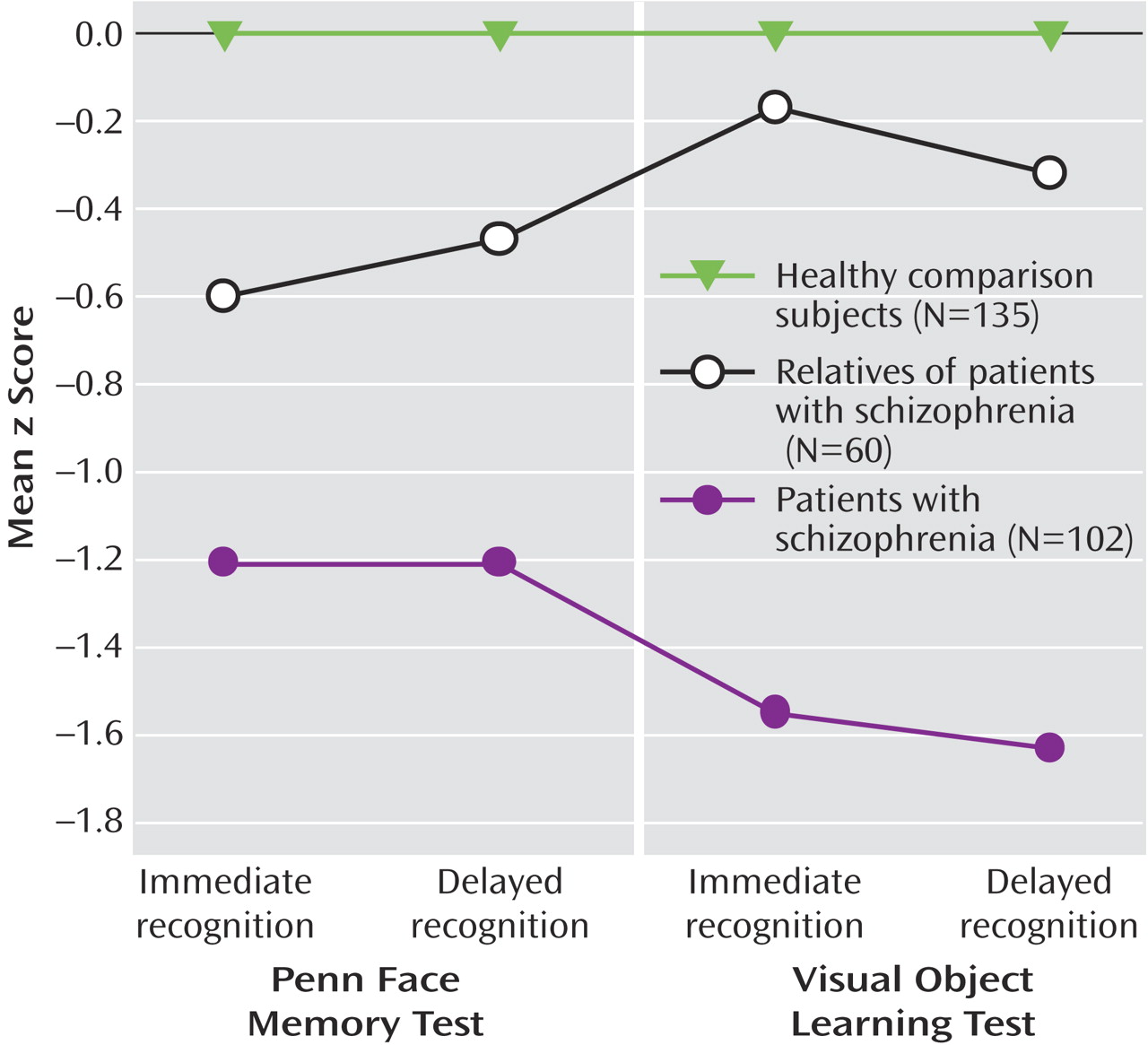
Repeated-measures ANOVA, with Penn Face Memory Test (immediate and delayed) as the within-subjects factor and group (schizophrenia, relative, or comparison) as the between-subjects factor showed a main effect of group (F=46.47, df=2, 293, p<0.001) and no group-by-measure interaction (F=0.24, df=2, 293, p=0.47). Follow-up one-way ANOVAs and post hoc tests (Tukey’s least significant difference) were performed to identify sources of the group effect. Patients recognized fewer faces than healthy subjects in both immediate and delay conditions (
Figure 1). Relatives recognized fewer faces than healthy subjects and more faces than patients in both conditions. There were no differences in performance between immediate and delayed recognition on the Penn Face Memory Test; patients and relatives were more impaired than healthy subjects in both immediate and delayed face memory. Results were similar for the Visual Object Learning Test (F=46.41, df=2, 161, p<0.001), but in follow-up tests, relatives did not differ from comparison subjects.
Analysis of covariance (ANCOVA) revealed age as a significant covariate (p<0.01), but pairwise ANCOVAs between relatives and healthy comparison subjects yielded the same results as those shown in
Figure 1. Moreover, in both patients and relatives, correlations between face memory and age were small and nonsignificant. Correlations were significant but small in the comparison group (r=–0.24, N=135, p<0.005, for immediate recognition; r=–0.20, N=135, p<0.05, for delayed recognition), accounting at most for 4% of the variance. Thus, ANCOVA and correlation analyses suggest that the deficit in relatives was not attributable to age differences.
Because some relatives had conditions for which comparison subjects were excluded, data were reanalyzed with only the medically and psychiatrically healthy relatives, age ≤65 years (N=28). Results were unaltered. Because some patients and relatives came from the same families, some observations are not independent. We repeated the analyses comparing relatives and comparison subjects with one relative per family (closest in age to the patient) (N=35); again, results were unchanged. Finally, we conducted within-participant group t tests using sex as a grouping variable. Men and women did not differ, indicating that the preponderance of men did not account for impairment in schizophrenia.
To assess the robustness of the face memory deficit, we conducted receiver-operating-curve analyses, which provide an index of sensitivity and specificity. The area under the curve value indicates the ability of a measure (face memory) to differentiate between two groups (1.0=perfect discriminability, 0.5=groups overlap completely). Relative to healthy subjects, area under the curve values were highly significant for measures of face memory in patients (area under the curve=0.78, SE=0.03, p<0.001, for immediate recognition; area under the curve=0.77, SE=0.03, p<0.001, for delayed recognition) and relatives (area under the curve=0.69, SE=0.04, p<0.001, for immediate recognition; area under the curve=0.65, SE=0.04, p<0.002, for delayed recognition). Thus, both immediate and delayed face memory robustly differentiate patients with schizophrenia and their relatives from healthy people.
We used Pearson bivariate correlation coefficients to assess relationships among the four dependent variables. With two exceptions, correlations were similar within each group and were moderate (r=0.30–0.67, all p<0.05). Correlations were small and nonsignificant between Penn Face Memory Test immediate recognition and Visual Object Learning Test delayed recognition in comparison subjects (r=0.21) and between Penn Face Memory Test delayed recognition and Visual Object Learning Test immediate recognition in relatives (r=0.27).